improving the thrombolysis regime for central venous catheters
advertisement

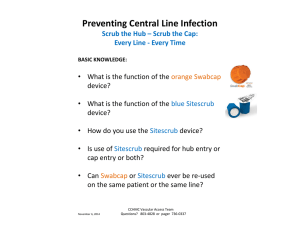
P51 IMPROVING THE THROMBOLYSIS REGIME FOR CENTRAL VENOUS CATHETERS Saunders E1, Davies L1, Thomas H2, Donovan K3, Benzimra R4 and Bradley R2 1 Specialist Dialysis Access Nurse, 2Renal Pharmacist 3Consultant Nephrologist, 4Associate Specialist. University Hospital of Wales, Cardiff and Vale University Health Board Background Central Venous Catheter (CVC) dysfunction prevents adequate haemodialysis (HD) by reducing or ceasing blood flow. This occurs primarily as a result of occlusion of the CVC with fibrin deposition or thrombus formation. The National Kidney Foundation Dialysis Outcomes Quality Initiative (KDOQI) and Renal Association guidance recommend anti-thrombotic therapy as the primary medical intervention to prevent and treat CVC dysfunction. We use citrate line locks in the majority of our HD patients to prevent CVC occlusion. The optimal anti-thrombotic agent for treating CVC occlusion is not clear, therefore on the basis of cost, urokinase is used within our Trust. In 2011, we reviewed our practice regarding the administration of urokinase. Prior to this we had used an overnight infusion, which meant that patients were admitted to the ward. Anecdotally we found that this was often ineffective, so using experience from other centres we adopted a new approach to administering the drug. A “push lock” of Urokinase is used for partial occlusion and a 90minute IV infusion is used where the CVC is completely blocked. To support this change in practice, guidelines were written to provide advice on how to use urokinase, but this change was not fully implemented. Method After the establishment of the dialysis access service, the specialist nurses, along with a specialist pharmacist, revisited the 2011 urokinase guidance in order to develop an information package for the administration of urokinase to unblock HD CVCs. This pack incorporated all the relevant information, including clear nurse administration protocols for the “push lock” and infusion, as well as an algorithm to follow when faced with a poor functioning CVC. Results The new information pack was piloted at one of the satellite HD units for 2 months. This was supported by the specialist nurses and the pharmacist attending the unit to provide teaching to ensure that the nursing staff were fully aware of the changes. One of the main concerns about how the units were previously giving urokinase was that there had been an over-simplification in the “push lock” protocol. This meant that all patients were given the same volume, regardless of the lumen size of their CVC. This could have resulted in the “push lock” being ineffective and the patient being transferred to the hospital for administration of the infusion. The outcomes of the pilot were positive; staff stated that the regime was easy to follow and much better for the patient. The clear guidance about when to use urokinase and a “push lock” protocol which incorporated a nomogram detailing the correct volumes for each CVC size, meant that the nursing staff where confident about how and when to correctly use urokinase. This prevented the patients from having to travel to the hospital for an infusion because, if push locks were unsuccessful, the infusion could be administered at the satellite unit. This has now been adopted on the other HD units, and both the outcomes of the use of urokinase and the frequency of referral to the hospital for further management of the line are being audited. Conclusion The multidisciplinary approach to the development of the new guidance has meant that they are clear and user-friendly. The information pack is readily available in all clinical areas, as are posters of the administration protocols for quick reference. As well as the onsite training sessions for the nursing staff, this has meant that the new guidance has been successfully implemented across the directorate. Cost-savings have been realised by more cost-effective use P51 of the drug, as well as by minimising the distance that the patient has to travel to receive this treatment.