Hemoglobin__O2
advertisement

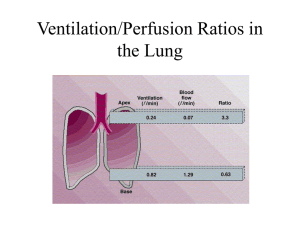
Hemoglobin – O2 & CO2 Transport. Respiratory Physiology. Wittmers. Katelyn Rogers. 10.26.09. Learning Objectives: 1. Define oxygen partial pressure (tension), oxygen content, & percentage hemoglobin saturation as they pertain to blood. O2 will dissolve in blood to an extent that is determined by the equilibrium between the undissolved O2 & the O2 that has dissolved in the blood. *Oxygen Partial Pressure (tension) – the individual P exerted independently by O2 within a mixture of gases w/in the blood. Also basically the amt of O2 dissolved in the plasma. Because this obeys Henry’s Law amt dissolved (xPx) is proportional to the partial pressure (Px) (100 mm Hg of PO2 there is 0.3 ml O2/100ml in arterial blood). *Oxygen Content – dissolved + bound to Hb. [1.39 x Hb x (SaO2/100)] + 0.003 x PO2= 20.3ml] Each gram of Hb can carry 1.39 ml of O2. Usually in arterial blood 97.5% of Hb is satd & blood contains 15 g Hb/100ml. In mixed venous blood, PO2=40 mm Hg & SaO2=75%. *Percent Hemoglobin Saturation – Percentage of the available binding sites that have O2 attached. SaO2 = (HbO2/O2 capacity) x 100 2. Draw an oxyhemoglobin dissociation curve (Hb ox equil curve) showing the relationships between ox partial P, hb saturation, & blood ox content. On the same axes, draw the relationship between PO2 & dissolved plasma O2 content (Henry’s Law). Compare the relative amounts of O2 carried bound to Hb with the carried in the dissolved form. Bound = 20.3 ml O2 Dissolved = 0.3 ml O2 Arterial bld O2 conc=21ml/100ml, while venous bld O2 conc=16ml/199ml 3. Describe how the shape of the oxyhemoglobin dissociation curve influences the uptake & delivery of ox. Sigmoidal in shape because as each consecutive O2 binds to Hb there is an inc in Hb affinity for O2 helping upload. Flat portion of curve in resting tissue: Large change PO2 small change SaO2, meaning even if the PO2 in alveolar gas falls somewhat, loading of O2 will be little affected. Additionally, as the RBC takes up O2 along the pulm cap, a large partial P diffc btwn alveolar gas & blood cons to exist when most of the O2 has been transferred. As a result the diffusion process is hastened. In highly metabolizing tissues, steep portion: helps unload O2. Large amts can be withdrawn for only a small drop in cap PO2. 4. Define P50 The PO2 in the blood at which the Hb is 50% saturated, typically about 27 mmHg for a healthy person. A conventional measure of Hb affinity for oxygen. A R shift incs P50, meaning a larger partial pressure is needed to maintain SaO2= 50%. This indicates decreased affinity. 5. Show how the oxyhemoglobin dissociation cure is affected by changes in blood T, pH, PCO2, & 2,3-DPG, & describe a situation where such changes have important physiological consequences. Exercising muscle shifts R: Acid (incd H+) Hypercarbic (Incd PCO2) Hot (incd T) And benefits from increasing its unloading of O2 from its capillaries. 2,3-DPG – incs during chronic hypoxia (high altitude or chronic lung disease). Shifts R. Unloading of O2 is assisted. Use P50 to determine placement of curve. (Norm 27 mm Hg) Note: As blood passes from the arterial system L shift holds onto O2. to the veinslets the following R shift go of O2. occurs: T rises a FEW degrees, CO rises a FEW mm Hg, & pH falls a FEW tenths of a unit. 6. Describe how anemia & carbon monoxide poisoning affect the shape of the oxyhemoglobin dissociation curve. In anemia there is no L shift, but there is a decrease in Hb conc resulting in decreased O2 conc. A small addition of CO to blood causes a L shift bc it has a 240 times greater affinity for Hb then O2. The PCO axis is greatly compressed for this reason small amts can tie up a large proportion of Hb. Hb conc & PO2 may be normal, but the O2 conc is grossly decreased. The L shift interferes with the unloading of O2. 7. List the forms in which carbon dioxide is carried in the blood. Identify the percentage of total CO2 transported as each form in both arterial & venous blood. couldn’t find just Venous blood!) Dissolved CO2 % Bicarbonate% Carbamino Compounds% Arterial Blood 5 Venous-Arterial Diffc 30 90 5 60 10 (I 8. Describe the importance of the importance of the chloride shift in the transport of CO2 by the blood. Bicarbonate is formed in the blood by the following sequence: The first rxn is slow in plasma, but fast in RBCs bc of CA presence. The second rxn is fast even w/o an enzyme. HCO30- diffuses out, but H+ can’t be displaced as easiliy bc the membrane is impermeable to cations, so to maintain electrical neutrality, Cl- ions move into the cell from the plasma. Th isis called the Chloride Shift. 9. Identify the enzyme that is essential to normal carbon dioxide transport by the blood & its location. Carbonic Anyhdrase (CA) located mostly in the RBCs. 10. Draw the carbon dioxide dissociation curves for oxy- & deoxyhemoglobin. Describe the interplay between CO2 & O2 binding on hemoglobin that causes the Haldane effect. The H+ that is liberated from the chloride shift binds reduced hemoblogin (Hb w/ no O2 – which is better able to mop up the H+ ions since less acidic), thus allowing loading of CO2 (bc of release of O2) in peripheral tissues. The fact that deoxygenation of the blood incs its ability to carry CO2 is known as the Haldane effect. Much more linear than O2 diss curve. The lower the saturation of Hb with O2, the larger the CO2 concentration for a given PCO2. Note also that formation of carbamino-Hb, (HbNH2 + CO2 HbNHCOOH) occurs better with reduced Hb than with HbO2. Key Concepts: Most of O2 transported in blood is bound to Hb. The max amt that can be bound is called the O2 capacity. The O2 saturation is the amount combined with the hemoglobin divided by the capacity & is equal to the proportion of the binding sites that are occupied by O2. The O2 dissociation curve is shifted to the R (that is, the O2 affinity of the Hb is reduced) by incs in PCO2, H+, T, & 2,3-DPG. Most of the CO2 in blood is in the form of bicarbonate, with smaller amts in dissolved and carbamino cpmds. The CO2 dissociation curve is steep and more linear than that for O2. Questions: 1. What is the term for oxygen bound summed with dissolved oxygen? a. O2 capacity b. O2 content c. O2 saturation d. Partial Pressure of O2 2. Define P50. True/False: it is a conventional measure for partial pressure of oxygen. 3. Which of the following result in a L shift of the oxyhemoglobin curve? a. Incd T b. Dec pH c. Inc CO2 d. Dec 2,3-DPG 4. What is the main difference between anemia and carbon monoxide poisoning on oxyhemoglobin curves? 5. What is the major form that CO2 is carried in the arterial blood? 6. Which of the following is false about the CO2 dissociation? a. Curve is more linear in shape. b. Lower saturation of Hb w/ O2, the smaller the CO2 conc for a given PCO2. (Haldane effect) c. The chloride shift allows for loading of CO2 in peripheral tissues. d. Carbamino-Hb forms easier with reduced Hb than HbO2. Answers: 1. b 2. The PO2 in the blood at which the Hb is 50% saturated. F, for Hb affinity for oxygen. 3. d 4. Anemia only lowers the curve, while CO poisoning also shifts the curve to L. 5. Bicarbonate. 6. b, It should be say, “that larger the CO2 conc for a given PCO2. (Haldane effect)