Resurgence of HPAI in Birds and Mechanisms of Transmission
advertisement

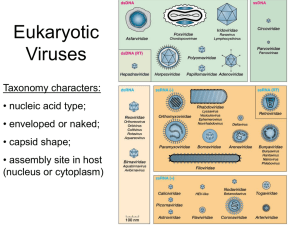
Resurgence of HPAI in Birds and Mechanisms of Transmission David E. Swayne, MSc, DVM, PhD, dACVP, dACPV Southeast Poultry Research Laboratory, Agricultural Research Service, U.S. Department of Agriculture, Athens, Georgia 30605 USA David.Swayne@ars.usda.gov 1. Summary High pathogenicity avian influenza (HPAI) viruses typically produce a severe, systemic disease with high mortality in chickens and other gallinaceous birds, but either no disease or only mild disease in domestic ducks and wild birds. However with emergency of H5N1 HPAI viruses and their maintenance in domestic poultry for past 17 years, there has been a shift in virulence within chickens evident as shorter means death times (MDT) and widespread virus replication in vascular endothelial cells. In domestic ducks, H5N1 HPAI viruses have changed from producing inconsistent respiratory infections in 2 week-old domestic ducks to some strains being highly lethal in adult ducks with virus in multiple internal organs and the brain. The H5N1 HPAI virus has crossed multiple species barriers to infect domestic poultry, captive and wild birds, carnivorous mammals and humans. Human infections have been associated with direct or indirect contact with live or dead poultry while in carnivores, consumption of infected birds or their products have been associated with infections. Experimental studies in the ferrets and pigs demonstrated transmission of H5N1 HPAI virus by oral or direct digestive tract exposure, but required a much higher dose of virus than exposure via the upper respiratory tract. With respiratory trophic H5N1 virus, consumption of infected meat by ferrets initiated infection through the tonsil followed by nasal cavity, but with systemic H5N1 HPAI viruses simultaneous infection also occurred via the upper digestive tract with spread to liver and pancreas. Slaughter of H5N1 HPAI virus infected asymptomatic chickens, produced airborne virus in large droplets and aerosols, and transmitted the virus to infect and kill chickens and ferrets exposed within the same air-space. 2. Introduction Avian influenza (AI) viruses are a diverse group of type A orthomyxoviruses divided into 144 different subtypes based on different combinations of the 16 hemagglutinin and 9 neuraminidase subtypes, and two different pathotypes (low [LP] and high pathogenicity [HP]). LPAI can be any of the 16 H subtypes, but only H5 and H7 subtypes have been HPAI viruses. 3. Pathology In gallinaceous poultry, infection by LPAI viruses produces lesions of inflammation principally in then respiratory tract, especially the upper respiratory tract. However, LPAI viruses can replicate in the intestinal tract but typically without lesions. By contrast, HPAI viruses produce systemic infection in gallinaceous poultry with associated lesions of necrosis and inflammation in most organ systems. However, the HPAI viruses usually produce no clinical signs of infection or only mild disease in domestic ducks and wild birds. Over the past decade, the emergent HPAI viruses have shifted to 1 increased virulence for chickens as evident by shorter mean death times (MDT) and a greater propensity for massive disseminated replication in vascular endothelial cells. Especially important, the Asian H5N1 HPAI viruses have changed from producing inconsistent respiratory infections in 2 week-old domestic ducks to some strains being highly lethal in ducks with virus in multiple internal organs and brain. However, the high lethality for ducks is inversely related to age, unlike these viruses in gallinaceous poultry which are highly lethal irrespective of the host age. The most recent Asian H5N1 HPAI viruses have infected some wild birds producing systemic infections and death. Across all bird species, the ability to produce severe disease and death is associated with high virus replication titers in the host, especially in specific tissues such as brain and heart 4. Field Situation There have been 35 epizootics of high pathogenicity avian influenza (HPAI) in birds since 1959. The H5N1 (HPAI) virus emerged in China during 1996 and has spread to infect poultry and/or wild birds in 63 countries during the past 18 years. In the past 2 years, the majority of the outbreaks of H5N1 HPAI have occurred in Indonesia, Egypt, Vietnam, and Bangladesh, in decreasing order, but also limited cases have been reported in Bhutan, Cambodia, Hong Kong, India, Laos, Libya, North Korea, Myanmar, and Nepal. The majority of the HPAI cases have been H5N1, but outbreaks of H5N2 have occurred in Chinese Taipei (chickens) and South Africa (ostriches), an outbreak of H7N3 HPAI in Mexico (egg-type chickens), an outbreak of H7N7 HPAI in Australia (free range layers), an outbreak of H7N2 HPAI in Australia (free range chickens and layers), and an outbreak of H7N7 in Italy (layers). Reassortment of the hemagglutinin gene of the H5N1 HPAI within China has resulted in emergence of viruses with changes in internals gene segments and different neuraminidases; i.e. H5N2, H5N5, H5N6 and H5N8. The latter has caused outbreaks in South Korea (breeder and meat ducks) and Japan. 5. Transmission Several of the AI viruses have crossed multiple species barriers to infect various poultry species, captive and wild birds, carnivorous mammals and humans. 4.1 Transmission between poultry. In a series of studies,1 an H5N1 HPAI virus (A/Whooper Swan/224/05) was used to determine the susceptibility and pathogenesis of chickens and domestic ducks when administered through respiratory or alimentary routes of exposure. The chickens and ducks were more susceptible to the H5N1 HPAI virus, as evidenced by low infectious and lethal viral doses, when exposed by intranasal as compared to alimentary routes of inoculation (intragastric or oral fed). In the alimentary exposure pathogenesis study, pathological changes included hemorrhage, necrosis and inflammation in association with virus detection were generally observed in most visceral organs of chickens between 2 and 4 DPI, which is similar to lesions and virus localization in birds exposed by natural or experimental intranasal routes. Similarly, the virus caused systemic infection in the ducks characterized by moderate lymphocytic encephalitis, necrotized hepatitis and pancreatitis with corresponded demonstration of virus. However, with alimentary exposure, lesions and/or virus was first demonstrated in upper alimentary tract on 1 DPI suggesting alimentary tract was initial site affected upon consumption of infected meat or gavage of virus in liquid medium. Alimentary infection does require higher exposure doses to produce infection when compared to intranasal exposure in chickens. These data suggest that respiratory exposure 2 to H5N1 HPAI virus in birds is more likely to result in virus transmission than consumption of infected meat unless the latter contain high doses of virus such as in cannibalized infected carcasses. Transmission Birds to Mammals, including Humans. With carnivores, consumption of infected birds or their products have been associated with infections. Consumption of infected meat by ferrets resulted in respiratory system infection with A/Muscovy duck/Vietnam/209/05 and A/Whooper swan/Mongolia/244/05 viruses, or in both severe respiratory and systemic infection with predominant involvement of the liver, pancreas, and large and small intestine with A/Vietnam/1203/04 virus.2 Direct intragastric exposure to infected meat (A/Vietnam/1203/04 virus) resulted in lethal systemic disease mainly affecting the intestine, liver, and pancreas but not involving the lungs. These results demonstrated that exposure of the digestive system to H5N1 influenza viruses could initiate infection either through the tonsil, with spread to respiratory tissues, or through intestinal infection, with spread to the liver and pancreas. Additional work looking at non-Asia HPAI viruses, the dose of virus needed to infect ferrets through consumption was much higher than via respiratory exposure and varied with the virus strain.3 In addition, H5N1 HPAI viruses produced higher titers in the meat of infected chickens and more easily infected ferrets than the H7N3 or H7N7 HPAI viruses. The majority of human infections with H5N1 high pathogenicity avian influenza (HPAI) virus have occurred in the village setting of developing countries with the primary exposure risk being direct contact with live or dead poultry in the household or neighborhood. In Egypt, the majority of the human H5N1 HPAI virus infections with clinical disease have been in women and children and they are the high risk group who tend, play with, slaughter and prepare the household poultry for consumption. Halal slaughter of poultry requires free movement of the bird during the death struggle, which tends to create a viral plume thereby enhancing human exposure by inhalation. In experimental studies in BSL-3Ag, simulated home slaughter of asymptomatic H5N1 HPAI virus infected chickens in generated airborne virus, and chickens and ferrets housed in same airspace as the slaughter process became infected and died.4 Conducting the slaughter step of H5N1 HPAI virus-infected non-vaccinated chickens in a plastic bag greatly reduced the virus transmission through the air to ferrets. Experimental ferret models have shown airborne transmission of the virus from simulated slaughter of subclinically infected chickens or through feeding infected meat. However, the infectious dose required in much lower with aerosol exposure. 6. References 1. Kwon YK, Swayne DE: Different routes of inoculation impact infectivity and pathogenesis of H5N1 high pathogenicity avian influenza virus infection in chickens and domestic ducks. Avian Dis 54(4):1260-1269, 2010 2. Lipatov AS, Kwon YK, Jackwood MJP, Swayne DE: Pathogenesis of H5N1 influenza virus infections in mice and ferret models differ between respiratory and digestive system exposure . J Infect Dis 199:717–25, 2009. 3 3. Bertran K, Swayne DE: High doses of highly pathogenic avian influenza virus in chicken meat are required to infect ferrets. Vet Res 45:60, 2014 4. Swayne DE. Mechanisms of transmission and spread of H5N1 high pathogenicity avian influenza virus in birds and mammals. Abstracts of the Seventh International Symposium on Avian Influenza, pp 50-51. 2009. 4