DVT Prophylaxis
advertisement

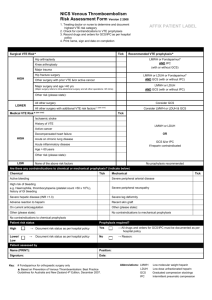
A. GENERAL GUIDELINE OF VTE PROPHYLAXIS Clinical judgment should always be used in utilizing the guideline. References: a. b. c. d. AAOS Clinical Guideline (Prevention of Symptomatic Pulmonary Embolism Guideline 2007) MedQIC-Surgical Care Improvement Project. Specifications Manual for National Hospital Inpatient Quality Measures. Discharges 10-01-08 (4Q08) through 03-31-09 (1Q09) Prevention of venous thromboembolism: ACCP Evidence-Based Clinical Practice Guidelines (8th edition) Chest 2008;133(6):381S-453S Regional Anesthesia in the Anticoagulated patient: Defining the Risks (The Second American Society of Regional Anesthesia Consensus Conference on Neuraxial Anesthesia and Anticoagulation). Reg Aesth Pain Med 2003;28:172-197. Abbreviations: - Sequential Compression devices (SCD) - Arterial Venous Impulse Boots (AVI) - Low-dose unfractionated heparin (LDUH) - Low molecular weight heparin (LMWH) - Central Venous Catheter (CVC) 1. Risk factor stratification is based on individual predisposing factors and the risk associated with current illness or procedure 2. Mechanical Methods of Prophylaxis SCD or AVI alone or in combination with aspirin in orthopedic surgery patients with documented high risk of bleeding is recommended SCD or AVI as an adjunct to anticoagulant-based prophylaxis Ensure correct size and application of the mechanical device, and optimal compliance 3. Neuraxial anesthesia/analgesia (NAA) [spinal or epidural anesthesia and continuous epidural anesthesia] Avoid neuraxial anesthesia/analgesia (NAA) in patients with a known bleeding disorder Avoid NAA in patients whose preoperative hemostasis is impaired by antithrombotic drugs a. NSAID (generally safe) b. Clopidogrel should be discontinued 5-14 days prior to NAA Needle insertion: at least 8-12 hours after a subcutaneous (SubQ) dose of unfractionated heparin (UFH) or a twice daily prophylactic dose of low molecular weight heparin (LMWH), or at least 18 hours after a once-daily dose of LMWH Needle removal: Remove an epidural catheter when the anticoagulant effect is at a minimum just before the next scheduled SubQ injection Delay anticoagulant prophylaxis for at least 2 hours after spinal needle or epidural catheter removal Delay anticoagulation if a hemorrhagic aspirate is encountered during the initial spinal needle placement If on prophylaxis with warfarin, remove a catheter when INR <1.5 Fondaparinux prophylaxis appears to be safe in patients who have received a spinal anesthetic only if needle placement was atraumatic and accomplished on the first attempt, but should be avoided with continuous epidural analgesia B. VENOUS THROMBOEMOLISM RISK ASSESSMENT Acute medical illness Age >65 Cancer (active or occult) Cancer therapy (hormonal, chemo- or radiotherapy, angiogenesis inhibitors) Estrogen-based OC or HRT Erythropoiesis-stimulating agents Immobility, lower-extremity paresis Indwelling central venous catheter Inflammatory bowel disease Inherited or acquired thrombophilia Myeloproliferative disorders Nephrotic syndrome Obesity Paroxysmal nocturnal hemoglobinuria Pregnancy and post-partum period Previous VTE Selective estrogen receptor modulators Surgery Trauma (major or lower extremity) Venous compression (tumor, hematoma, arterial abnormality This is not a permanent part of the medical record. Please discard after completing form. C. VTE Prophylaxis Selection by Surgery 1 Patients who receive neuraxial anesthesia or have a documented contraindication to pharmacological prophylaxis may pass the performance measure if either appropriate pharmacologic prophylaxis or mechanical prophylaxis is ordered. 2Recommendations are from the Specifications Manual for National Hospital Quality Measures 10-01-08 (4Q08) through 0331-09 (1Q09) SCIP-VTE 2-5. AAOS refers to the SCIP Guidelines for patients with high risk of bleeding. Surgery Recommended Prophylaxis1 Surgery Recommended Prophylaxis1 Intracranial Neurosurgery Any of the following: SCD with LDUH LMWH LDUH or LMWH* combined with SCD *Current guidelines recommend postoperative LMWH for Intracranial Neurosurgery Elective Total Hip Replacement Any of the following: LMWH Fondaparinux Warfarin Elective Total Hip Replacement with contraindications to pharmacological prophylaxis Any of the following: SCD AVI Any one of the above plus aspirin2 Elective Total Knee Replacement Any of the following: LMWH Fondaparinux Warfarin SCD VFP General Surgery General Surgery with high risk for bleeding Gynecologic Surgery Urologic Surgery Any of the following: LDUH LMWH Fondaparinux LDUH or LMWH or Fondaparinux combined with SCD Any of the following: SCD Any of the following: LDUH LMWH Fondaparinux SCD LDUH or LMWH or Fondaparinux combined with SCD Any of the following: LDUH LMWH Fondaparinux SCD LDUH or LMWH or Fondaparinux combined with SCD Abbreviations: - Sequential Compression devices (SCD) - Arterial Venous Impulse Boots (AVI) Hip Fracture Surgery Hip Fracture Surgery with contraindications to pharmacological prophylaxis Any of the following: LDUH LMWH Fondaparinux Warfarin Any of the following: SCD AVI Any one of the above plus aspirin2 - Low-dose unfractionated heparin (LDUH) - Low molecular weight heparin (LMWH) - Central Venous Catheter (CVC) This is not a permanent part of the medical record. Please discard after completing form. Adult VTE Risk Assessment and Physician Order Physician: Please check risk factor(s) below and order prophylaxis. Acute medical illness Age >65 Cancer (active or occult) Cancer therapy (hormonal, chemo- or radio-therapy, angiogenesis inhibitors) Estrogen-based OC or HRT Erythropoiesis-stimulating agents Inherited or acquired thrombophilia Immobility, lower-extremity paresis Indwelling central venous catheter Inflammatory bowel disease Myeloproliferative disorder Nephrotic syndrome Obesity Paroxysmal nocturnal hemoglobinuria Pregnancy or post-partum period Previous VTE Selective estrogen receptor modulators Surgery Trauma (major or lower extremity) Venous compression (Tumor, hematoma, arterial abnormality Pharmacological and Mechanical Prophylaxis Safety Assessment (Physician to check those that apply) Pharmacological Prophylaxis Contraindication(s): Is patient experiencing any active bleeding? Does patient have (or has had history of) heparin-induced thrombocytopenia? Is patient’s platelet count <100,0003/mm? Is patient already on anticoagulant therapy (warfarin, heparin, LMWH, or fondaparinux)? Is patient’s creatinine clearance abnormal (<30 ml/min)? Fondaparinux is contraindicated. Other: If any of the above boxes are checked, the patient may not be a candidate for anticoagulant therapy. Consider alternative prophylactic measures (mechanical prophylaxis) in Section B below. B. Mechanical Prophylaxis Contraindications(s): Does patient have severe peripheral arterial disease? Does patient have congestive heart failure (peripheral edema)? Does patient have an acute superficial/deep vein thrombosis? Does patient have skin conditions (dermatitis, open skin lesions, gangrenous condition, or lymphedema)? Other: If any of the above boxes are checked, then patient may not be a candidate for a sequential compression device. Post-Op Physician’s Order (please check one): Prophylaxis is not indicated as checked above or other reason ___________________________________ ________________________________________________________________________________ Prophylaxis has already been ordered Place SCD (Sequential Compression Device) or AVI (Arterial Venous Impulse Boots) AND Aspirin 325 mg ______ daily For all post op surgical patients, start the first dose on the morning of POD one or as indicated below. Enoxaparin 40 mg SubQ daily, first dose at ___________. Pharmacy to adjust the dose, if CrCl < 30 ml/min. Enoxaparin 30 mg SubQ twice daily, first dose at ___________. Pharmacy to adjust the dose, if CrCl < 30 ml/min. Fondaparinux 2.5 mg SubQ daily, first dose at ___________. (contraindicated, if CrCl < 30 ml/min) Unfractionated heparin 5000 units every 8 hours, first dose at ___________. Warfarin ________ mg PO, first dose at ___________ and daily (until INR ______) and daily INR Physician Signature *0940770* ID Date Adult VTE Risk Assessment & Physician Orders Trial Form Time