Common viral infections - Ipswich-Year2-Med-PBL-Gp-2
advertisement

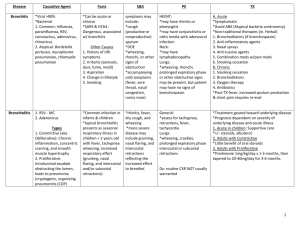
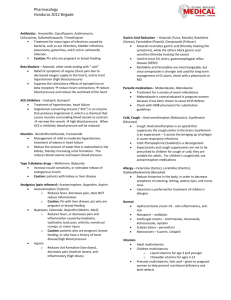
PBL 14 A Persistent Cough Rick Allen Common viral infections. Cold and flu, croup, bronchiolitis. Managing Pt treatment expectations in cold & flu presentations Croup laryngotracheobronchitits – inflammatory narrowing of the airway inspiratory stridor. Parainfluenza virus. Fever, coryza (head cold symptoms), sore throat, hoarseness, cough. Laryngoepiglottis Caused by RSV (respiratory syncitial virus), haemophilus influenzae or β-haemolytic streptococci sudden swelling of epiglottis and vocal cords are potentially leathal in young kids…not in adults due to larger airways. Bronchiolitis (laryngotracheobronchitis) – vocal cord swelling and abundant mucus exudate. Impaired bronchociliary function secondary bacterial infection increase of symptoms. Can block smaller airways and lead to atelectasis (incomplete expansion or collapse of a portion of a lung) Pertussis Bordetella pertussis, pertussis = “violent cough”. Gram neg aerobic bacilli. Spread = unimmunized house – 80-100%. Immunized = 20% Pathogenesis = attaches to nasopharynx epithelium (adhesins), replicates, releases toxin, which causes local mucosal damage along with other stuff. Incubation 7-10 days. Symptoms – Whooping cough, prolonged/paroxysmal/sleep-disturbing cough, Can cause vomiting. Fatigue evident. Cough can become less frequent and severe after 2-4 weeks, lasting 1-3 months. Complications = ↑ intrathoracic pressure petechiae haemorrhages on face and trunk, Hernias, wt. loss (↓ intake), pneumothorax. Dx. nasopharyngeal swab/aspirate then culture. Tx. macrolide Ab. Azithromycin/clarithromycin/erythromycin Prevention: chemoprophylaxis (wow!) and immunisation. Common Cold Generally speaking are inflammatory diseases of the upper airways. Origin = viral bacterial (greater symptoms) -Infectious rhinitis –aetiology: adenovirus, echovirus, rhinovirus pathogenesis: evoke profuse catarrhal discharge. Initial acute stage, nasal mucosa is thickened, red and oedematous, nasal cavaties narrowed, turbinates enlarged. Can extend pharyngotonsilitis. Secondary bacterial infection enhances the inflam. reactionmucopurulent/suppuratives exudate. Symptoms approx. 10 days, + 3 in smokers, resolve without sequlae. Incubation 1-2 days. PBL 14 A Persistent Cough Rick Allen Symptoms: rhinorrhoea, sneezing, nasal congestion, sore throat, systemic – malaise, headache. Can exacerbate asthma and chronic pulmonary issues, blockage of pharyngotympanic tube/sinus drainage otitis media/acute sinusitis. Immunosuppressed pneumonia Tx. – Symptomatic. Sinusitis Acute is generally preceded by acute/chronic rhinitis. Maxillary sinusitis can arise from a periapical infection through the bony floor of the sinus. Aetiology: many common nasal flora. Inflam. is nonspecific (oedema) blockage of sinus drainage suppuratives exudates (sinus empyema) Tonsilitis Enlargement of lymphoid tissue (hyperplasia) within Waldeyers ring. Influenza Aetiology: A, B or C based on nucleoprotein surrounding single-strand RNA. Lipid bilayer round the outside with viral hemagglutinin and neuraminidase (H1N1). This is what Ab’s are created against. Type A – infects humans, pigs, birds, horses. Major pandemic and epidemic cause. Antigenic drift = Mutations of H and N causes repeated infections by avoiding host Ab’s. Antigenic shift = H and N are replaced with those of animal varients, leading to all people being susceptible. Type B and C do not undergo shift or drift and therefore only affect kids. Symptoms: abrupt onset, fever, cough, myalgia (muscle pain), malaiseUsually self resolves in 2-5 days, with a cough lasting for approx. 1-2 weeks after. Complications: . Complications are usually due to exacerbation of pulmonary complications. >64, <2, pregnant in 2nd/3rd trimester. Pneumonia Clearance: cytotoxic T cells kill infected cells, and intracellular anti-influenza protein (Mx1) is induced in macrophages by cytokines (IFN-α and β) Pathogenesis – spread most efficiently via airborne droplets, though contact and fomite transfer may also be to blame. Virus invades URT epithelium, replicates within cells and then spreads rapidly. Causes necrosis, can cause metaplasia. Unlikely to be found outside pulmonary system despite systemic symptoms. Morphology: mucosal hyperaemia, and swelling, with primarily lymphomonocytic and plasmacytic infiltration of submucosa plus mucous oversecretion can plug sinuses, pharyngotympanic tube or nasal channels secondary bacterial infection. PBL 14 A Persistent Cough Rick Allen 2008 NICE (National Institute for Health and Clinical Excellence) guidelines from the UK recommend that patients seeking medical evaluation for cold symptoms should [5,6]: Be advised that the usual course and duration of illness is up to one and a half weeks for patients with a cold; symptoms persist an additional three days on average in smokers [7] Be informed regarding the risks and benefits of symptomatic management, including analgesics and antipyretics Be informed and reassured that antibiotics are not needed and may have side effects Have their concerns and expectations discussed Be advised to return for review if their condition worsens or exceeds the expected time for recovery. We suggest prophylaxis with vitamin C (200 to 500 mg daily) for prevention of upper respiratory infection for people exposed to vigorous activity in extreme cold conditions (Grade 2B) (does not change severity). We suggest not using echinacea or vitamin E for prophylaxis of colds (Grade 2B). (See 'Prevention' above.)