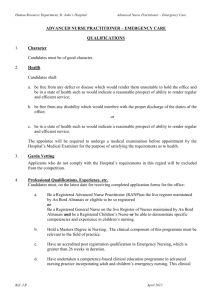
File
advertisement

Hill APN Interview 1 D.A. is 35 years old, married and a mother of three children. She grew up in the Kansas City area. Her educational background includes a Bachelor of Science in Biology, 1995; Bachelor of Science in Nursing (BSN), 2000, and Master of Science in Nursing (MSN) - Family Nurse Practitioner (FNP), 2007. Her work history includes being a Med tech at a lab from 1996-1999; Clinical Associate at a large (375+ bed) hospital from 1999-2000; Registered Nurse in a progressive care unit at the same 375+ bed hospital from 2000-2007; Nurse Practitioner (NP) in internal medicine office, PRN (“as needed”), 2007-2008; “Rounding” Cardiology Nurse Practitioner, PRN, at a large (375+ bed) area hospital from 2007-2008, and a rounding FNP with a large cardiology group at a 525+ bed teaching hospital, 2008-present. Currently, D.A. works as a rounding family nurse practitioner with 37 physicians in a cardiology group at a large (525+ bed) not-for-profit hospital. She see inpatients and outpatients, writes daily progress notes, orders/interprets any tests, and dictates history and physical (H&P) information and discharge summaries, as well as performs all of the computer/background work that needs to be done to take care of hospitalized patients. The challenges of D.A.’s position as a rounding family nurse practitioner are several. First, D.A. works with one of 37 different physicians every week and they all have different styles and preferences. Another challenge D.A. faces is that she works in a teaching institution and therefore, in a lot of ways the system is not very efficient. Also, D.A. feels the role of a nurse practitioner is not well defined. She cites spending a lot of time trying to define her role to her colleagues, the physicians that she works with as well as herself. Finally, D.A discusses that she works in two roles – seeing patients as a mid-level provider, but she is also expected to do all the background work that maybe a nurse or tech might be expected to do in the office setting. One example D.A. gives to support this challenge in her position is setting up patients for follow-up or outpatient testing, obtaining records from other facilities and triaging patients. In general, D.A. makes sure that nothing gets missed – she might spend an hour on a patient but only fifteen minutes at the bedside and the physician might only spend five minutes on that patient and then move on. Hill APN Interview 2 Several benefits to being a FNP with a cardiology group are mentioned by D.A. First, by working in a teaching institution D.A. believes she has learned a lot. She works “in a specialty that I love”, says that the benefits and salary are pretty good, and that she doesn’t have to work weekends, holidays or take call. When asked “What do you wish you had learned while in school, but didn’t?” D.A. points out several items. First, D.A. believes that a nurse practitioner program should prepare an advanced practice nurse to work in a clinical setting as the majority of graduates do. She believes that too much emphasis is placed on theory and not enough on the practical information that advanced degree nurses can use in a clinical setting. Personally, D.A. suspects that she probably would have been better served in an acute care nurse practitioner program. She also believes that even if she did not practice in a hospital setting more time should have been spent on learning test interpretation (chest x-rays, lab, etc). Also, D.A. believes more advanced physiology, pathophysiology and pharmacology would have been helpful. D.A. states that most of her knowledge in her current setting was obtained from previous experience in cardiology and on the job training. D.A. still feels very insecure about her knowledge beyond that and also believes that it would be advantageous to have some sort of system for specialty certification. When asked how she first became interested in advanced nursing practice, D.A. stated that after she graduated with her first degree (BS in Biology, 1995), she didn’t really know what she wanted to do. She discusses working at a lab for awhile as a med tech but felt that wasn’t going to lead to anything. She had always liked the medical field and so she explored her options. Like many nurses, D.A. feels that nursing has the most opportunity and flexibility, “You can choose many different types of specialties and settings and move around within the field if you don’t like where you end up”. She also says that she had planned from the start on getting a master’s degree. One area of nursing that D.A. discussed pursuing was as a nurse anesthetist, but she felt the hours and schooling wouldn’t work as well with having a family. A typical day at work for D.A. includes arriving between 0730 and 0800. First, she gets updated patient lists from the admitting department and updates the list in the computer. Then, Hill APN Interview 3 she “rounds” on their groups primary patients – checks labs, tests, vitals, telemetry, sees and examine the patient, write a note, and orders anything that needs to be done or starts working on discharging the patient. Next, she “rounds” on any consults they may have received with the same routine as above. Then she meets up with the rounding physician at some point early in this process, and they talk about who needs what, see some patients together and see some separately. All day long D.A. sees new consults, admit patients from either the office, emergency department (ED), or as transfers from other facilities. Next, she dictates admission H&Ps, discharge summaries, and signs off on notes. Then she enters all the information in the computer that needs to be entered. She mentions that her facility currently uses two computer systems – one for the hospital and one for the clinic and that most of the information needs to go in both systems. D.A. mentions this as very time consuming, however, she also knows that soon her office will be switching to the same system that the hospital uses. D.A.’s “typical day” is not “typical” at all. Each day varies depending on the number, timing, and complexity of the new patients coming in. It also varies from week to week depending on the physician that she is working with, as “they all have different expectations of the mid-level provider and they all approach each diagnosis differently”. In D.A.’s opinion, there really hasn’t been much talk about the doctorate nurse practitioner (DNP) program outside of academia. She believes that nurses in general need to further their education and the logical route is to have an advanced practice nurse get a doctorate to practice. She also discussed that the DNP program should be much more clinical in nature or there should be an RN to DNP bridge program that puts much more emphasis on clinical education. She believes that there is concern from physicians about the title associated with this program – that boundaries could be blurred; patients could be confused, etc. However, D.A. states “We will not be medical doctors”. She believes that there are people out there that might misrepresent themselves, but thinks for the majority of people it won’t be a problem. In a related issue, D.A. feels strongly that the level of education should change for registered nurses (RNs) as well. She believes an RN should have a BSN at the minimum, and says we need to Hill APN Interview 4 have separate roles for an associate’s prepared nurse and a bachelor’s prepared nurse. In her opinion, this issue is much more important than having the advance practice nurse (APN) receive a DNP. In closing, her advice to the “new” advanced practice nurse was simple: “Don’t rush to find a job. It’s more important to find a good fit.”