Problem List
advertisement
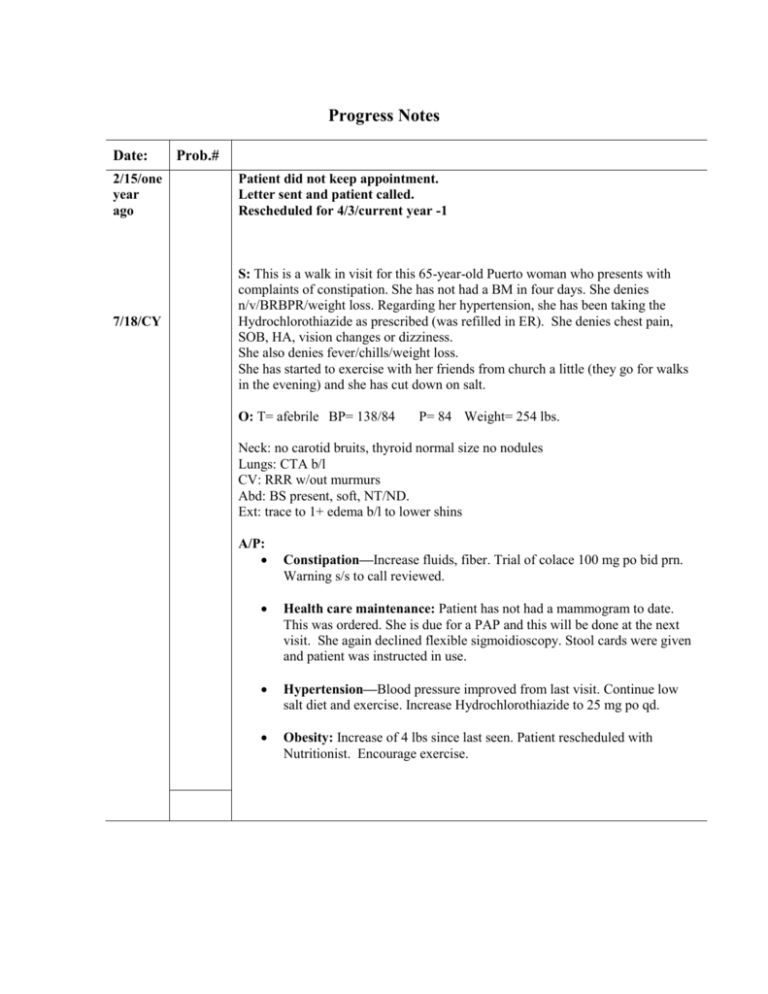
Progress Notes Date: 2/15/one year ago 7/18/CY Prob.# Patient did not keep appointment. Letter sent and patient called. Rescheduled for 4/3/current year -1 S: This is a walk in visit for this 65-year-old Puerto woman who presents with complaints of constipation. She has not had a BM in four days. She denies n/v/BRBPR/weight loss. Regarding her hypertension, she has been taking the Hydrochlorothiazide as prescribed (was refilled in ER). She denies chest pain, SOB, HA, vision changes or dizziness. She also denies fever/chills/weight loss. She has started to exercise with her friends from church a little (they go for walks in the evening) and she has cut down on salt. O: T= afebrile BP= 138/84 P= 84 Weight= 254 lbs. Neck: no carotid bruits, thyroid normal size no nodules Lungs: CTA b/l CV: RRR w/out murmurs Abd: BS present, soft, NT/ND. Ext: trace to 1+ edema b/l to lower shins A/P: Constipation—Increase fluids, fiber. Trial of colace 100 mg po bid prn. Warning s/s to call reviewed. Health care maintenance: Patient has not had a mammogram to date. This was ordered. She is due for a PAP and this will be done at the next visit. She again declined flexible sigmoidioscopy. Stool cards were given and patient was instructed in use. Hypertension—Blood pressure improved from last visit. Continue low salt diet and exercise. Increase Hydrochlorothiazide to 25 mg po qd. Obesity: Increase of 4 lbs since last seen. Patient rescheduled with Nutritionist. Encourage exercise. Progress Notes Date: 10/5/11 yrs ago 12/5/11 yrs ago 12/20/C Y-2 Prob.# Patient did not keep appointment. Letter sent and patient called. Rescheduled for 12/5/current year -11 Patient did not keep appointment. Daughter notified clinic that patient has gone back to Puerto Rico. S: This is an acute care visit for this 63-year-old woman who presents with complaints of b/l lower extremity edema. She has not been seen in Family Medicine in approximately 9 years. She denies chest pain, SOB, PND, orthopnea, or dyspnea on exertion. She also denies fever/chills/redness/warmth. She is also here for f/u of her blood pressure. She denies headache or vision changes as well. She continues to eat a high salt diet. O: T= afebrile BP= 144/96 P= 80 Weight= 250 lbs. Neck: no carotid bruits, thyroid normal size no nodules Lungs: CTA b/l CV: RRR w/out murmurs Abd: BS present, soft, NT/ND. Ext: trace to 1+ edema b/l to lower shins A/P: Health care maintenance: Patient has not had mammogram to date. This was ordered. Td, Pneumovax, and Flu shots were given today. Hypertension—patient has had two BP elevations >140/90. has not been successful with decreased salt intake and dietary management. Not currently engaged in active exercise program. Will start trial of Hydrochlorothiazide 12.5 mg po qd which should also help with venous stasis. Venous stasis--TED stockings, elevate legs, decrease salt intake, and hydrochlorothiazide as above. Obesity: Encourage continued work with nutrition and exercise. Follow up for BP check in 1 month. Progress Notes Date 8/4/11 yrs ago Prob# S: This is the first Family Medicine visit for this 54-year-old Puerto Rican woman. She has a past medical history significant for osteoarthritis, borderline blood pressures, and occasional headaches. She just moved from Puerto Rico and is transferring her medical care to Family Medicine. She presents with her medical records from Puerto Rico for a health care maintenance visit. The patient is without medical complaints at this time. She has not had a PAP smear or physical in over 7 years. In terms of her osteoarthritis, she describes pain in b/l knees that is worse later in the day and also worse in rainy weather. She denies h/o swelling, redness, warmth, or fever. She denies any h/o recent or previous injury. She also has low back pain off and on and was told in the past that this was from “age”. Her knee pain is usually relieved with one or two doses of 800mgs Ibuprofen per day. Her record is reviewed, showing cholesterol drawn two years ago (fasting) of 210, HDL 46, TG 173, blood sugar was 112. Casimira has a number of blood pressures in the past medical record with diastolics in the 84-92 range, and systolics from about 138 to as high as 148. The patient notes that she was recommended to "cut back on salt". Social: The patient moved from Puerto Rico to New York City at age 15. She went back to Puerto Rico with her husband and just recently returned to the United States with her children. She completed high school. She describes her relationship with her husband as good. She denies domestic violence or abuse. Couple is sexually active. She lives with her daughter on the second floor of a house in Jamaica Plain. Substance Abuse history: Denies tobacco, alcohol or drug use, past or present. GYN history: Patient’s menses stopped 7 years ago and she has had no vaginal bleeding since that time. She has no sexual difficulties. No urinary incontinence. Last PAP smear was over 7 years ago. Medications: Ibuprofen, 600-800 mgs one or two times a week prn knee pain or headache. Allergies: PCN rash. Review of systems: Non contributory. O: Physical Exam: She is in no acute distress. Blood pressure: 142/92. Weight: 246 lbs. Height: 5'3". Pulse: 84 regular. Neck: supple, there is no lymphadenopathy, no thyromegaly, TMs are clear, Eyes: pupils round and equally reactive to light; extraocular movements intact Pharynx: clear, no masses, no tongue lesions, dentition good Lungs: clear all fields Heart: regular rate and rhythm without rubs, murmurs or gallops. Breast: examined seated and supine, no masses felt in either position, no asymmetries, no skin changes, no nipple discharge, no axillary, supraclavicular, infraclavicular lymphadenopathy. Abdomen: obese, normo-active bowel sounds, no organomegaly. Pelvic: Ext genitalia normal, no lesions, Vagina normal no lesions/discharge, Cervix, no lesions/discharge, Bi-manual exam normal size uterus and adnexa, no CMT or adnexal/uterine tenderness Extremities: no gross deformities, full ROM. Skin: no abnormal pigmented lesions. Neurological: alert and oriented x 3, cranial nerves grossly intact, LT and PP intact in all extremities; discs flat, rhomberg negative, f-n intact, gait normal. Vascular: peripheral pulses are 2+ throughout A/P: Health care maintenance – Physical/PAP/GC/chl done. She has her immunization record at home and will bring this next visit. Mammogram booked. Discussed flexible sigmoidoscopy for cancer screening and patient declined. Stool guiacs given. Random glu, fasting lipid panel. Obesity - We discussed strategies for a gradual weight loss through permanent modification of diet rather than dieting. I suggest referral for nutritionist and she agrees. She will try to start exercising 3 times/week by walking for a half hour. Osteoarthritis—Continue Motrin for now, as this appears to be working. Motrin 800 mg po tid prn with food. Elevated Blood pressure- Lower salt intake. Increase exercise as above. Weight management as above. Follow up for blood pressure check in 2 months.