Controlling Healthcare Spending on Medical Imaging: Paging Dr
advertisement

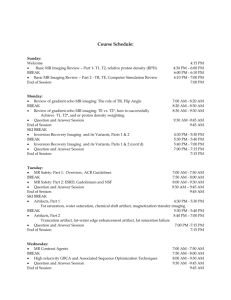
Controlling Healthcare Spending on Medical Imaging: Paging Dr. Bayes Timothy F Christian, MD, MPA The Mossaver-Rahmani Center for Business and Government Harvard Kennedy School Harvard University, Cambridge, MA Address Timothy F Christian, MD, MPA The Mossaver-Rahmani Center for Business and Government Harvard Kennedy School/ 5 Belfer 79 JFK Street Cambridge, MA 02138 Timothy_christian@hks.harvard.edu Medicine is a science of uncertainty and an art of probability -Sir William Osler Spending on medical imaging has doubled since 2000. In a single year, imaging costs accounted for 27% of the increase in overall healthcare costs (1,2). This rapid increase cuts across public, private and managed health care systems (1). Imaging has come into focus politically. As imagers working in dark rooms, such notoriety is novel but also most disturbing. The Admistration’s budget for 2012 calls for across the board cuts in imaging spending and implementation of broad prior-authorization program for Medicare patients. The savings of this approach is a modest $820 million dollar reduction in spending and a probable dose of provider resentment. Others would like to put imaging under the microscope of cost-effective or cost utility analyses by the new Patient-Centered Outcomes Research Institute created by the Affordable Care Act (3). The current increases in healthcare spending are unsustainable, as the true cost has been buried within deficit spending. But neither broad reductions in reimbursement and access nor cost effective analyses studies are likely to be effective for the imaging problem. There is a better, simpler approach. Cost effective analyses work well for therapies because outcomes are directly linked to the therapy. For example, there have been excellent studies (4,5) examining the cost effectiveness of coronary bypass surgery against coronary angioplasty, the latter being a far less invasive approach to relieving obstructed arteries in the heart. There are objective outcomes: survival, relief of anginal chest pain, and functionality. Quality of life questionaires (the heart of the utility analysis), reveal that quality of life is superior for angioplasty in the first month, as surgical patients have recovering wounds but this advantage evens out by 6 months. We also see that diabetic patients have improved survival with bypass, so there is variability in the response depending on patient group. CEA and CUA are thus quite effective as tools to compare and contrast therapies. But medical imaging is quite different (6). There is no direct outcome to measure because survival, quality of life, symptom relief, all come from a therapy, not the diagnosis. Therapies can vary widely. In the case of coronary artery disease it can take the form of medication, exercise programs, angioplasty, bypass surgery or nothing. The imaging outcome cannot dictate the therapy. The final decision to apply a therapy is the result of a chain of information which starts with a conversation and an exam. Imaging is an intermediary step. The only way to isolate the imaging portion of this chain is to hold the therapy constant, which is not medically feasible. But what about quality of life measures (often assessed as quality adjusted life years or the QALY)? Lets take an example. Many people have anxiety toward heart disease because of its silent, common and sudden nature. Pressure for screening is fairly high, but, even more so than most diseases, there are risk factors that are known to predispose one to the condition. In the absence of these, screening (say in the form of stress test imaging) is not indicated because the pre-imaging risk is so low that almost all the results performed on such patients will be normal. The QALY does not uncover this. Since having coronary heart disease is a negative good, a person’s QALY goes up with a negative test! It was an inappropriate use of imaging but as far as doctor and patient are concerned, it is a win-win strategy. The QALY is misleading in this common example. The test will also analyze favorable in terms of outcomes because it will predict no events, and due to the low pre-test risk of the patient, no events is what the analysis will show. Which brings us to back to what imagers have known for many years: the performance and utility of an imaging test is a function of its inherent accuracy as well as the prevalence of disease in the population being tested. This is Bayes Theorem. Additional information has the greatest impact when uncertainty is highest. This is graphically displayed in figure 1. The function of the clinical history and exam is to take the probability of the presence or absence of disease from a flip of a coin to a greater certainty. If the pre-test probability on this first go-round is very low, then nothing more should be done. If high, then definitive diagnosis and therapy should be sought. But often the history and physical leave the probability in the intermediate zone, where further information is needed. Just what constitutes low, high and intermediate probability are a function of the potential risk of the disease. Consequently, a coronary artery disease question has higher stakes than the etiology of low back pain. But the principles remain the same: Most of the potential incremental information of imaging and thus the value for money of the test will lie in the intermediate group. How much value depends on the accuracy of the test. Imaging modalities of CT, MRI, and PET imaging generally afford better overall accuracy (at a price) but no imaging test will provide much value for money in either the very low or high-risk groups (see figure 2). Then how are we to control the rising costs of medical imaging? There are many forces that contribute to this rise. These include better imaging technology and resolution. How many of us would like to go back to earliest models of mobile phones, even though they would be much cheaper and provide the basics (which used to be voice communication)? Patients have come to expect a definitive answer to their concerns and imaging offers this. Imaging provides a bump up in reimbursement for office visits. In the face of declining payouts overall, this is a driver. Imaging buys reassurance for physicians against malpractice claims. Finally, imaging is incredibly powerful in diagnosing pathology. These are all potent forces so an equally potent solution is required to counter. The most straight-forward solution is to tie reimbursement for imaging, either on the provider side or consumer side, to the pre-test probability of the disease in question. Virtually all imaging modalities have appropriateness critieria agreed upon by expert physicians (8,9). These are evidence-based and published. For example, for nuclear stress imaging, detailed appropriateness criteria for patients based on symptoms, other tests in hand, and risk factors have been carefully worked out (10). All of them recommend against imaging very low pre-test risk patients. These panels have decades of outcomes research publications to draw from. New trials confirming these facts are not needed. What is needed is to give these criteria teeth. By weighting reimbursement to the appropriateness classification, there will be a driving incentive to keep imaging centered on the intermediate risk populations, where it needs to be. Tying malpractice reform to this incentive-based strategy will be critical. References 1. Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Affairs 2008; 27: 1491-1502. 2. MedPAC. A Data Book; Health Care Spending and the Medicare Program. 3. The Institute of the National Academies. 100 Initial Priority Topics for Comparative Effectiveness Research. 2009 4. Hlatky MA, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet 2009; 373: 1190-1197. 5. Garber AM. How the Patient-Centered Outcomes Research Institute can best influence real-world healthcare decision making. Health Affairs 2011; 30: 22432251. 6. Tatsioni A, Zarin DA, Aronson N, Samson BA, Flamm CR, Schmid C, Lau J. Challenges in Systematic Reviews of Diagnostic Technologies. Ann Intern Med 2005; 142: 1048-1055. 7. Grundy SM, Pasternak R, Greenland P, et al. AHA/ACC scientific statement: assessment of cardiovascular risk by use of multiple-risk factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol. 1999;34:1348 –59. 8. Patel MR, Spertus JA, Brindis RG, Hendel RC, Douglas PS, Peterson ED, Wolk MJ, Allen JM, Raskin IE. ACCF Proposed Method for Evaluating the Appropriateness of Cardiovascular Imaging. J Am Coll Cardiol 2005; 46:1606-1615. 9. Sistrom CL. The Appropriateness of Imaging: A Comprehensive Conceptual Framework. June 2009 Radiology, 251, 637-649. 10. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging. ASNC 2009. Figure 1 Figure 1 Bayes theorem graphically represented. Individual pre-test probability (x-axis) is plotted against the post-imaging test probability of the disease in question. Dashed line=identity (no added value). In this type of analysis, it is assumed that the pre-test probability is a reflection of the prevalence of disease in that patient probability classification. The degree of convexity of the positive result and negative result curves increase as the sensitivity and specificity of the test increase. This curve approximates a test with 90% sensitivity and 80% specificity, which is an approximation of stress testing with imaging. Note that at 50% pre-test probability (A), the gain in information regarding disease probability is maximal (a positive test increases the likelihood of disease from 50 to 85% certainty). For low risk patients (B) where presence of disease is rare, neither a positive nor a negative test result moves a patient out of the low probability range. This is because nearly all the positive responders in this range are false positives. The rate of false positive do not change based on prevalence. Figure 2 Figure 2: Comparison of two tests of different accuracy and cost for the detection of coronary artery disease. Nuclear stress imaging (black lines) is portrayed with a sensitivity of 90% and specificity of 80% while exercise testing without imaging (approximately 4-5-fold less expensive) is assumed to have a sensitivity of 70% and specificity of 60%. At low prevalence (arrows) there is still minimal added value with a positive or negative result independent of cost. The cost portion of the analysis is more favorable, but the value of the information is unchanged. Consequently, simply substituting a less expensive test in low-risk patients has limited justification.