ISOLATION, EXPANSION AND CHARACTERIZATION OF SINGLE
MESENCHYMAL STEM CELLS
Jared Everett Christensen
B.S., California Polytechnic State University, San Luis Obispo, 2003
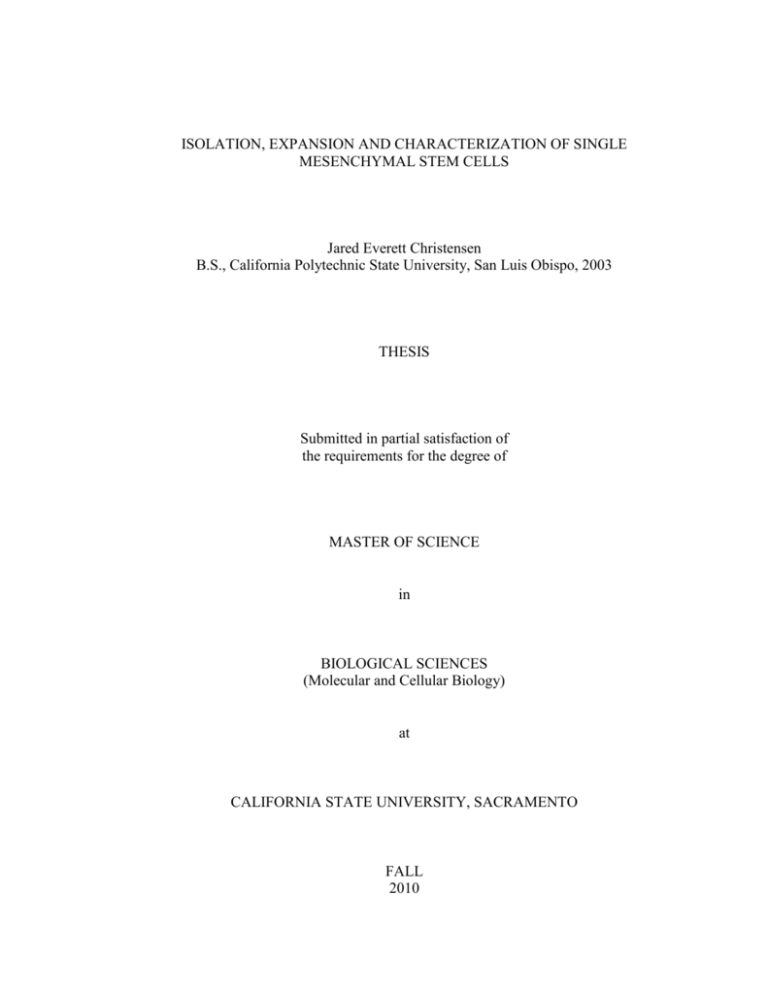
THESIS
Submitted in partial satisfaction of
the requirements for the degree of
MASTER OF SCIENCE
in
BIOLOGICAL SCIENCES
(Molecular and Cellular Biology)
at
CALIFORNIA STATE UNIVERSITY, SACRAMENTO
FALL
2010
© 2010
Jared Everett Christensen
ALL RIGHTS RESERVED
ii
ISOLATION, EXPANSION AND CHARACTERIZATION OF SINGLE
MESENCHYMAL STEM CELLS
A Thesis
by
Jared Everett Christensen
Approved by:
__________________________________, Committee Chair
Thomas Landerholm, PhD
__________________________________, Second Reader
Alice F. Tarantal, PhD
__________________________________, Third Reader
Tom Peavy, PhD
____________________
Date
iii
Student: Jared Everett Christensen
I certify that this student has met the requirements for format contained in the University
format manual, and that this thesis is suitable for shelving in the Library and credit is to
be awarded for the thesis.
______________________________, Graduate Coordinator
James W. Baxter, PhD
Department of Biological Sciences
iv
_________________
Date
Abstract
of
ISOLATION, EXPANSION AND CHARACTERIZATION OF SINGLE
MESENCHYMAL STEM CELLS
by
Jared Everett Christensen
Mesenchymal Stem Cells (MSCs) are multipotent precursors to many
mesodermal cell lineages in vertebrate animals and are most often obtained from bone
marrow. Certain attributes of MSCs, including migration toward sites of inflammation,
ease of transduction, and lack of immunogenicity, suggest these cells may be potentially
useful for regenerative medicine. Putative therapeutic uses include regeneration of
damaged tissue, acting as a vessel for delivering a therapeutic transgene, support of other
cell types for tissue repair, and modulating the immune reaction to co-transplanted cells
or tissues. However, MSCs lack distinctive surface markers and conventional MSC
culture has been shown to be heterogeneous. A thorough characterization of MSC
culture at a single cell level has not been adequately demonstrated. These conditions
lead to the question of whether there are true mesenchymal “stem” cells, or simply a
mixed population of committed mesenchymal progenitors.
In addition to being an
important question in MSC biology, this may prove to be an important distinction in
certain therapeutic settings. In this study, the methods used to identify hematopoietic
high proliferative potential-colony forming cells (HPP-CFCs) and high proliferative
potential- endothelial colony forming cells (HPP-ECFCs), were adapted to investigate
v
the existence of high proliferative potential-mesenchymal colony forming cells (HPPMCFCs), and the differentiation potential of these cells toward adipogenic,
chondrogenic, and osteogenic lineages at a single cell level. This study demonstrates for
the first time that a hierarchy of mesenchymal cells within conventional MSC culture
can be described, and single HPP-MCFCs can differentiate toward adipogenic,
chondrogenic and osteogenic lineages as well as form secondary colonies.
__________________________________, Committee Chair
Thomas Landerholm, PhD
____________________
Date
vi
ACKNOWLEDGMENTS
I would like to thank Dr. Alice Tarantal and Dr. Chang Lee at the California
National Primate Research Center, University of California, Davis, without whom this
study would not have been possible. I would like to thank Dr. Mervin Yoder at Indiana
University School of Medicine for his expert advice. I would also like to thank Carol
Oxford, Araceli Cuellar, Stacy Ralston, and Christine Mall at the University of
California, Davis for technical assistance. Finally, I would like to thank Dr. Thomas
Landerholm for his patience and guidance during the writing process. These studies
were supported by National Institutes of Health (NIH) grants #HL073220, #HL085036,
and the Primate Center base operating grant #RR00169.
vii
TABLE OF CONTENTS
Page
Acknowledgments............................................................................................................. vii
List of Tables ..................................................................................................................... ix
List of Figures ......................................................................................................................x
INTRODUCTION ...............................................................................................................1
METHODS ........................................................................................................................18
MC Culture ............................................................................................................18
Preparation of MC Feeders ....................................................................................18
Preparation of Basement Membrane Extracellular Matrix ....................................19
Transduction and Sorting .......................................................................................19
Differentiation of MCs ...........................................................................................20
Cell Staining...........................................................................................................21
PCR Analysis .........................................................................................................22
ICC .........................................................................................................................23
Flow Cytometry .....................................................................................................25
Statistical Analysis .................................................................................................25
RESULTS ..........................................................................................................................27
DISCUSSION ....................................................................................................................37
CONCLUSIONS................................................................................................................41
Literature Cited ..................................................................................................................43
viii
LIST OF TABLES
Page
Table 1.
Identification Information for Adipogenic, Chondrogenic and
Osteogenic Genes Utilized for qRT-PCR ......................................................24
ix
LIST OF FIGURES
Page
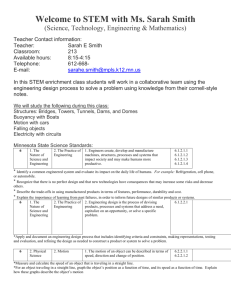
Figure 1.
Plan for Single Mesenchymal Cell (MC) Isolation and
Expansion......................................................................................................16
Figure 2.
Comparison of Single Mesenchymal Cell Growth with
Fluorescence Images .....................................................................................28
Figure 3.
Comparison of Single Mesenchymal Cell Proliferation After
First and Second Sortings .............................................................................29
Figure 4.
Charting Proliferation of Single Mesenchymal Cells
Through 13 Days in Culture .........................................................................30
Figure 5.
Comparison of Surface Marker Expression in Conventional
Mesenchymal Stem Cell Culture and High Proliferative
Potential-Mesenchymal Colony Forming Cells ............................................32
Figure 6.
Image Verification of Adipogenic, Chondrogenic and
Osteogenic Differentiation of Single Mesenchymal CellDerived Colonies ..........................................................................................33
Figure 7.
Pre- and Post-Differentiation qRT-PCR for Adipogenic,
Chondrogenic, and Osteogenic Gene Expression in High
Proliferative Potential-Mesenchymal Colony Forming Cells .......................35
x
1
INTRODUCTION
The Promise of Stem Cells
Stem cells are defined as having two essential properties: the ability to self-renew
and reconstitute their own population, and the ability to differentiate into multiple
different types of mature daughter cells. The latter ability is referred to as the cell’s
potency, and several different levels of potency exist during the development of an
organism. Totipotent cells exist for a short time between fertilization and formation of
the blastocyst. These cells have the potential to become any cell type in the body, as
well as the extra-embryonic tissues such as the placenta or yolk sac. Pluripotent cells
have lost the ability to form the extra-embryonic tissues, but are still able to form all
three germ layers of the developing embryo (endoderm, mesoderm, ectoderm).
Pluripotent cells exist in the inner cell mass of the blastocyst and are a source of human
embryonic stem cell (hESC) lines [1].
hESCs are highly prized for stem cell research due to their potential; these cells
can be utilized by investigators studying development in any organ or tissue type in the
body.
New factors for modulating differentiation can be tested and protocols for
directing cell fate may be developed, producing new cell sources for regenerative
medicine [2]. Also, hESCs are particularly useful because they may be utilized to study
different disease mechanisms which may occur during any point in development, from
the most immature state all the way through terminal differentiation. Pharmaceutical
2
discovery is another use for hESCs, from screening for new drugs, to safety and efficacy
assessment [3]. Transplantation studies in animal models have shown great promise as
well, as protocols have been developed for deriving cell types including hematopoietic
cells, cardiomyocytes, oligodendrocytes, dopamine neurons, and pancreatic beta cells,
among others. However, the same potential for differentiation that makes hESCs useful,
coupled with the complex signaling that is necessary for normal embryonic development,
also render them difficult to control [2]. Often the results of transplantation include
teratomas, a hurdle that must be overcome before widespread clinical use will be
possible [4].
Another difficulty that has plagued hESC research is the ethical argument posed
by critics that deriving a cell line from a blastocyst is the moral equivalent of destroying
a human life.
Federal funding laws are changing with the new presidential
administration. However, until recently only the 19 hESC lines that were in existence in
August, 2001 have been available for research, limiting the diversity of data obtained
from such studies. This limitation slows down the process of investigation for hESCs,
which is necessary before the safety of any type of human trial can be accurately
assessed. The subsequent lag in discovery has in turn lead to further criticism that hESC
research has not lived up to its promise [5]. All in all, hESC research still holds the
greatest potential for regenerative medicine, but has proven to involve the greatest
difficulties as well.
One alternative to hESCs for use in clinical studies is adult stem cells. Adult
stem cells cannot generate an entire new tissue as hESCs are able to, but the stigmas
3
associated with hESCs are not applicable to adult stem cells, which can be found in
certain tissues from birth through adulthood and harvested without great harm to the
donor. These cells are self-renewing and multipotent, being able to differentiate into
multiple cell types of the same embryonic germ layer. Hematopoietic stem cells (HSCs)
are the classic example of adult stem cells, with the first HSC transplantation taking
place in 1956 [6].
Since then, HSCs have become an invaluable tool, both in
understanding the basic science of cell biology, and as treatment in clinical settings
involving cancers of the blood. Amazingly, a single transplanted HSC has the potential
to repopulate the entire blood system [7]. It has been shown however, that successful
transplantation of HSCs is aided greatly by another type of adult stem cell, the
mesenchymal stem cell (MSC).
Mesenchymal Stem Cells
MSCs are multipotent precursors to many mesodermal cell lineages in vertebrate
animals. They are present from early gestation through adulthood and although they
have been isolated from many adult tissues, MSCs are most commonly obtained from
bone marrow where they act as part of the stroma to support hematopoietic
differentiation. MSCs display a stable phenotype in long-term culture and retain the
potential for adipogenic, chondrogenic, and osteogenic lineage differentiation in vitro [8]
and are typically involved in the healing of damaged tissues such as bone, cartilage,
muscle, ligament, tendon, adipose, and stroma in vivo [9]. MSCs are currently utilized
as treatment for repair of bone defects in animals [10], as well as osteogenesis
4
imperfecta in children [11].
In addition to growth and differentiation, other
characteristics of MSCs such as migration, stable long-term transduction [12], and lack
of immunogenicity suggest that these cells will also play further roles in regenerative
medicine [13]. MSCs have shown positive results in studies involving hematopoietic
transplantation [14], arthritis therapy [15], cardiac repair [16, 17], kidney regeneration
[18], skin wound healing [19], intervertebral disk repair [20], and many others. The
utilization of MSCs has been called the “most exciting advance in cell therapy following
the widespread use of HSC transplantation” [21]. In fact, the potential of the putative
functions for MSCs in regenerative medicine are such that hundreds of human trials
involving MSCs are currently under way all across the globe [22].
Therapeutic Uses for MSCs
Several possible therapeutic functions exist for MSCs. First, they may directly
participate in cell repopulation via expansion and differentiation. Disease caused by
physical or chemical damage may soon be treated by directing the differentiation of a
patient’s own stem and progenitor cells into the depleted cell types and introducing them
into the affected tissue [23]. The hypothesis that MSCs could reconstitute a population
of stem cells in adipose, bone, or cartilaginous tissues has been disseminated for many
years [24], and continues to be investigated today [25]. Also, as stated previously, MSC
are under investigation for direct repair of many other tissues such as heart, kidney, and
skin.
5
A second possible role for MSCs is as a vessel for delivering a therapeutic
transgene. Severe combined immunodeficiency (SCID) [26] and Parkinson’s disease [27]
are examples of target diseases for stem cell-based gene therapy. The dysfunctional
allele(s) that may be responsible for a disease can be circumvented by the insertion of a
functional gene into the patient’s stem cells, followed by transplantation into an
appropriate tissue where they can propagate and produce the therapeutic gene product(s)
[27]. Transplanted MSCs have been reported to stably reside in several tissue types
including bone [28], cardiac [29], and neural tissues [30]. Also, it has been shown that
human MSCs can maintain transgene expression after expansion, differentiation, and
transplantation into NOD/SCID mice [28].
Subsequent migration of transplanted MSCs toward sites of inflammation is
another ability which makes transduced MSCs attractive as therapeutic agents.
Although the mechanisms behind MSC migration require further research, it has been
shown that the chemotactic factor CXCL12, which is released during inflammation,
induces expression of genes involved in cellular movement, including migratory factors
in MSCs [31]. Other factors including hypoxic conditions, stromal cell-derived factor-1
(SDF-1), and hepatocyte growth factor (HGF) are also being examined for their role in
attracting MSCs to damaged regions of tissue [32]. Due in part to their ability to migrate,
MSCs have been shown to be an effective therapeutic agent to fight the tumor
glioblastoma multiforme (GBM).
GBM is highly invasive and diffuse, rendering
surgery inadequate, and leading to a median survival time of 10-12 months. MSCs
engineered to express tumor necrosis factor apoptosis ligand (TRAIL) were shown to
6
migrate toward GBM cells. There they remained undifferentiated and non-expansive,
and stably expressing and secreting TRAIL, effectively reducing the tumor burden and
increasing survival time in a mouse model [33].
A third possibility for MSCs in tissue repair is an indirect role in support of other
cell types. MSCs are known to support hematopoiesis in bone marrow by acting as part
of the stroma, and allogeneic MSC transplants have been shown to enhance engraftment
of HSC [34]; MSCs supply physical support and cytochemical direction by producing
growth factors and cytokines, likely providing the essential cues for cell proliferation
and differentiation [14]. MSCs given to patients who experienced tissue toxicity after
receiving HSC transplants have been shown to aid in clearing severe haemorrhagic
cystitis, pneumo-mediastimun, as well as diverticulitis and peritonitis caused by steroidresistant graft versus host disease (GVHD) [35].
A more recent hypothesis suggests a similar role for those MSCs found to reside
in other tissues undergoing repair and re-growth; MSCs may act as a support system for
other stem and progenitor cells, instead of the direct role previously advocated [36].
MSCs have been shown to home to areas of hypoxia and cause rapid revascularization
after injury [32]. This ability is particularly important for treatment of ischemic injury.
Ischemic tissue regeneration studies utilizing MSCs have included stroke models [37,
38], skeletal muscle ischemia [39, 40], and a myocardial infarction (MI) model [41].
Heart disease is the most common cause of mortality in developed nations [17]. Even
when patients survive acute attacks like MI, however, there is often loss of functional
tissue leading to decreased cardiac output and decreased quality of life.
7
The utilization of MSCs for cardiac repair is one area of regenerative medicine
where all of these cells’ putative therapeutic capabilities have been explored. Although
studies have shown evidence of differentiation of MSCs toward cardiomyocyte-like cells
for direct repopulation of the damaged area [42-44], it has recently been shown that only
a very small portion of cells from MSC culture (~0.07%) retain this potential [45]. It
would be preferable to have a pure population of undifferentiated MSCs with myogenic
potential for transplantation in order to take advantage of their ability to migrate to the
edge of necrotic tissue and retain the potential for proliferation as the tissue begins to
regenerate. Thus, better markers are needed for identification of myogenic-competent
cells within MSC culture before the direct repopulation approach is likely to become a
practical option. However, a current Phase II study by Osiris Therapeutics has shown a
significantly increased ejection fraction after major anterior wall heart attacks with MSC
transplantation [22]. This improvement is more likely due to MSC’s pro-angiogenic
capabilities, improving the microenvironment and secreting factors that lead to increased
blood flow and greater access to nutrients required for efficient regeneration.
The fourth therapeutic role for MSCs is as an immune system modulator.
Several studies have shown that allogeneic transplantation of MSCs does not appear to
induce an immune response [46-48], leading to greater tolerance and reducing both the
occurrence and the extent of GVHD [49]. MSCs have been shown to alter proliferation
and differentiation of B-cells, monocytes, and immature dendritic cells via expression of
immune modulating factors such as prostaglandin-E2 (PGE-2), IL-10, and transforming
growth factor-β (TGF-β), as well as inhibiting NK cells and T-cells via indoleamine-2,3-
8
oxygenase [50].
Adding MSCs to a mixed lymphocyte culture suppresses T-cell
proliferation, with the degree of suppression being dose-dependent and MHC
independent. These findings may also be explained by the fact that MSCs do not
express co-stimulatory molecules such as CD40, a protein found on APCs which must
come in contact with its corresponding receptor (CD40L) on T helper cells in order for
activation, and subsequent proliferation of resting T cells, to occur. Although the precise
mechanism by which MSCs modulate T cells likely varies depending on the cell types
present in vivo [36].
Overall, these data present the possibility of transplanting
allogeneic MSCs, thus removing the need to harvest cells from a patient if it may cause
undue risk. Also, expansion of MSCs can take place prior to need, and universal donors
may be utilized for many patients. Importantly, MSCs harvested from adult rhesus
monkey bone marrow have shown decreased potential for self-renewal and
differentiation when compared to MSCs from younger age groups [51, 52]. Therefore,
future therapeutic approaches for adult patients may prove to be more effective when
utilizing allogeneic cells from younger donors. It has been proposed that a stem cell
bank of well-characterized MSCs, ready for use in allogeneic transplants, would be a
valuable tool for both investigators and clinicians [21].
While initial therapeutic studies focused on directly transplanting MSCs into the
injured site, some more recent strategies have involved tissue engineering in which
synthetic or bioengineered scaffolds seeded with MSCs are utilized [53]. MSCs are held
in place by the scaffold while they secrete soluble factors, contributing to tissue repair.
One difficulty with this approach is that vasculature is required around the site of the
9
construct to support the seeded MSCs’ metabolic requirements.
The size of the
construct is therefore limited to the depth of diffusion of oxygen and other nutrients.
Subsequently, vascularized constructs have been developed [54], broadening application
of these scaffolds to include large bone defects [55].
In addition to studies of their therapeutic properties, MSCs are useful in the study
of transformation and cancer. According to the cancer stem cell theory, tumor cells have
differing potential for propagation of the tumor. Only a small subset of tumor cells
retains this potential and can be called “cancer stem cells” [56]. MSCs have been shown
to be susceptible to transformation and some studies have suggested they have a possible
role in cancer development.
MSCs are theorized to act as cancer stem cells in
malignancies such as Ewing’s sarcoma [57] or myxoid liposarcoma [58].
The
differentiation state of MSCs that are thought to give rise to liposarcomas has even
become the basis for a new classification system of these tumors [59].
The role that MSCs play in tumor development, like the role that they play in
healing, could also be indirect. Just as MSCs support hematopoiesis and regeneration of
tissue by secretion of cytokines and creating an ideal microenvironment, they may also
support growth of solid epithelial tumors. Considering this supportive role, MSCs have
been proposed as the initial source of tumor-associated fibroblasts and carcinomaassociated fibroblasts (CAFs), cells known to be essential for supporting and sustaining
malignancies [60]. However, the true source of these cells has not been conclusively
determined [21]. Also, the high rate of transformation reported for MSCs is based only
on experiments in mice, which are often utilized as an in vivo model for human stem cell
10
engraftment studies. Therefore, there is now disagreement on the neoplastic tendencies
of human MSCs due to data that has shown a lack of transformation or mechanisms for
maintenance of telomeres after long-term culture [61]. Also, data from both humans and
rhesus macaques show failure of transplanted MSCs to produce tumors after long-term
culture [62]. Owing in part to this controversy, MSCs remain attractive for future
studies in transformation and tumor development, which are needed to elucidate the
tumor microenvironment and the initial sources of the cell types involved.
In the
meantime, MSCs utilized for human transplantation are grown under Good
Manufacturing Practice (GMP) in facilities where their safety and potency are constantly
tested [63].
There remain a number of other unresolved issues surrounding MSCs including
whether they are true stem cells, and methods for in vivo identification [64]. Also, a
quantitative analysis at a single cell level of MSC culture to determine the frequency of
cells that have the ability to self-renew and differentiate toward multiple lineages has not
yet been fully investigated. Since MSC cultures may contain a population of several
different types of progenitor cells, an assay on single stem cells is necessary for
determining the true quantity of stem cells in this mixed population.
MSC Characterization Difficulties
Despite the interest and potential associated with MSCs, cell characterization
similar to the techniques used for HSC has yet to be achieved. Isolation of MSCs was
first achieved nearly 40 years ago from guinea pig bone marrow [65]. These studies
11
involved culture of bone marrow mononuclear cells on a plastic substrate, which allow
fibroblast-like cells (later named MSCs) to adhere while others, such as hematopoietic
cells, do not. These culture conditions are still used today, and supplemented with
growth promoting media. However, studies have shown that MSC cultures based solely
on adherence to plastic are highly heterogeneous [66, 67]. Other protocols have also
been developed to isolate MSCs, including flow cytometry and cell sorting with
antibodies to cell surface markers such as STRO-1 [68], SSEA-1/CD15 [69], and SSEA4 [70]. The STRO-1 surface marker is found on ~10% of bone marrow mononuclear
cells. Fibroblast-like colony forming units (CFU-F) are exclusively STRO-1pos and have
shown adipogenic, myogenic, and fibroblastic potential, yet the vast majority of these
cells are erythroid precursors [68].
Experiments utilizing SSEA-1/CD15 in mice have shown a multipotent
population of cells that are able to give rise to SSEA-1pos as well as SSEA-1neg cells. The
negative cell fraction showed less differentiation potential and was unable to give rise to
SSEA-1pos cells, suggesting a hierarchical relationship.
However, SSEA-1pos
populations were not adequately shown to have been derived from a single cell, since
FACS sorting was utilized without fluorescence microscopy [69]. Experiments with the
marker SSEA-4 showed multipotent cells as well, although clonality was again not
adequately demonstrated [70]. Interestingly, SSEA-4pos cells were shown to be SSEA1neg, indicating that SSEA-1 is only expressed in a subset of multipotent cells and is not
a marker of the most immature MSC.
12
Consequently, a unique marker has not been found on MSCs to distinguish them
from all other cell types. Cells from MSC culture are known to be positive for the
surface peptides SH2, SH3, and SH4, and the surface receptors CD29, CD71, CD90,
CD123, and CD166. Other cell types also express these markers, thus it would be
preferable if there were truly a unique marker to identify the most immature and
therefore the most highly potent MSCs. For example, other cells express markers that
MSCs do not, such as CD31 for endothelial cells, CD14 for monocytes and macrophages,
and CD34 for hematopoietic progenitor cells.
Unfortunately, all current selection
protocols still produce heterogeneous cultures with respect to surface markers and cell
morphology [8].
Due to the lack of a unique surface marker, investigators have thus far been
unable to definitively show that a single MSC has both indefinite proliferation potential
and the ability to give rise to multiple daughter cell types [36]. Therefore, there is still
debate as to whether MSC culture contains true stem cells, or simply consists of a
heterogeneous mix of committed adipogenic, chondrogenic, and osteogenic progenitor
cells. This question may be answered by isolating a single MSC, expanding it through
many population doublings, and directing the differentiation of the resulting
homogeneous population of cells.
Proliferation Potential of MSCs
Differentiating between populations of cells within the same culture based on
proliferation potential has proven to be a useful technique in characterizing other stem
13
and progenitor cells, and may prove a useful tool for MSCs as well. Hematopoietic high
proliferative potential-colony forming cells (HPP-CFCs), obtained from both mouse and
human bone marrow, form large colonies (~50,000 cells) in double-layer agar cultures
and differentiate into multiple hematopoietic cell types [71-73].
Low proliferative
potential-colony forming cells (LPP-CFCs) are defined as hematopoietic cells that can
grow into colonies smaller than HPP-CFCs but greater than 50 cells [69]. Further
characterization experiments for HPP-CFCs have identified them as the most primitive
hematopoietic progenitor cells that can be assayed in vitro [74].
This method for
classifying different cell types based on their proliferative potential has also been
influential in identifying a hierarchy of circulating endothelial progenitor cells (EPCs).
Ingram et al. [75] identified four distinct cell types in EPC culture which included high
proliferative potential-endothelial colony forming cells (HPP-ECFCs), low proliferative
potential-endothelial colony forming cells (LPP-ECFCs), endothelial cell clusters, and
mature differentiated endothelium. HPP-ECFCs have been shown to give rise to
secondary and tertiary HPP-ECFCs, as well as all subsequent stages of endothelial
progenitors [75].
The techniques used for identifying HPP-CFCs and HPP-ECFCs
provide a unique quantitative method for assessing the degree of heterogeneity in stem
cell cultures. A similar proliferation assay, coupled with subsequent assays to determine
the differentiation potential of single MSC-derived colonies may also offer important
insight into MSC biology.
Single Cell Isolation Techniques
14
An essential hurdle that must be overcome in order to show that colonies in
culture are truly clonal is the difficulty of ensuring that only one cell from culture has
been isolated for growth.
Studies involving the isolation of single MSC for
characterization have been attempted before [9, 25], although the precision of the
techniques utilized to isolate single MSCs are questionable.
Three techniques are
normally used to isolate single cells in culture. These include cloning rings, serial
dilution, and fluorescence activated cell sorting (FACS).
Pittenger et al. used the
cloning ring technique in 1999, which involves plating cells at low density, identifying
single cells, and allowing them to grow into colonies. The colonies are then separated
from the rest of the culture by a glass ring, harvested, and transferred to a new culture
plate. The inaccuracy in this technique comes from the uncertainty that the ring has
surrounded only cells from the desired colony, and that no cells have migrated into this
colony from elsewhere in the culture. Given their highly migratory nature, the cloning
ring technique is not ideal for clonal assays involving MSC.
The serial dilution technique was utilized by Mareddy et al. (2007). A sample of
cells in solution was counted to find the concentration in cells per unit volume. This
sample was then diluted to the point that when an aliquot was transferred to a well in a
new culture plate, it was likely to only contain a single cell. The wells could then be
scanned to confirm that only a single cell was present. The trouble associated with this
technique is that cells are transparent under normal light microscopy and although a well
may appear to contain only one cell, it is difficult to recognize cells that have settled
against the wall of the well. The authors confirmed that this technique is imprecise
15
when they acknowledged that wells contained between 1 and 3 cells at initial plating
[25].
The third technique involves using a FACS-based cell sorting machine to deposit
single cells into the wells of a culture plate. Single cell sorting is again not entirely
accurate; two or three MSCs are often stuck together. With this technique however,
MSCs can also be transduced to express a marker such as enhanced green fluorescent
protein (EGFP) prior to sorting. The cell sorter can then select only EGFP expressing
cells, which will eliminate the uncertainty involved in identifying wells with single cells
if they are subsequently scanned under fluorescent microscopy. Cells will fluoresce
green and can easily be identified anywhere in the well, including the sides and walls.
Untransduced feeder cells can also then be utilized to promote proliferation while still
being able to detect which cells descended from the initial single cell (Fig. 1).
Summary
MSCs are adult stem cells that are potentially highly effective agents for
regenerative medicine via several different therapeutic uses and lack the ethical issues
that have been associated with stem cells of embryonic origin. However, conventional
MSC culture has been shown to be heterogeneous and a thorough characterization at the
single cell level has not been adequately demonstrated. These conditions lead to the
question of whether there are true mesenchymal “stem” cells, or just mixed populations
of adipogenic, chondrogenic, and osteogenic progenitors.
In addition to being an
important question in MSC biology, this may prove to be an important distinction in
16
Figure 1. Plan for Single Mesenchymal Cell (MC) Isolation and Expansion. MC from
conventional MSC culture were transduced with an HIV-1 derived lentiviral
vector containing enhanced green fluorescent protein (EGFP) under the
control of the cytomegalovirus (CMV) promoter. EGFP expressing cells
were then sorted as single cells and expanded with irradiated feeder MSCs to
produce clonal colonies.
17
certain therapeutic settings.
In the present study it is hypothesized that conventional, heterogeneous MSC
culture contains a hierarchy of cells with respect to proliferation and differentiation
potential. Also, it is hypothesized that a population of cells with both self-renewal and
multipotent differentiation capabilities exists within MSC culture. These hypotheses
were tested by first adapting the FACS-based methods used to classify HPP-CFCs and
HPP-ECFCs in order to assess proliferation potential and renewal capabilities of single
cell-derived colonies.
Finally, the differentiation potential of these colonies was
assessed via PCR, immunocytochemistry (ICC), and cell staining experiments. Single
cells from MSC culture and their subsequent clonal colonies will be referred to as
mesenchymal cells (MCs), as their “stem cell” properties are under investigation. This
study demonstrates for the first time that a hierarchy of MCs within conventional MSC
culture can be described, and multipotent high proliferation potential-mesenchymal
colony forming cells (HPP-MCFCs) can form secondary colonies at a single cell level.
18
METHODS
MC Culture
Human bone marrow mononuclear cells (1x107 cells, Cambrex, NJ) obtained
from healthy donors (N=3) were plated on 100 mm plates in -20 medium (-MEM
supplemented with 20% fetal bovine serum (FBS), 1% L-glutamine, and 1% pen-strep)
and incubated at 37oC and 5% CO2. Passage 0 cultures were washed with phosphate
buffered saline (PBS) three times every other day until cells reached approximately 80%
confluence. Cells were then washed with PBS and incubated with 0.25% trypsin-EDTA
(Gibco, Carlsbad, CA) for 5 min at 37oC, then -20 medium was added to cells in at
least a 1:1 ratio to trypsin in order to inactivate.
Cells were counted with a
hemacytometer and plated in -20 medium at 5x103 cells/cm2. For subsequent passages,
medium was changed the following day and every third day thereafter, and cultures were
passaged when 80% confluence was reached.
Preparation of MC Feeders
MCs used as feeders for EGFP-positive sorted single MCs were plated at 5x103
cells/cm2 in 100 mm plates with -20 medium and grown to approximately 80%
confluence as described above. Cells were washed with PBS and incubated with 0.25%
trypsin-EDTA for 5 min at 37oC and 5% CO2. Cells were collected, washed in fresh
19
medium, and irradiated using a gamma irradiator (J. L. Shepherd & Associates, CA) at
3,000 rads.
Preparation of Basement Membrane Extracellular Matrix (ECM)
PYS-2 cells (ATCC, VA), which have been shown to produce type IV collagen,
laminin, and heparin sulfate proteoglycans [76], were cultured in DMEM containing 10%
FBS, 1% L-glutamine, and 1% pen-strep. Cells were cultured to 100% confluence with
medium replaced every other day. Cells were then treated with medium containing 5%
dextran, and maintained in culture for 5-9 days. Cultures were washed with water and
de-cellularized with 1% NH4OH for 10 min with 5 subsequent washes with PBS. Decellularized culture dishes were utilized along with untreated culture dishes to compare
proliferation of single MCs with and without untransduced feeder cells.
Transduction and Sorting
MCs were plated in 6-well plates in -20 medium at 5x103 cells/cm2 and
incubated at 37oC overnight. Cells were transduced with an HIV-1-derived lentiviral
vector (1x106 infectious particles/ml) expressing either EGFP or red fluorescent protein
(RFP) under the control of the cytomegalovirus (CMV) promoter in medium containing
4 g/ml polybrene. Cells were incubated with the vector overnight at 37oC, then washed
with PBS and replenished with new medium. After cells reached approximately 80%
confluence, cells were trypsinized and stained with 1 g/ml propidium iodide. EGFP-
20
expressing MCs that did not take up propidium iodide were sorted into 24-well plates
with and without irradiated feeder MCs or ECM at 1 cell/well using a MoFlo Cell sorter
(DakoCytomation) and incubated overnight at 37oC. On day 1 post-sorting each well
was monitored for EGFP-positive cells under a fluorescence microscope equipped with
an X-Y stage, and wells containing more than 1 cell were excluded from the study.
Wells containing single cells were monitored and counted every 3 days and those that
showed growth after 13 days in culture were trypsinized, counted using a hemacytometer,
and passaged at 5x103 cells/cm2. A subset of single MC-derived colonies showing
greater than 9 population doublings were combined and again sorted into 24-well plates
with irradiated feeder MCs at 1 cell/well and incubated overnight at 37oC. Wells were
verified to contain a single EGFP-positive cell and were monitored for growth for 13
days as described above. RFP-positive cells were co-cultured with EGFP-positive cells
and used as a control to identify any possible cell fusion events.
Differentiation of MCs
MCs derived from single cells and expanded with irradiated feeder MCs were
differentiated into osteogenic, adipogenic, and chondrogenic lineages using Osteogenic,
Adipogenic, and Chondrogenic Differentiation Medium (Lonza, Allendale, NJ)
following the manufacturer’s recommendations. Briefly, for osteogenic differentiation,
cells derived from single MCs were plated at 3.1x103 cells/cm2 in 2-well Permanox
chamber slides (Nunc, Rochester, NY) in -20 medium and incubated overnight. Each
well was replaced with Osteogenic Induction Medium, which was refreshed every 3-4
21
days for 21 days. For adipogenic differentiation, single MC-derived cells were plated at
a density of 2.1x104 cells/cm2 in 2-well chamber slides, and -20 medium was
replenished every 2-3 days until the cultures formed a confluent monolayer. Cells were
then incubated in three cycles consisting of 3 days of culture in Adipogenic Induction
Medium followed by 1-3 days of culture in Adipogenic Maintenance Medium. Cells
were then cultured an additional 7 days in Adipogenic Maintenance Medium, replacing
the medium every 2-3 days.
For chondrogenic differentiation, 2.5x105 single MC-
derived cells were pelleted in triplicate at 150 g for 5 min at room temperature in 15 ml
polypropylene tubes in -20 medium. MC pellets were then resuspended in incomplete
Chondrogenic Induction Medium and centrifuged again under the same conditions. The
pellets were resuspended in complete Chondrogenic Induction Medium (supplemented
with 10 ng/ml TGF-3), centrifuged once more, and incubated at 37°C and 5% CO2. The
cell pellets were fed every 2-3 days by complete replacement of the medium with freshly
prepared complete Chondrogenic Induction Medium for 21 days.
Cell Staining
Adipogenic-differentiated slides were stained with Oil Red-O. Cells were fixed
in 10% buffered formalin (Fisher, Pittsburg, PA) for 60 min at room temperature. Stock
Oil Red-O solution was prepared by adding 100 mL isopropanol to 300 mg Oil Red-O
Powder (Sigma, St. Louis, MO). Working solution was prepared with 3 parts stock
solution to 2 parts deionized water and filtered. After fixing, slides were washed with
22
water then 60% isopropanol for 5 min. Slides were stained with working Oil Red-O
solution for 2 hrs then rinsed with water until clear (about 50 mL).
Slides were then
counterstained with hematoxylin for 45 sec and slides were washed with water until
clear.
Chondrogenic-differentiated pellet sections were stained with Safranin-O.
Sections were fixed in methanol at -20oC for 20 min. Slides were allowed to dry, then
washed in PBS for 2 min. Sections were stained with hematoxylin for 75 sec, rinsed
with water, stained in 0.02% Fast green FCF (Sigma) for 3 min then in 0.1% Safranin-O
(Sigma) for 5 min. Sections were dehydrated in 90% ethanol (2x5 min), 100% ethanol
(2x5 min), and xylene (2x5 min) then a coverslip was placed.
Osteogenic-differentiated slides were stained with Von Kossa stain. Cells were
fixed in 10% buffered formalin for 1 hr at room temperature. Slides were then washed
with water and stained with 1% aqueous silver nitrate (Sigma) and incubated at room
temperature under ultraviolet light for 45 min. Slides were then washed with water until
clear and stained with 3% aqueous sodium thiosulphate (Sigma) for 5 min. Slides were
washed with tap water and stained with 0.1% aqueous Neutral Red (Sigma) for 1 min
then washed with water. Images for all slides were obtained with a Zeiss Axiovert 100
microscope (Zeiss, Oberkochen, Germany).
PCR Analysis
Total RNA was prepared from sorted EGFP-positive, differentiated MCs using
the Qiagen RNeasy Micro kit (Qiagen, Valencia, CA). cDNA was synthesized using the
23
Sensiscript RT kit (Qiagen). Real-time PCR was performed using the QuantiTect SYBR
Green PCR kit (Qiagen) with the primers shown in Table 1. The primers for the
housekeeping gene elongation factor-1 alpha (EF1 analysis were EF1-Forward (5’GAC-CCA-CCA-ATG-GAA-GCA-G-3’)
and
EF1-Reverse
(5’-TGT-GGC-AAT-
CCA-ATA-CAG-GG-3’). Amplification was performed in an ABI 7900 Sequence
Detection System (Applied Biosystems, Foster City, CA). Signal copy numbers were
calculated per copies EF1based on a standard curve (r2 = 0.9997) [52].
ICC
All primary and secondary antibodies were obtained from Millipore (Bilerica,
MA). Chamber slides from adipogenic and osteogenic differentiation and sections from
chondrogenic pellets were washed for 10 min in PBS then blocked with 1% bovine
serum albumin (BSA) in PBS for 20 min. For adipogenic slides, one well was incubated
with mouse anti-human Peroxisome Proliferator-Activated Receptor (PPAR) γ1/γ2 at
1:500 dilution in 1% BSA for 1 hr while the other well remained in 1% BSA as a control.
Slides were then washed 3 times for 5 min in PBS and incubated for 1 hr in goat antimouse Alexafluor 594 at 1:200 dilution in 1% BSA. Osteogenic slides were incubated
with rabbit anti-human Bone Sialoprotein (BSP) II at 1:100 dilution in 1% BSA in one
well and 1% BSA alone in the other for 1 hr, followed by 5 min in PBS three times and 1
hr of goat anti-rabbit Alexafluor 594 (1:200 dilution) incubation. Chondrogenic sections
were incubated for 1 hr with rabbit anti-human Collagen (COL) II (1:10 dilution), then
24
25
three 5 min washes in PBS and 1 hr with goat anti-rabbit Alexafluor 594 (1:200 dilution)
incubation. Control chondrogenic sections were incubated in 1% BSA without primary
antibody. After secondary incubation, all slides were washed three times for 5 min in
PBS, mounted with Prolong Gold Antifade + DAPI mounting solution (Invitrogen,
Carlsbad, CA) and a coverslip placed.
Fluorescent images were obtained with an
Olympus BX61 microscope (Olympus, Melville, NY).
Flow Cytometry
A total of 2x104 trypsinized MCs were suspended in staining medium (0.1%
sodium azide in PBS) and stained with CD14 (clone M5E2; BD), CD29 (clone
4B4LDC9LDH8; Beckman Coulter, Fullerton, CA), CD34 (clone 563; BD), CD71
(clone DF1513; Ancell, Bayport, MN), CD90 (clone 5E10; BD), and SH3 (American
Type Culture Collection, Manassas, VA) antibodies at room temperature for 20 min.
Cells were gated by their forward- and side-scatter characteristics and to exclude dead
cell debris. Five thousand events were acquired using a FACSCalibur Flow Cytometry
System (Becton, Dickinson and Company, Biosciences, San Diego, CA) and analyzed
with CellQuest software.
Statistical Analysis
Results obtained were reported as the mean ± standard error of the mean (SEM)
and calculated using Microsoft Excel (Microsoft, Redmond, WA). Statistical
26
significance (p<0.05) was determined by analysis of variance (ANOVA) or two-sided
Student’s t-test analysis.
27
RESULTS
Growth of Single MCs
Single human bone marrow-derived MCs expressing EGFP were sorted and
cultured with and without irradiated feeder mesenchymal cells for 13 days. Sorting
efficiency for single cells was 26.8±1.9% of wells in 24 well plates; other wells
contained 0, 2, or 3 EGFP-positive cells. Wells with single EGFP-positive cells were
counted every three days. Based on population doublings (PD), cells were classified into
four groups: high proliferative potential-mesenchymal colony forming cells (HPPMCFCs, > 9 PD, Fig. 2A-D), low proliferative potential-MCFCs (LPP-MCFCs, >6 – 9
PD, Fig. 2E-H), mesenchymal cell clusters (MCCs, > 3 – 6 PD, Fig. 2I-L), and mature
mesenchymal cells (MMCs, ≤ 3 PD, Fig. 2M-P).
Of single cells grown with MC feeders, 7% were HPP-MCFCs (13 colonies/180
single cells plated). LPP-MCFCs, MCCs, and MMCs occurred at a frequency of 29%,
26%, and 38%, respectively (Fig. 3). All LPP-MCFCs, MCCs, and MMCs showed
limited proliferative potential (Fig. 4), increased cytoplasm by 9 days in culture, and
reached senescence during the study (Fig. 2H, L, P). However, HPP-MCFCs continued
to grow and maintained a spindle-shape morphology. Population doubling time of HPPMCFCs (26.2±0.4 hrs) was significantly shorter than conventional heterogeneous adult
bone marrow-derived MSC cultures (50.2±1.6 hrs, p<0.01).
Single MCs cultured
without feeder cells did not grow beyond 6 PD, and the majority of these cells never
28
A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Figure 2. Comparison of Single Mesenchymal Cell Growth with Fluorescence Images.
Images of EGFP expressing cells under fluorescent microscopy obtained on
day 1 (A, E, I, M) post-sorting showing that only a single cell was sorted into
each well. Images of day 3 (B, F, J, N), day 6 (C, G, K, O), and day 9 (D, H,
L, P) show differing growth patterns of the sorted single cells. Four distinct
cell populations were observed in culture; high proliferative potentialmesenchymal colony forming cells (HPP-MCFCs) (A-D), low proliferative
potential-mesenchymal colony forming cells (LPP-MCFCs) (E-H),
mesenchymal cell clusters (MCCs) (I-L), and mature mesenchymal cells
(MMC) (M-P).
29
Figure 3. Comparison of Single Mesenchymal Cell Proliferation After First and Second
Sortings. Percentage of total cells plated on the Y axis, against the level of
growth observed on the X axis. High proliferative potential-mesenchymal
colony forming cells (HPP-MCFCs), low proliferative potentialmesenchymal colony forming cells (LPP-MCFCs), mesenchymal cell clusters
(MCCs), and mature mesenchymal cells (MMCs), were each observed after
both the first and second sorting. Error bars show ±1 standard error of the
mean.
30
Figure 4. Charting Proliferation of Single Mesenchymal Cells Through 13 Days in
Culture. Shown is the total number of cells present in single mesenchymal
cell-derived colonies (Y axis) counted every 3 days for 13 days (X axis). All
low proliferative potential-mesenchymal colony forming cells (LPP-MCFCs),
mesenchymal cell clusters (MCCs), and mature mesenchymal cells (MMCs)
reached senescence within 13 days, whereas high proliferative potentialmesenchymal colony forming cells (HPP-MCFCs) continued to proliferate.
31
divided. Single MCs were also cultured on the basement membrane ECM from decellularized mouse PYS-2 cell culture plates with and without MC feeders in an attempt
to develop a feeder-free culture system [76]. However, PYS-2 cell derived-ECM did not
promote growth of single cells without the presence of MC feeders.
Surface marker expression in conventional MSC culture (Fig. 5A) was not found
to be different from HPP-MCFC (Fig. 5B) when compared by flow cytometry. MCs
were positive for SH3, CD29, CD71, and CD90, and negative for hematopoietic cell
markers CD14, CD34, and CD45.
Differentiation of HPP-MCFCs
HPP-MCFC colonies derived from single MCs were differentiated toward
adipogenic, chondrogenic, and osteogenic lineages and confirmed by Oil Red-O (Fig.
6D), Safranin-O (Fig. 6E), and Von Kossa (Fig. 6F) staining, respectively. To recognize
differentiated HPP-MCFCs from the feeder MCs, cells were stained with antibodies
against PPAR1/2 (adipogenic), COL-II (chondrogenic), and BSP-II (osteogenic). Colocalization of EGFP and PPAR1/2 (Fig. 6G), COL-II (Fig. 6H), or BSP-II (Fig. 6I)
was observed in all cultures. To exclude the possibility of cell fusion, EGFP-positive
MCs were co-cultured with RFP-positive MCs. No cell fusion (yellow cell) events were
observed in all cell cultures examined (data not shown). Although limited proliferation
potential prevented determination of differentiation potential for individual LPP-MCFC,
MCC, and MMC colonies, pooled colonies were differentiated and stained with
32
A
B
Figure 5. Comparison of Surface Marker Expression in Conventional Mesenchymal
Stem Cell Culture and High Proliferative Potential-Mesenchymal Colony
Forming Cells. Bone marrow MSC cultured under routine conditions (A)
and HPP-MCFCs (B) were negative for CD14, CD34, and CD45, and
positive for SH3, CD29, CD71, and CD90 via flow cytometry.
33
Figure 6. Image Verification of Adipogenic, Chondrogenic and Osteogenic
Differentiation of Single Mesenchymal Cell-Derived Colonies. Fluorescence
imaging (A, B, C) verifies EGFP expression along with typical morphology
for differentiated colonies. Positive cellular staining (D, E, F) and colocalization of signal with immunocytochemistry (ICC) (G, H, I) show the
expression of adipogenic (D, G) chondrogenic (E, H) and osteogenic (F, I)
gene expression for all colonies analyzed.
34
antibodies as described above.
Double-stained cells were rare or non-existent for
adipogenic cultures and chondrogenic pellets (MCC and MCC chondrogenic pellets
were not possible to obtain due to low proliferation). However, osteogenic cultures
showed double positive cells for LPP-MCFC, MCC, and MMC colonies (data not
shown).
In order to quantify differentiation between EGFP-positive cells (single cell-derived) and
the feeder MCs, qRT-PCR was performed. Adipogenic, chondrogenic, and osteogenic
cultures were dissociated with trypsin and sorted based on EGFP fluorescence. EGFPpositive cells (single-cell derived) and negative cells (MC feeders) were analyzed for
lineage specific gene expression. Significantly higher expression of adipogenic genes
(PPAR2, LEP, LPL) was observed in EGFP-positive HPP-MCFCs compared to MC
feeders obtained from the same culture induced with adipogenic factors (Fig. 7A).
Interestingly, differences in chondrogenic gene expression (LUM, COMP, BIG) were
not all in the positive direction after differentiation. Similar to adipogenic cultures, all
osteogenic gene expression (CBFA1, IBSP, BGLAP) was observed to be significantly
higher in HPP-MCFC compared to the MC feeders from the same osteogenicdifferentiated culture (Fig. 7C).
Replating Potential of HPP-MCFCs
To investigate replating potential, single cells from single HPP-MCFC-derived colonies
were sorted and re-cultured with MC feeders. As described above, single cells were
35
Figure 7. Pre- and Post-Differentiation qRT-PCR for Adipogenic, Chondrogenic, and
Osteogenic Gene Expression in High Proliferative Potential-Mesenchymal
Colony Forming Cells. Gene expression in high proliferative potentialmesenchymal colony forming cells, relative to the mesenchymal cell feeders
from them same culture (Y axis), is shown before and after adipogenic,
chondrogenic, and osteogenic differentiation (X axis). Error bars show ±1
standard error of the mean.
36
monitored and counted for 13 days and a hierarchy of cells showed different degrees of
self-renewal potential. Compared to the initial distribution where 7% of sorted single
MCs displayed characteristics of HPP-MCFCs, 17% (11 HPP-MCFCs/62 single cells
plated) of single cells in the secondary co-cultures showed greater than 9 PDs (Fig. 3).
Interestingly, the frequencies of LPP-MCFCs and MCCs declined to 16% each (10 HPPMCFCs/62 single cells plated) in secondary culture. However, the frequency of MMCs
increased to 51% (31 HPP-MCFCs/62 single cells plated) in secondary co-cultures
compared to 38% with the initial sorted single MCs. Single HPP-MCFCs gave rise to
11.0±0.2 PDs during the initial expansion, and 10.9±0.3 PDs during the secondary
proliferation period, equivalent to a single cell expanding to 3.8x106±6.6x105 cells.
37
DISCUSSION
With the emergence of MSCs for regenerative medicine and the observed
heterogeneity of conventional MSC culture, it is important to fully discover the potential
and characteristics of these cells. Additionally, the ability to identify and isolate the
optimal target population for regenerative medicine within MSC culture is necessary.
For the first time, this study shows that a single HPP-MCFC from conventional human
bone marrow-derived MSC culture has the potential to proliferate through at least 9
population doublings, generate secondary colonies of HPP-MCFCs, and differentiate
toward adipogenic, chondrogenic, and osteogenic lineages. Also, it has been shown for
the first time that conventional MSC culture contains a hierarchy of cells with differing
proliferative potential, which can only be evaluated by employing a careful single cell
analysis. This analysis offers a quantitative examination of the growth characteristics of
a population of bone marrow-derived MCs and supports previous findings of
heterogeneity within conventional MSC culture [66, 67].
Prior studies describing the characteristics of single bone marrow-derived MCs
employed colony-forming cell isolation techniques that were not ideal, based on the
nature of these cells. Cloning rings allow for migration of cells into or out of the area of
the identified colony forming cell prior to the addition of the ring. Due to the migratory
nature of MCs in culture, it cannot be definitively shown that a MC colony obtained via
the cloning ring technique is truly clonal. Additionally, serial dilution involves the
probability of aliquoting a single cell into a culture well based on a cell count, although
38
ultimately there is no guarantee that only one cell was deposited. With the observed
tendency for MCs to adhere to corners and walls of culture plates where it is often
impossible to identify them under light microscopy due to the optical edge effect (optical
interference produced by the wall of well plates), serial dilution is also not ideal for the
requirements to study single MCs. In support of these assertions, sorted single MCs
showed a trend of adhering at the outer edge of their respective wells; 41% of sorted
cells were observed under fluorescent microscopy to be at or very near to the edge of the
well, and another 34% where visualization would have been difficult under normal light
microscopy. All in all, 75% of sorted cells were affected by the optical edge effect.
In contrast, FACS sorting allows only EGFP-positive cells to be deposited in
culture wells, and any wells in which cells have adhered to the walls can still be
identified and excluded.
Even under the stringent single cell sorting and culture
conditions used in the current study, rare two-cell aggregates were detected after sorting.
Although it is possible that these are identical, newly separated daughter cells, it is not
possible to show conclusively that these cells were in fact, from a single cell except
through use of a lentiviral or retroviral insertional analysis at the genomic level. Thus,
any two-cell aggregates were excluded from this study. By utilizing FACS sorting of
EGFP-transduced cells and interrogation of culture wells under fluorescence microscopy,
the techniques employed in the current study addressed both the migratory and the walladherence issues of single MC isolation.
Importantly, less than 10% of human bone marrow-derived single MCs showed
proliferation potential beyond 9 PD, while nearly 40% of the clones did not go through
39
more than 3 PDs before senescence was observed. While several reports indicate vast
proliferation from adult bone marrow MSCs [9, 52, 67], this study demonstrates that
long-term culture may be established by a small subpopulation of cells within
conventional MSC culture. Under current culture conditions this subpopulation, termed
HPP-MCFCs, undergo asymmetric division and establish a secondary population of
MCs with the full hierarchy of proliferation potential observed in initial culture.
Although the data demonstrates the replating potential HPP-MCFCs, it also indicates
that not all cells in secondary HPP-MCFC culture retain this ability and it may not be
possible to obtain a pure population of HPP-MCFCs with current methods. However,
the possibility remains that this asymmetric division is not obligatory and further
optimization of culture conditions may provide an environment in which secondary
HPP-MCFC colonies retain a more uniform proliferation potential.
Another important observation was that all single bone marrow derived-MCs
required the presence of feeder MCs in order to proliferate to greater than 6 PD.
Attempts to design a feeder-free culture system, including the use of ECM from
decellularized mouse PYS-2 cell culture plates, all resulted in diminished proliferation
and senescence. It is therefore evident that single HPP-MCFCs are unable to recreate
the microenvironment necessary for self-renewal under current culture conditions,
although the necessary cellular constituents do appear to be present within the
heterogeneous population of MCs found in conventional MSC culture. It is also possible
that the feeder MC component of the current culture method contributes to the
asymmetric division observed in secondary HPP-MCFC colonies. Thus, there is a need
40
for further optimization of culture conditions before the self-renewal capacity of HPPMCFCs can be fully described.
Previous reports have indicated the presence of unipotent or bipotent cells in
conventional MSC culture [25, 77], and LPP-MCFC, MCC, and MMC colonies appear
to retain only unipotent or bipotent differentiation capacity. Interestingly, HPP-MCFC
colonies show greater adipogenic and osteogenic differentiation potential when
compared to feeder MCs.
Considering the growth potential of HPP-MCFCs, this
observation may be due to protocols for adipogenic and osteogenic differentiation,
which involve more proliferation during the differentiation period than the chondrogenic
protocol. The inconclusive chondrogenic PCR data (Fig 6B) may also be explained by
the length of time that the pellets were in culture. Pellets were harvested after 21 days in
differentiation medium, whereas the protocol states that they can be harvested from 1421 days. Chondrogenic gene expression may begin to attenuate after 14 days, although
antibody staining showed the presence of extracellular collagen (Fig. 5I) and HPPMCFCs clearly showed tri-lineage differentiation potential. It is important, however, to
note that the data shown in Figure 6 have been normalized with an internal control, and
HPP-MCFCs show greater adipogenic and osteogenic differentiation potential in
comparison to conventional MSC culture. It is also possible that the tripotential balance
of HPP-MCFCs may be disturbed by a variety of culture conditions, with resulting
colonies tending to favor one lineage over another. When considering the complexity of
cytochemical signals and possible intermediate cellular states involved in differentiation,
it may be necessary to optimize culture conditions for single MCs.
41
CONCLUSIONS
Until in vivo data from an appropriate animal model is obtained on the
repopulating potential of HPP-MCFCs, it may still be premature to proclaim the
existence of a true MSC. However, HPP-MCFCs meet both basic requirements for
designation as stem cells (self-renewal capacity and differentiation potential) in vitro,
and are of interest for further characterization. While these cells are not pluripotent and
are not likely candidates for studies involving endodermal or ectodermal development,
they can be harvested from adult tissues and are not associated with the ethical dilemmas
of hESCs; no embryos need be destroyed to obtain the cells and the direct formation of
tumors by cells from MSC culture has not been reported in humans or nonhuman
primate models after transplantation. Although MSCs’ ability to migrate toward sites of
inflammation and induce angiogenesis has led to the suggestion of a role in support of
solid epithelial tumor growth, this association has not been fully examined and has not
been an issue in any clinical studies thus far.
Ideally, a cell surface marker will be found that allows for isolation of HPPMCFCs from MSC culture. Since this population of cells within MSC culture retain
both the highest proliferation potential and most efficient differentiation, HPP-MCFCs
are likely candidates for further transplantation studies.
Transplanted HPP-MCFC
populations will have greater proliferation capabilities and may persist longer and
provide added therapeutic value when compared to a heterogeneous MSC population.
For example, in studies where an unoccupied niche is not readily available or
42
inflammation is not present, successful engraftment and persistence may be rare events
for transplanted cells [33]. Utilizing HPP-MCFCs instead of a heterogeneous MSC
population for transplantation may increase the probability that any cell which is able to
successfully engraft would persist, proliferate, and either differentiate or express a
designed transgene as needed for a particular disease state.
When the other characteristics associated with MSC culture are considered for
HPP-MCFCs (e.g., immune modulation, support of co-transplanted cells, no need for
HLA matching, and banking prior to use) it is conceivable that HPP-MCFCs could
become a helpful tool in many different types of transplantation studies. However,
further characterization is necessary for this possibility to become a reality. It will be
critical to investigate the in vivo properties of HPP-MCFCs if they are to be considered
for future clinical trials.
In addition, determining the potential of HPP-MCFCs to
differentiate toward lineages other than those included in this study, such as myogenic
lineages, may be valuable.
The experiments performed in this thesis provide evidence for the first time that a
hierarchy of MCs can be described within conventional MSC culture. The potential for
proliferation and formation of secondary colonies, as well as efficiency of differentiation
toward adipogenic, chondrogenic, and osteogenic lineages were shown to be greatest in
a minority population of cells termed HPP-MCFCs. As further characterization of the
therapeutic properties of cells from MSC culture is achieved, studies performed at the
single cell level will be essential for providing both quantitative and qualitative data for
identifying and isolating the ideal population of cells for transplantation.
43
LITERATURE CITED
1.
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall
VS, and Jones JM. Embryonic stem cell lines derived from human blastocysts.
Science 282:1145-1147, 1998.
2.
Murry CE and Keller G. Differentiation of embryonic stem cells to clinically
relevant populations: lessons from embryonic development. Cell 132:661-680,
2008.
3.
Jensen J, Hyllner J, and Björquist P. Human embryonic stem cell technologies
and drug discovery. J Cell Physiol 219:513-519, 2009.
4.
Byrne JA, Mitalipov SM, and Wolf DP. Current progress with primate
embryonic stem cells. Curr Stem Cell Res Ther 1:127-138, 2006.
5.
Hynes RO. US policies on human embryonic stem cells. Nat Rev Mol Cell Biol
9:993-997, 2008.
6.
Ford CE, Hamerton JL, Barnes DWH, and Loutit JF. Cytological identification
of radiation-chimaeras. Nature 177:452-454, 1956.
7.
Srour EF and Yoder MC. Flow cytometric analysis of hematopoietic
development. Methods Mol Med 105:65-80, 2005.
8.
Alhadlaq A and Mao JJ. Mesenchymal Stem Cells: Isolation and Therapeutics.
Stem Cells Dev 13:436-448, 2004.
44
9.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD,
Moorman MA, Simonetti DW, Craig S, and Marshak DR. Multilineage potential
of adult human mesenchymal stem cells. Science 284:143-147, 1999.
10.
Kon E, Muraglia A, Corsi A, Bianco P, Marcacci M, Martin I, Boyde A,
Ruspantini I, Chistolini P, Rocca M, Giardino R, Cancedda R, and Quarto R.
Autologous bone marrow stromal cells loaded onto porous hydroxyapatite
ceramic accelerate bone repair in critical-size defects of sheep long bones. J
Biomed Mater Res 49:328-37, 2000.
11.
Horwitz EM, Prockop DJ, and Fitzpatrick LA. Transplantability and therapeutic
effects of bone marrow-derived mesenchymal cells in children with osteogenesis
imperfecta. Nat Med 5:309–313, 1999.
12.
Lee CI, Kohn DB, Ekert JE, and Tarantal AF. Morphological analysis and
lentiviral transduction of fetal monkey bone marrow-derived mesenchymal stem
cells. Mol Ther 9:112-23, 2004.
13.
Song L, Webb NE, Song Y, and Tuan RS. Identification and Functional Analysis
of Candidate Genes Regulating Mesenchymal Stem Cell Self-Renewal and
Multipotency. Stem Cells 24:1707-1718, 2006.
14.
Ball LM, Bernardo ME, Locatelli F, and Egeler RM. Potential role of
mesenchymal stromal cells in pediatric hematopoietic SCT. Bone Marrow
Transplant 42:S60–S66, 2008.
15.
Chen FH and Tuan RS. Mesenchymal stem cells in arthritic diseases. Arthritis
Res Ther 10:223(doi:10.1186/ar2514), 2008.
45
16.
Hare JM and Chaparro SV. Cardiac regeneration and stem cell therapy. Curr
Opin Organ Transplant 13:536–542, 2008.
17.
Nesselmann C, Ma N, Bieback K, Wagner W, Ho A, Konttinen YT, Zhang H,
Hinescu ME, and Steinhoff G. Mesenchymal stem cells and cardiac repair. J Cell
Mol Med 12:1795-1810, 2008.
18.
Hopkins C, Li J, Rae F, and Little MH. Stem cell options for kidney disease. J
Pathol 217:265–281, 2009.
19.
Fu XB, Fang LJ, Li XK, Cheng B, and Sheng ZY. Enhanced wound-healing
quality with bone marrow mesenchymal stem cells autografting after skin injury.
Wound Repair Regen 14:325–335, 2006.
20.
Crevensten G, Walsh AJ, Ananthakrishnan D, Page P, Wahba GM, Lotz JC, and
Berven S. Intervertebral disc cell therapy for regeneration: mesenchymal stem
cell implantation in rat intervertebral discs. Ann Biomed Eng 32:430–434, 2004.
21.
García-Castro J, Trigueros C, Madrenas J, Pérez-Simón JA, Rodriguez R, and
Menendez P. Mesenchymal stem cells and their use as cell replacement therapy
and disease modeling tool. J Cell Mol Med 12(6B):2552-2565, 2008.
22.
http://www.clinicaltrials.gov, 2009.
23.
Alsberg E, von Recum HA, and Mahoney MJ. Environmental cues to guide stem
cell fate decision for tissue engineering applications. Expert Opin Biol Ther
6:847-866, 2006.
46
24.
Prockop DJ. Marrow stromal cells as stem cells for continual renewal of
nonhematopoietic tissues and as potential vectors for gene therapy. J Cell
Biochem Suppl 30-31:284-285, 1998.
25.
Mareddy S, Crawford R, Brooke G, and Xiao Y. Clonal isolation and
characterization of bone marrow stromal cells from patients with osteoarthritis.
Tissue Eng 13:819-829, 2007.
26.
Gaspar
BH
and
Thrasher
AJ.
Gene
therapy
for
severe
combined
immunodeficiencies. Expert Opin Biol Ther 5:1175-1182, 2005.
27.
Reiser J, Zhang XY, Hemenway CS, Mondal D, Pradhan L, and La Russa VF.
Potential of mesenchymal stem cells in gene therapy approaches for inherited and
acquired diseases. Expert Opin Biol Ther 5:1571-1584, 2005.
28.
Lee K, Majumdar MK, Buyaner D, Hendricks JK, Pittenger MF, and Mosca JD.
Human mesenchymal stem cells maintain transgene expression during expansion
and differentiation. Mol Ther 3:857-866, 2001.
29.
Kraitchman DL, Tatsumi M, Gilson WD, Ishimori T, Kedziorek D, Walczak P,
Segars WP, Chen HH, Fritzges D, Izbudak I, Young RG, Marcelino M, Pittenger
MF, Solaiyappan M, Boston RC, Tsui BM, Wahl RL, and Bulte JW. Dynamic
imaging of allogeneic mesenchymal stem cells trafficking to myocardial
infarction. Circulation 112:1451-1461, 2005.
30.
Torrente Y and Pollie E. Mesenchymal stem cell transplantation for
neurodegenerative diseases. Cell Transplant 17:1103-1113, 2008.
47
31.
Stich S, Haag M, Häupl T, Sezer O, Notter M, Kaps C, Sittinger M, and Ringe J.
Gene expression profiling of human mesenchymal stem cells chemotactically
induced with CXCL12. Cell Tissue Res DOI 10.1007/s00441-009-0768-z, 2009.
32.
Rosova I, Dao M, Capoccia B, Link D, and Nolta JA. Hypoxic Preconditioning
Results in Increased Motility and Improved Therapeutic Potential of Human
Mesenchymal Stem Cells. Stem Cells 26:2173–2182, 2008.
33.
Sasportas LS, Kasmieh R, Wakimoto H, Hingtgen S, van de Water JA,
Mohapatra G, Figueiredo JL, Martuza RL, Weissleder R, and Shah K..
Assessment of therapeutic efficacy and fate of engineered human mesenchymal
stem cells for cancer therapy. Proc Natl Acad Sci DOI 10.1073/ pnas.0806647106,
2009.
34.
Almeida-Porada G, Flake AW, Glimp HA, and Zanjani ED. Cotransplantation of
stroma results in enhancement of engraftment and early expression of donor
hematopoietic stem cells in utero. Exp Hematol 27:1569–1575, 1999.
35.
Ringdén O, Uzunel M, Sundberg B, Lönnies L, Nava S, Gustafsson J,
Henningsohn L, and Le Blanc K. Tissue repair using allogeneic mesenchymal
stem cells for hemorrhagic cystitis, pneumomediastinum and perforated colon.
Leukemia 21:2271-2276, 2007.
36.
Le Blanc K and Pittenger M. Mesenchymal stem cells: progress toward promise.
Cytotherapy 7:36-45, 2005.
48
37.
Chen J, Li Y, Wang L, Lu M, Zhang X, and Chopp M. Therapeutic benefit of
intracerebral transplantation of bone marrow stromal cells after cerebral ischemia
in rats. J Neurol Sci 189:49-57, 2001.
38.
Li Y, Chen J, Zhang CL, Wang L, Lu D, Katakowski M, Gao Q, Shen LH,
Zhang J, Lu M, and Chopp M. Gliosis and brain remodeling after treatment of
stroke in rats with marrow stromal cells. Glia 49:407-417, 2005.
39.
Nakagami H, Maeda K, Morishita R, Iguchi S, Nishikawa T, Takami Y, Kikuchi
Y, Saito Y, Tamai K, Ogihara T, and Kaneda Y. Novel autologous cell therapy in
ischemic limb disease through growth factor secretion by cultured adipose tissuederived stromal cells. Arterioscler Thromb Vasc Biol 25:2542-2547, 2005.
40.
Kim SW, Han H, Chae GT, Lee SH, Bo S, Yoon JH, Lee YS, Lee KS, Park HK,
and Kang KS. Successful stem cell therapy using umbilical cord blood-derived
multipotent stem cells for Buerger's disease and ischemic limb disease animal
model. Stem Cells 24:1620-1626, 2006.
41.
Tang J, Xie Q, Pan G, Wang J, and Wang M. Mesenchymal stem cells participate
in angiogenesis and improve heart function in rat model of myocardial ischemia
with reperfusion. Eur J Cardiothorac Surg 30:353-361, 2006.
42.
Makino S, Fukuda K, Miyoshi S, Konishi F, Kodama H, Pan J, Sano M,
Takahashi T, Hori S, Abe H, Hata J, Umezawa A, and Ogawa S.
Cardiomyocytes can be generated from marrow stromal cells in vitro. J Clin
Invest 103:697-705, 1999.
49
43.
Toma C, Pittenger MF, Cahill KS, Byrne BJ, and Kessler PD. Human
mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult
murine heart. Circulation 105:93-98, 2002.
44.
Li W, Ma N, Ong LL, Nesselmann C, Klopsch C, Ladilov Y, Furlani D,
Piechaczek C, Moebius JM, Lutzow K, Lendlein A, Stamm C, Li RK, and
Steinhoff G. Bcl-2 engineered MSCs inhibited apoptosis and improved heart
function. Stem Cells 25:2118-2127, 2007.
45.
Martin-Rendon E, Sweeney D, Lu F, Girdlestone J, Navarrete C, and Watt SM.
5-Azacytidine-treated human mesenchymal stem/progenitor cells derived from
umbilical cord, cord blood and bone marrow do not generate cardiomyocytes in
vitro at high frequencies. Vox Sang 95:137-148, 2008.
46.
Devine SM, Bartholomew AM, Mahmud N, Nelson M, Patil S, Hardy W,
Sturgeon C, Hewett T, Chung T, Stock W, Sher D, Weissman S, Ferrer K, Mosca
J, Deans R, Moseley A, and Hoffman R. Mesenchymal stem cells are capable of
homing to the BM of non-human primates following systemic infusion. Exp
Hematol 29:244–255, 2001.
47.
Horwitz EM, Gordon PL, Koo WK, Marx JC, Neel MD, McNall RY, Muul L,
and Hofmann T. Isolated allogeneic BM-derived mesenchymal cells engraft and
stimulate growth in children with osteogenesis imperfecta: implications for cell
therapy of bone. Proc Natl Acad Sci U S A 99:8932–8937, 2002.
50
48.
Le Blanc K, Rasmusson I, Sundberg B, Gotherstrom C, Hassan M, Uzunel M,
and Ringden O. Treatment of severe acute graft-versus-host disease with third
party haploidentical mesenchymal stem cells. Lancet 36:1439–1441, 2004.
49.
Aggarwal S and Pittenger MF. Mesenchymal stem cells modulate allogeneic
immune cell responses. Blood 105:1815-1822, 2005.
50.
Nauta AJ and Fibbe WE. Immunomodulatory properties of mesenchymal stromal
cells. Blood 110:3499-3506, 2007.
51.
Lee CC, Ye F, and Tarantal AF. Comparison of growth and differentiation of
fetal and adult rhesus monkey mesenchymal stem cells. Stem Cells Dev 15:20920, 2006.
52.
Hacia JG, Lee CC, Jimenez DF, Karaman MW, Ho VV, Siegmund KD, and
Tarantal AF. Age-related gene expression profiles of rhesus monkey bone
marrow-derived mesenchymal stem cells. J Cell Biochem 103:1198-210, 2008.
53.
Tuan RS, Boland G, and Tuli R. Adult mesenchymal stem cells and cell-based
tissue engineering. Arthritis Res Ther 5:32–45, 2003.
54.
Cetrulo CL Jr. Cord-blood mesenchymal stem cells and tissue engineering. Stem
Cell Rev 2:163–168, 2006.
55.
Verrie S, Meury T, Lipross S, and Alini M. An engineered vascularized graft for
large bone defect. Eur Cell Mat 13:38, 2007.
56.
Vermeulen L, Sprick MR, Kemper K, Stassi G, and Medema JP. Cancer stem
cells – old concepts, new insights. Cell Death Differ 15:947–958, 2008.
51
57.
Riggi N, Cironi L, Provero P, Suvà ML, Stehle JC, Baumer K, Guillou L, and
Stamenkovic I. Expression of the FUS-CHOP fusion protein in primary
mesenchymal progenitor cells gives rise to a model of myxoid liposarcoma.
Cancer Res 66:7016–7023, 2006.
58.
Riggi N, Cironi L, Provero P, Suvà ML, Kaloulis K, Garcia-Echeverria C,
Hoffmann F, Trumpp A, and Stamenkovic I. Development of Ewing’s sarcoma
from primary BM-derived mesenchymal progenitor cells. Cancer Res 65:11459–
11468, 2005.
59.
Matushansky I, Hernando E, Socci ND, Matos T, Mills J, Edgar MA, Schwartz
GK, Singer S, Cordon-Cardo C, and Maki RG. A developmental model of
sarcomagenesis defines a differentiation-based classification for liposarcomas.
Am J Pathol 172:1069–1080, 2008.
60.
Mishra PJ, Mishra PJ, Glod JW, and Banerjee D. Mesenchymal stem cells: flip
side of the coin. Cancer Res 69:1255-1258, 2009.
61.
Bernardo ME, Zaffaroni N, Novara F, Cometa AM, Avanzini MA, Moretta A,
Montagna D, Maccario R, Villa R, Daidone MG, Zuffardi O, and Locatelli F.
Human BM derived mesenchymal stem cells do not undergo transformation after
long-term in vitro culture and do not exhibit telomere maintenance mechanisms.
Cancer Res 67:9142–9149, 2007.
62.
Izadpanah R, Kaushal D, Kriedt C, Tsien F, Patel B, Dufour J, and Bunnell BA.
Longterm in vitro expansion alters the biology of adult mesenchymal stem cells.
Cancer Res 68:4229–4238, 2008.
52
63.
Senseb L, Bourin P, and Douay L. Good Manufacturing Practices: Clinical-Scale
Production of Mesenchymal Stem Cells. Stem Cell Transplant DOI
10.1002/3527608745.ch6, 2006.
64.
Kim BS, Lee CC, Christensen JE, Huser TR, Chan JW, and Tarantal AF. Growth,
differentiation, and biochemical signatures of rhesus monkey mesenchymal stem
cells. Stem Cells Dev 17:185-98, 2008.
65.
Friedstein, AJ, Chailakhjan RK, and Lalykina KS.
The development of
fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen
cells. Cell Tissue Kinet 3:393-403, 1970.
66.
Colter DC, Sekiya I, and Prockop DJ. Identification of a subpopulation of rapidly
self-renewing and multipotential adult stem cells in colonies of human marrow
stromal cells. Proc Natl Acad Sci 98:7841-7845, 2001.
67.
Prockop DJ, Sekiya I, and Colter DC. Isolation and characterization of rapidly
self-renewing stem cells from cultures of human marrow stromal cells.
Cytotherapy 3:393-396, 2001.
68.
Simmons PJ and Torok-Storb B. Identification of stromal cell precursors in
human bone marrow by a novel monoclonal antibody, STRO-1. Blood 1:55-62,
1991.
69.
Anjos-Afonso F and Bonnet D. Nonhematopoietic/endothelial SSEA-1_ cells
define the most primitive progenitors in the adult murine BM mesenchymal
compartment. Blood 109:1298–1306, 2007.
53
70.
Gang EJ, Bosnakovski D, Figueiredo CA, Visser JW, and Perlingeiro RC. SSEA4 identifies mesenchymal stem cells from BM. Blood 109:1743–1751, 2007.
71.
McNiece IK, Bertoncello I, Kriegler AB, and Quesenberry PJ. Colony-forming
cells with high proliferative potential (HPP-CFC). Int J Cell Cloning 8:146-160,
1990.
72.
Yoder MC, Du XX, and Williams DA. High proliferative potential colonyforming cell heterogeneity identified using counterflow centrifugal elutriation.
Blood 82:385-391, 1993.
73.
Bradley TR and Hodgson GS. Detection of primitive macrophage progenitor
cells in mouse bone marrow. Blood 54:1446-1450, 1979.
74.
Srour EF, Brandt JE, Briddell RA, Grigsby S, Leemhuis T, and Hoffman R.
Long-term generation and expansion of human primitive hematopoietic
progenitor cells in vitro. Blood 81:661-669, 1993.
75.
Ingram DA, Mead LE, Moore DB, Woodard W, Fenoglio A, and Yoder MC.
Vessel wall-derived endothelial cells rapidly proliferate because they contain a
complete hierarchy of endothelial progenitor cells. Blood 105:2783-2786, 2005.
76.
Matsubara T, Tsutsumi S, Pan H, Hiraoka H, Oda R, Nishimura M, Kawaguchi
H, Nakamura K, and Kato Y. A new technique to expand human mesenchymal
stem cells using basement membrane extracellular matrix. Biochem Biophys Res
Commun 313:503-508, 2004.
77.
Owen, M. Marrow stromal stem cells. J Cell Sci 10:63-76, 1988.