Micro Chapter 23 [4-20
advertisement
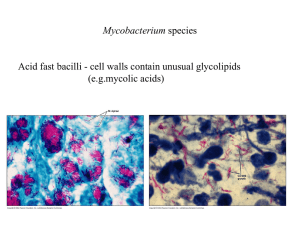
Micro Chapter 23: Tuberculosis and Leprosy (Mycobacteria) Tuberculosis is caused by mycobacterium tuberculosis Worldwide, TB is second only to HIV in deaths caused by a single infectious agent Most immunocompetent people who get infected with M. tuberculosis, will never become ill Mycobacterium are a family of obligate aerobes Mycobacteria that don’t cause TB are called atypical mycobacteria Many mycobacteria are harmless, and some live on the human body without causing disease Mycobacteria are unique in that they stain acid fast, are resistant to drying, and grow slowly Mycobacteria are unique in that they stain acid fast: - The mycobacterial envelope has waxes made of long-chain hydrocarbons The most abundant wax, mycolic acid, gives it its staining characteristic o Mycobacter actually means – bacteria with mycolic acid The waxy mycolic acid barrier decreases permeability to many molecules, including gram stain, so mycobacteria are neither gram positive or gram negative The only way to stain mycobacteria is to heat them with a red dye called fuchsin, then treat them with HCl o This removes every organism but mycobacteria, so they are acid fast o The mycobacteria will look like slender red rods o Fluorochrome dyes are used more often than fuchsin now since they’re easier to use with fluorescence The waxy coat of mycolic acid makes M. tuberculosis resistant to drying and chemicals, helping them survive in and out of the body - Mycobacteria are surprisingly resistant to killing by phagocytes The resistance to drying makes mycobacteria good at airborne transmission The mycolic waxy coat doesn’t protect from heat though Mycobacteria grow much slower than most bacterial pathogens - Slow growth can delay diagnosis by culturing So if a patient had a culture test positive for acid fast for mycobacteria and started meds for it, it could take weeks before they know if those meds work on that mycobacteria Tuberculosis is now rare in the US, and half of all cases here are from foreign-borne people M. tuberculosis infects 1/3 of the world’s population To spread rapidly, M. tuberculosis prefers crowded living conditions in a population with little resistance to it Half of people in Africa with AIDS, also have TB, and 1/3 of AIDS deaths are from TB - Nearly all people coinfected with HIV and M. Tuberculosis will eventually develop TB People with AIDS are more prone to reactivating infection, and for rapid progression of acute infection TB will cause widespread extrapulmonary disease in AIDS patients People with AIDS are also very susceptible to Mycobacterium avium complex (MAC), found in water and soil, and usually harmless to immunocompetent people o It was rare before AIDS, but in AIDS patients it can colonize the GI and spread o Symptoms include fever, malaise, and wasting, diarrhea, abdominal pain Almost all TB infections result from inhaling infectious mycoplasma particles that were aerosolized by coughing, sneezing, or talking - The initial source of infection is the lung These droplet nuclei dry while airborne, and can remain in the air for hours, and then get inhaled Coughing, sneezing, and talking for several minutes, can produce thousands of droplet nuclei Air in the room occupied by a person with pulmonary TB may remain infectious even after the person has left the room! Fortunately, prolonged exposure and multiple aerosol incoula are usually required to establish an infection Brief contact carries little risk, and infection rarely happens outdoors, because UV light kills M. tuberculosis Large drops of respiratory secretions, or contaminated inanimate objects, rarely cause transmission of TB Reasons airborne spread of TB is efficient for infection: - - Host inflammatory response to TB creates open lung lesions called pulmonary cavities, that have large #’s of organisms o Coughing spreads the organisms from such a lesion into the air The small size of droplet nuclei is also ideal for bypassing the mucociliary lining of large airways, to get to the alveoli Symptoms of TB are mainly caused by the host immune response - Damage is caused by chronic inflammation and survival of organisms in macrophage Primary infection by TB: - Airborne droplet nuclei reach the alveoli, where multiplication begins - - - - - - o This is usually in the middle lung zone, where airflow is greatest In the middle lung zone, the M. tuberculosis is ingested by alveolar macrophage o They only get rid of a few of the organisms though Instead, M. tuberculosis multiplies basically unimpeded, and actually destroys the alveolar macrophage M. tuberculosis is a facultative intracellular pathogen – means it can multiply both inside of and outside of cells At this point, lymphocytes and monocytes come from the blood to get the M. tuberculosis, and macrophage ingest it o These infected macrophage are carried by lymph to regional lymph nodes o Ghon complex – an area of lung inflammation that has enlarged hilar lymph nodes draining the area Seen in some cases of TB In immunosuppressed people, the M. tuberculosis can spread through blood throughout the body o When they spread, they like to spread to the upper lungs, lymph nodes, vertebral bodies, and meninges Until a sufficient immune response develops, the TB grows at the lung and spread sites Cell immunity and tissue hypersensitivity to M. tuberculosis usually appears 3-8 weeks after infection, and is marked by a positive tuberculin (TB) skin test o In most people, this response controls the infection, no symptoms develop, and the only evidence of infection is the skin TB test On some cases though, the immune response doesn’t control the primary infection, leading to progressive primary TB o Usually happens int eh young, elderly, and people with AIDS o Often this progresses to worsening pneumonia, and in the young, TB meningitis In people with immunity from previous exposure to M. tuberculosis, organisms in newly inhaled droplets are destroyed before they can multiply Nearly all TB in previously infected people is from endogenous reactivation o However when the airborne inoculum is large, or when host defenses are compromised, exogenous reinfection can happen Age influences the course of the TB infection o Kids under 5 – have a high risk of developing progressive primary TB o 5-puberty – they’re resistant to progressive TB disease, but not infection o Puberty-young adulthood – formation of an lung apex cavity is common o Mid adulthood – much better immediate and long term prognosis o Elderly – can have their defenses go down and previously gotten TB roars up, or they’re more susceptible to primary infection Endogenous reactivation of TB – secondary TB - - Endogenous reactivation of TB usually happens within 2 years after initial infection, but can happen at any time after Impairment of immunity can make a person vulnerable to reactivation of latent mycobacteria o Causes could be malnutrition, corticosteroids, cancer, and end-stage renal disease Worldwide, the most important cause of reactivation is coinfection with HIV Disturbing the mycobacteria environment, like in lung surgery, can also reactivate TB The most common site of reactivation is the apex of the lung Reactivated lesions slowly become necrotic, undergo caseous necrosis (looks cheesy), and eventually merge to form larger lesions Eventually, the caseous lesions liquefy and discharge their contents into bronchi o This creates a well-aerated cavity for the mycobacteria to grow in o It also spreads mycobacteria to other parts of the lung, which can cause rapid and progressive tuberculosis pneumonia o Also, the discharged lesion stuff can be coughed up, and become infectious droplet nuclei When hypersensitivity develops, tissue damage creates lung apex cavities characteristic of pulmonary TB T-cell mediated immunity responds to TB - - - Antibodies have no role in TB In the first few weeks after exposure, the host has almost no immune defense against M. tuberculosis, so the bacteria multiply freely in alveolar spaces or in alveolar macrophage Everyone has CD4+ T cells that can recognize mycobacterial antigens if processed and presented by macrophage with their MHC2’s o This activates the T cell and causes it to proliferate o The activated T cells then make lymphokines that attract, and activate macrophage at the site of antigen exposure o Activated macrophage use lytic enzymes and free radicals to kill the mycobacteria, but these things can also cause host tissue necrosis When there’s enough T cells, cutaneous delayed-type hypersensitivity to tuberculin develops o This response takes about 3-8 weeks The symptoms of TB are due to hypersensitivity to mycobacterial antigens o The classic tissue response to TB involves organization of macrophage, Langerhans giant cells, and lymphocytes, to form granulomas, which will contain the infection This is followed by healing with fibrosis, encapsulation, and scar formation o With time though, the centers of the granuloma can become necrotic with caseous material, that liquefies and discharges through the bronchial tree, forming a cavity and conditions for bacteria to multiply There is an equilibrium established where some macrophage kill the mycobacterium, others are killed by it, and still others just let the mycobacterium live in it - - Immunocompromised people may not contain the primary infection, and mycobacterium invade the blood and spread to cause a life-threatening military TB o Called military because the granulomas look like millet seeds (aka bird seed) o This will show granulomas (tubercles) in many organs Macrophage usually contain the M. tuberculosis, but they also make Il-1 and TNF-α, which cause fever, weight loss, and night sweats The tuberculin skin (PPD) test – tubercle mycobacteria proteins called tuberculin are injected into the dermis - - The material used is a mixture called purified protein derivative (PPD) A positive rxn is indicated by thickening (induration) of the skin several days after inoculation o This is a result of infiltration by phagocytes and T cells to the site, a delayed hypersensitivity rxn The tuberculin skin test (PPD) is most useful for diagnosing latent TB infection About 15% of people with active TB, will show a negative PPD o If you give them antiTB meds, that test will become a positive o Immunocompromised people, like those with AIDS, will have negative PPDs o So a negative tuberculin skin test (PPD) doesn’t exclude active TB infection Interferon-γ is critical in regulating the immune response to M. tuberculosis - Tests for this are way more specific for M. tuberculosis, and called interferon-γ release assays The most common manifestation of TB in adults is a chronic pneumonia that characteristically forms cavities in the apex of the lung - Persistent fever, weight loss, and drenching night sweats, are common during TB Pott disease – chronic back pain caused by M. tuberculosis infecting the vertebral bodies - Failure to treat Potts can cause destruction of vertebrae and permanent disability TB is all about balance: without T cell immunity and delayed hypersensitivity, casous necrosis wouldn’t develop, but the mycoplasma tuberculosis would proliferate unchecked, leading to military TB, which can kill way faster than chronic pulmonary TB - Ex: loss of CD4+ T cells in HIV leads to rapid progression of TB and death So the immune response contains the TB, even if it eventually causes damage Diagnose asymptomatic TB with a PPD Diagnose symptomatic TB with acid-fast staining and culture of sputum - Sputum can give you a rapid presumptive diagnosis, and contagiousness correlates with sputum smear positivity - The gold standard for diagnosing TB is culture Treat TB with isoniazid (INH), rifampin (inhibits transcription), pyrazinamide (PZA), or ethambutol - People with pulmonary TB usually become noncontagious within 2 weeks of therapy Mycoplasma tuberculosis is very good at getting resistant, so you need to treat with several drugs at once o The chances that mycoplasma will be resistant to two drugs at once is small, so taking multiple drugs prevents spread of resistance o Multidrug-resistant strains come from people not following the therapeutic course of their drug This would be catastrophic, so directly observed therapy for TB is the standard, with every dose directly administered by a health care provider o Using multiple drugs also decreases the time it takes to be cured Vaccines for TB are hard to make, cause antibodies aren’t involved, so live organisms would need injected to trigger T cell immunity - The bacilli Calmette-Guerin (BCG) vaccine is a strain of M. bovis that’s been attenuated, means made less virulent o It’s often given to newborns and young children o It will cause a positive PPD, a sign of positive immunization o BCG is not used in the US, cause then we wouldn’t be able to tell who has recent TB infections Leprosy – caused by mycobacterium leprae - - Leprosy is much less contagious than TB Leprosy still exists in tropical countries, but is rare in the US Getting leprosy requires prolonged contact with infectious people o It used to be thought it spread by skin-skin contact, but now it’s thought it’s airborne through the nose M. leprae survives and multiplies in macrophage o To really kill them, the macrophage need activated by T cells Leprosy mycobacteria grow best at low temperatures o So that lets them multiply the fastest on skin, nose, and other superficial temperatures Two types of leprosy: o Tuberculoid leprosy – characterized by red blotchy lesions, with local loss of sensation (anesthesia) Usually on the face, trunk, and extremities The mycobacteria grow and cause thickening of nerve sheaths, that can be felt through the skin, a characteristic of leprosy Better prognosis than lepromatous leprosy o Lepromatous leprosy – suppresses macrophage and T cells, so that there is little or no delayed-type hypersensitivity This lets lots of M. leprae grow in the skin and superficial nerves More organism than any other human disease Loss of local sensation cause easy damage to the body by the host, which can also become infected