medical management
advertisement

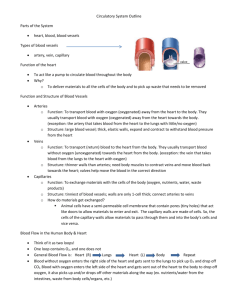
OCCULUSIVE DISORDERS: ARTERIOSCLEROSIS, ANGINA, MI ARTERIOSCLEROSIS: Narrowing of arteries or hardening of arteries caused by a buildup of lipids, collagen & smooth muscle cells. Blood flow through is decreased causing decreased perfusion to body cells. One type of Arteriosclerosis is Arthrosclerosis ATHROSCLEROSIS: plaque formation or fatty deposits on the linings of the major arteries. ANGINA PERTORIS: (or Myocardial Ischemia) When coronary arteries lose elasticity & become narrowed due to plaque formation, the heart muscle receives less blood & oxygen. It is a temporary inadequate blood supply to myocardial tissue. 5 E’s precipitate: Eating a healthy meal Exercise Exertion Emotional stress Exposure to extreme temperature Also, smoking & arterial spasms SIGNS & SYMPTOMS: Squeezing pain lower sternum that radiates to left shoulder, also to right shoulder, jaw, & ear. The symptoms increase in frequency & severity over time Severity depends on amount of collateral circulation -collateral circulation: shunting of blood from narrowed larger vessels to surrounding smaller vessels. DIAGNOSTIC TESTS: Patient history Stress test (thallium) Laboratory test- HDL, LDL Coronary Arteriogram TREATMENTS: Rest Vasodilatation (NTG) 3 NTG 15min apart Surgical -PTCA: percutaneious transluminal coronary angioplasty, “balloon surgery” -Stent: implanted into stenosed vessel, preventing it from collapsing. Balloon is used then removed & stent left in place. COMPLICATION: If piece of plaque breaks off & occludes artery CABG surgery is needed. CABG: The internal mammary artery, saphenous vein or synthetic graft is grafted to the aorta & passed beyond the occlusion in the coronary vessel. Meds: NTGvasodilation beta blockers calcium channel blockers low fat, low cholesterol, NA restricted rest periods limit fat to 30g a day exercise 3-5 times week for at least 20min MYOCARDIAL INFARCTION: leading cause of sudden death of men & women MI: obstruction in the coronary artery resulting in death (necrosis) to the tissue supplied to the artery. (first 24 hours are most crucial time) CAUSE: Atherosclerosis, thrombus, embolism Most common: atherosclerosis Most commonly affected is left ventricle If a large coronary artery is obstructed & client does not have sufficient collateral circulation client may die immediately, “massive MI” NORMAL: LDH2 is normally higher than LDH1: after MI it flips LDH1 (which is specific to cardiac muscle tissue) is higher than LDH2 SYMPTOMS: Chest pain (heaviness, tightness) Low sternal pain Pain NOT relieved by NTG S.O.B- diaphoresis – anxious Nausea & vomiting Pulse irregular, rapid, & weak BP drops Skin pale then cyanotic DIAGNOSES: Cardiac isoenzymes (CPU MB LDH) EKG Radioactive isotropic scan First 3 days after infarction- s/s low grade fever, elevated WBCs 4-7 days: infarct tissue softest & weakest Collateral circulation may take as long as 2-3 weeks after 2-3 months muscle will regain strength MEDICAL MANAGEMENT: Reduce workload of heart. In ICU on monitor 3 dysrthymias may occur after V-fib Bradycardia (atropine) Tachycardia (lanoxin) 2 types: A-fib (lanoxin) V-tach (lidocaine or cardioversion) SURGICAL MANAGEMENT: PTCA- percutaneous transluminal coronary angioplasty CABG PHARMALOGICAL: Oxygen Morphine for pain Nitrates (IV or Sublingual) Sedatives Stool softener Thrombolytic Therapy (within 3-6 hours of infarct) dissolves clot Streptolsinase Eminase Activase Complication: bleed. Nursing intervention: monitor amesis/tarry stools Heparin therapy (ASA usually not given with heparin) ASA to prevent vasoconstriction DIET: Acute stage: clear liquids (reduce workload of heart) progressed to low sodium –low fat –low cholesterol Avoid caffeine, extreme hot/cold foods ACTIVITY: Decrease workload of heart. First 24 hours bedrest Stress test prior to discharge to determine activity level HEALTH PROMOTION: Proper diet, exercise, stop smoking, cardiac rehab program, esp for women because women have worse prognosis than men. CONGESTIVE HEART FAILURE: weakened muscle that cannot meet metabolic needs of body. Can be right or left sided RIGHT SIDED: Congestion in inferior vena cavaedema in extremities then in trunk of body (edema in ankles, thighs,& abdomen) Enlarged liver & enlarged spleen Distended neck veins Oliguria LEFT SIDED: blood backs up left ventricle, left atrium & pulmonary veins lungs become crystallized (patient cyanotic, spits up blood, dyspnea, restlessness) moist respirations (crackles on auscultations) tachy decreased BP decreased urinary output confusion as blood oxygen level decreases GOAL MEDICAL MANAGEMENT: Improve circulation to coronary arteries & reduce workload of left ventricles TREATMENT: Oxygen Bedrest with HOB elevated Diuretics (lasix) restrict fluid, daily weights, measure abdominal girth Digatalis-strengthens contraction of heart muscle SUGICAL INTERVENTIONS: Intra-aortic balloon Ventricular assist device Cardiomyopathy PHARMOLOGICAL: Diurel Lasix Vasodilators NTG ACE inhibitors-angiotension converting enzyme, to reduce BP & peripheral resistance & improve cardiac output ie Capoten & Vasotec Morphine Sulfate (if pain) during acute phase to reduce anxiety DIET: Limit fluid intake Lo NA Daily weight ACTIVITY: Varies from bedrest with HOB elevated to ambulatory HEALTH PROMOTION: Low-fat diet high fiber diet calorie balance Regular exercise program Stress reduction program COR PULMONALE: heart is affected because of lung condition that interferes with CO2 & O2 exchange pulmonary artery vasoconstriction pulmonary hypertension. Right ventricle pumps against pulmonary pressure & enlarges & weakens in an attempt to pump blood into the lungs. SIGNS & SYMPTOMS: Same as right sided heart failure CARDIAC TRANSPLANTATION: who? Cardiomyopathy End-stage CAD Valvular disease Heart donor must be compatible with recipient Recipient is on immunosuppressant’s: Imuran, ATG, Sandimmuine etc PERIPHERAL VASCULAR DISORDERS: Venous Thrombus/Thrombophlebitis: Phlebitis=inflammation of the wall of the vein without clot Thrombophlebitis=inflammation of the wall of the vein with a clot 3 factors cause the formation of a clot: Pooling of blood Vessel trauma Problem with coagulation RISK FACTORS: Prolonged bedrest Leg trauma Oral contraceptives Obesity Varicose veins Hip fracture Total hip/knee replacement 2 TYPES OF THROMBI: Superficial thrombus DVT CAUSE: Trauma to vein (IVs) DIAGNOSTIC TEST: Venous Doppler SIGNS & SYMPTOMS: Reddened streak over skin Warmth & tenderness at site Unilateral edema of affected extremity Positive Homans sign Complaints that leg feels tight or heavy COMPLICATION: PE S/S sudden chest pain Dyspnea Tachypnea MEDICAL MANAGEMENT: Warm compresses NSAIDs Elevate extremity Support hose Bedrest SURGICAL MANAGEMENT: Tromblectomy: removal of clot Greenfield vena cava filter or umbrella filter= placed in inferior vena cava to prevent traveling clot from lower extremities to the lungs, heart, or brain PHARMALOGICAL: If a client is at risk for Thrombus, anticoagulant therapy can be initiated. Prophalatic Heparin Levenox- lo-molecular weight heparin used prophylactic ally after hip replacement surgery If clot: Patient is placed on IV heparin PTT before to establish baseline & regulate dose Later Coumadin (po) (3-6 months) MASSIVE DVT DRUGS: Streptokinase Urokinase *observe for bleeding with patients on anticoagulants & avoid ASA* DIET: Adequate hydration 2-3 quarts per day HEALTH PROMOTION: Early ambulation Prophylactic anticoagulants Elevate legs Deep breathing exercises Avoid sitting or standing for long periods of time Wear support hose Don’t sit with legs crossed VARICOSE VEINS: Varicosities are visibly prominent, dilated & twisted veins. Veins most affected are lower extremities Others include esophageal varices Hemorrhoids *women are more prone than men* RISK FACTOR: Familial tendency Congenital abnormalities Pregnancy Constrictive clothing Occupations that require periods of prolonged standing CAUSES: Incomplete absent valves & veins that lost elasticity Wall of vein of weakened MEDICAL Rx: Elastic support hose Elevate legs when sitting (don’t cross them) Ankle & leg exercises Sclerotherapy- sclerosing the vein so blood doesn’t flow through. Elastic stockings 4-5 days after, support hose 5 weeks or more. COMPLICATIONS: Necrosis at injection site Vasospasms Allergic response Hemolysis (destruction of RBCs) SURGICAL TREATMENT; Vein legation: tie off vein Vein stripping: stripping the walls of the vein Post Op: bedrest 24 hours, elastic stockings (5days), pain meds 30 min before the client ambulates PHARMOCOLOGICAL: Analgesics Anticoagulants ACTIVITY: Regular exercise Walking improves circulation Ankle exercises (rotating ankle) HEALTH PROMOTION: Encourage to elevate legs 6-10 inches when sitting Frequent position changes- not standing in 1 spot for long periods of time. NURSING MANAGEMENT: Elevate legs when sitting Read nursing management for patients with vein stripping & scliotherapy. BUERGERS DISEASE: inflammatory disease of small & medium arteries & veins that leads to vascular obstruction. It effects hands & feet & can also effect wrists & lower extremities. SIGNS & SYMPTOMS: Distal tip of hands & feet are pale As disease progresses hands & feet become reddened when held in dependant position. Pain in palm of hand & arch of foot Numbness, burning pain at rest Decreased sensation in hands & lower extremities Weak or absent pulses Skin color changes Sensitivity to cold Ulcers & gangrene in later stages Occurs between ages 20-40 There is a correlation with smoking MEDICAL TREATMENT: Stop smoking you people Buerger Allen excercises: -elevate leg until the blanch support them 2-3 minutes -lower the legs until they become red for 5-10 minutes -legs placed flat on bed with client supine for 10 minutes -repeat exercises as tolerated SURGICAL TREATMENT: Sympathectomy: excision of a segment of a sympathetic nerve to relieve pain & prevent vasospasms in the affected area. PHARMOCOLOGICAL: Analgesics to control pain Vasodilators to increase circulation to the affected area NURSING MANAGEMENT: Stop smoking Avoid exposure to cold, repetitive hand movements, & stressful situations Encourage stress management SECONDARY RAYNAUDS: is associated with connective tissue or collagen vascular disease, meds, or occupational trauma. RAYNAUDS OR PRIMARY RAYNAUDS: intermittent spasms of the digital arteries & arterioles that results in decreased circulation to fingers & toes. It sometimes affects tip of nose & ears. During a spasm that lasts 15 minutes, fingers become pale then cyanotic. As circulation returns fingers & fingertips become reddened & person experiences tingling or throbbing pain in the fingers Some people experience pallor & cyanosis Episode lasts 1-2 hours Exposure to cold, emotional stress triggers an attack MANIFESTATION: Affects (w) between 16-40 years Affects people that have occupations that require repetitive movements of hands or persons exposed to vinyl chloride DIAGNOSTIC: CBC, digital BP measurement & cold challenge test Cold challenge test: hands are placed in ice water for 20 seconds, temp of hand is taken q5 minutes until it returns to baseline Sed-rate –ANA- rheumatoid factor to determine presence of autoimmune disease MEDICAL MANAGEMENT: Medication: adulate, procardia, cardezem, calan, cardene, capoten For finger ulcers: cipro For digital ulcers: trental (decreases blood viscosity & improves blood flow) HEALTH PROMOTION: Avoid exposure to cold, repetitive, hand movement & stressful situations Quit smoking you people, avoid second hand smoke Stress management ANEURYSM: bulge or dilation of a weakened section of an artery. CAUSE: Main cause is atherosclerosis Lack of elasticity in arterial wall AAA heredity (Marfins Syndrome) Congenital conditions Trauma to vessel wall Infection/inflammation Syphilis At risk: smokers & hypertension Increased turbulence in the vessel Slow production of smooth muscle cells Incidence: AAA seen in male between ages 60-70 SYMPTOMS: Depends on location Asymptomatic until they leak or pressure on structure Upper back pain Deep scattered chest pain Dyspnea Cough Wheezing DIANGNOSTIC: X-rays MEDICAL MANAGEMENT: Rupture is emergency s/s: decreased BP, tachy, paleness, weakness, pain in back abdomen & groin. SURGICAL MANAGEMENT: Doppler U.S. to evaluate perphial vessels Cardiac workup Angiogram Have 4-8 units of blood available SURGERY: Synthetic graft after removal of portion of involved vessel COMPLICATION: MI, stroke, renal damage, after surgery patient placed in ICU on respirator PHARM MANAGEMENT: Inderol Symptomatic (antihypertensions) Analgesics ACTIVITY: Avoid activity that increases pressure on arteries HEALTH PROMOTION: Stop smoking Closely monitor BP Compliance with medical regimen HYPERTENSION: 140/90 or higher is indicative Prior to 55 more men, after 55 more women RISK FACTORS: Family history Smoking Obesity Lack of exercise Diabetes Poor education Low socioeconomic status Primary or Essential Hypertension: when cause is unknown Secondary Hypertension: when cause is related to another condition CAUSE: Renal : decreased blood flow to kidneys causes release of RENIN. When rennin is released it interacts with plasma protein & forms vasopessor called angio tension that causes vasoconstriction that leads to increased peripheral resistance. Arteriosclerosis/Athrosclerosis: narrows vessel lumen because of plaque formation increased resistance to blood flow & more pressure is needed to get blood through. Stress: stimulates the sympathetic nervous system that supplies nerves to smooth muscle that lines the arteries. Stimulation of smooth muscle vasoconstriction HTN Hypernatremia: causes vasocongestion heart must pump with more force. COMPLICATIONS OF HTN: MI Stroke CHF MEDICAL MANAGEMENT: Change in diet & lifestyle (weight loss, limit NA in diet, limit fat, cholesterol, & apple martinis) Stop smoking Maintain adequate calcium & magnesium Add a diuretic or beta blocker to regimen (2 months) If BP still 140/90 try another drug or add another diuretic (if BP is still 140/90 or higher try adding a second or third hypertensive PHARM MANAGEMENT: First start with diuretics, decrease fluid volume Beta blockers ACE inhibitors Calcium Channel Blockers Direct vasodilates Adrenergic antagonists Alpha receptor blockers DIET: Low fat, low cholesterol, low NA Avoid processed foods, carbonated drinks, & cereals Adequate intake of vitamin K, magnesium, & calcium Alcohol: 2oz of alcohol no more than twice a week