KEY Cardiovascular Study Guide Isengard
advertisement

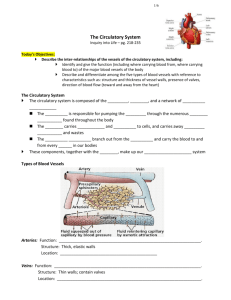
KEY Cardiovascular Study Guide Isengard-Anatomy CP Learning Objectives: RBC & WBC Formation (Red Blood Cell terms, reticulocyte, granulocyte, myeloid stem cells) Red blood cells are formed with reticulocytes. They originate in bone marrow and will be recycled in the spleen. Various hormones are required for RBC formation. Erythropoeitin is one of the main hormones. -White Blood Cells are categorized as granulocytes or agranulocytes (possessing no granules). Most WBCs arise from myeloid stem cells with the exception of the lymphocytes. Granulocytes include neutrophils, eosinophils & basophils Agranulocytes are the monocytes ,lymphocytes Steps of Hemostasis (Blood Stoppage) 1) Vascular Spasms (Serotonin Secretion) 2) Platelet Plug- Prothrombin Activator-forms plug 3) Fibrinogen will generate fibrin ( a tissue that will cover the injury) Steps of Clotting Cascade (Diagram these steps below) Prothrombin, Thrombin, etc. http://memorize.com/blood-human-anat-and-phys-7th-ed-marieb Name the hormones responsible for producing: Erythrocytes-Erythropoeitin Leukocytes-Interleukins &Colony Stimulating Factors (CSFs) Platelets-Thrombopoeitin Distinguish the differences between antibodies and antigens. Antigens are markers that identify the blood type as a person’s own(for example, Type A blood would possess A antigens. Antibodies are generated as an immune response to protect blood from foreign agents. For example,Type A blood would produce B antibodies and vice versa. Identify these in the table below List the steps of the cardiac cycle f c d e a e a h g g b b b 1. Location and Size Use the letters to label the heart image above a. Atria (2) e. Pulmonary Veins b. Ventricles (2) f. Aorta c. Sup. and Inf. d. Pulmonary Vena Trunk g. (AV) Valves (What are their names & how many flaps are in each one?) Bicuspid-2 Left / Tricuspid 3 flaps right h. Semilunar Valves- pulmonary leads to lungs/ aortic leads to aorta (main artery of the body). 5. Cardiac Circulation- blood flows from the atria to the ventricles. Valves do not allow backflow. B. Physiology of the Heart (pp. 368–374) 1. Intrinsic Conduction System of the Heart: Setting the Basic Rhythm a. Intrinsic Conduction SystemElectrical impulses through nerve signals control heart rate. SA Node & AV node signal contraction in a healthy heart. ii. iii. impulses). Ischemia-Dead heart tissue usually resulting from a heart attack Fibrillation Heart rhythms become out of sync (Defibrillators are used to restart the heart 2. Cardiac Cycle and Heart Sounds- Lub Dub Noises are generated when blood exits the atria (Lub) and then passes through the ventricles through the semilunar valves (Dub). Murmurs-Additional sounds from the lub dub rhythm may indicate backflow from one of the AV valves that close improperly. Calculating Cardiac Output (CO) CO= HR (Heartrate)X SV (Amount of blood pumped through the heart in one time). a. Regulation of Stroke Volume (SV) AV and Semilunar Valves typically control stroke volume. b. Factors Modifying Basic Heart Rate (HR)-Stressful situations can lead to an increase in angiotension, vasoconstrictors, and other hormones that would speed up or slow down the heart rate to accommodate to one’s environment. II. BLOOD VESSELS (pp. 374–395) A. Microscopic Anatomy of Blood Vessels (pp. 374–377) 1. Tunics- Tunica Interna- Inner lining of vessel-very slick to reduce friction in bloodflow Tunica Media (composed of involuntary smooth muscle) Tunica Externa-Strong outer layer of vessels 2. Structural Differences between Arteries, Veins, and Capillaries More muscular in arteries for blood pumping Vessels are folded inward in veins preventing backflow B. Gross Anatomy of Blood Vessels (pp. 378– 386) (Key attached separately on webpage as an Adobe document) 1. Major Arteries of the Systemic Circulation (Figure 11.12) a. i. Intercostal Arteries ii. Bronchial Arteries iii. Esophageal Arteries iv. Phrenic Arteries d. Arterial Branches of the Abdominal i. Celiac Trunk ii. Superior Mesenteric Artery Aorta Arterial Branches of the Ascending Aorta i. Right and Left Coronary Arteries iii. Renal Arteries b. Arterial Branches of the Aortic Arch iv. Gonadal Arteries i. Brachiocephalic Trunk v. Lumbar Arteries ii. Left Common Carotid Artery vi. Inferior Mesenteric Artery iii. Left Subclavian Artery vii. Common Iliac Arteries c. Arterial Branches of the Thoracic Aorta 2. Major Veins of the Systemic Circulation (Figure 11.13) a. Veins Draining into the Superior Vena Cava iv. Subclavian Vein v. Vertebral Vein Internal Jugular Brachiocephalic x. Great Saphenous Veins xi. Gonadal Veins xii. Renal Veins i. Radial and Ulnar vi. vii. ii. Cephalic Vein viii. Azygos Vein xiii. Hepatic Portal iii. Common Iliac ix. Tibial & Fibular Veins xiv. Hepatic veins 3. Special Circulations (Figures 11.14–11.17) a. Arterial Supply of the Brain and the Circle of Willis (Pictured to the right; is responsible for circulating blood through the brain from the central nervous system to the peripheral nervous system). Fetal Circulation This process shuttles blood from the mother to the developing fetus with several important steps. The placenta (site of nourishment-similar to a yolk sac) will transfer blood flow to the baby’s developing liver. All oxygen poor blood will then travel to the baby’s heart through the DUCTUS VENOSUS and then pass through the heart. DUCTUS ARTERIOSUS delivers blood back to the fetus after maternal circulation. One important step in this process is that blood flow does not enter pulmonary circulation but rather bypasses it through the FORAMEN OVALE ( a hole between the two atria). This important step happens because the baby’s lungs are NOT fully functional and therefore they do not require pulmonary circulation. c. Hepatic Portal Circulation This process is important for digestion. It delivers necessary nutrients from digestive tract to the blood for circulation throughout the body. Hepatic refers to the liver (Hepatitis-Inflammation of the Liver)