proteinurea
advertisement
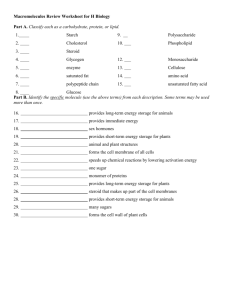
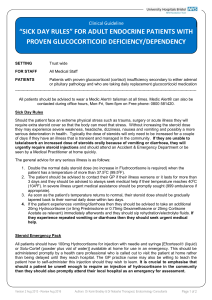
proteinurea 10% of children aged 8-12 years have +ve test for Protienurea. Ways of detection of Protienurea. 1-Dipstick, qualitative assessment of protein excretion, primarily for albumin and less sensitive for others types of protein(LMW, Bense Jones , gamma globulin),trase(10-20mg/dl), +=30, ++(100), +++=(300) , ++++=1000-2000mg/dl. False +ve 1-grosse haemeturia 2-contamination with antiseptic 3- urine PH greater than 7 4- phenozopyridne medication 5- high concentrated urine(sp.gravity more than 1.015) False –ve 1- diluted urine(sp.gravity less than 1.005) 2- other than albumin 2-Timed 12-24H urine collection for protein Normally 150mg/day, or 4mg/m2/day Abnormal=4-40mg/m2/hr Nephrotic range more than 3.5g/day or more than 40mg/m2/hr 3- URINARY PROTIE/ URINARY CREATINNE (upro/ucre) Normally less than 0.5 in child less than 2year and less than 0.2 in child more than 2year More than 3 suggest nephrotic range. Nephrotic syndrome Definition prevalense 2-3/100000 Disease of children (15 fold than adult) 1.proteinuria above 40 mg/m²/hr(or 1g/kg/24hr)or urinary protein (mg/dl)/creatinine(mg/dl)ratio of 2.0 or more ;alternative units-ratio more than 0.2mg/micromole 2. Hypoalbuminamia(serum albumin less than 25g/l 3.Hypercholesterolemia(serum cholesterol over 200mg/dl,5.25mmol/l 4.Oedema The primary abnormality is protein urea .others features are secondary to this, others chara .findings include .Hypocalcaemia(ionized fraction normal),below 9.0mg/dl .Hyponatremia(below 135mmol/l .Hypercoagulabity(decrease partial thromboplastin time(PTT) Etiology 90% Idiopathic,10%secondary(related to glomerular diseases like membranous nephropathy, membranoprolefretive) 85%minimal change disease nephrotic syndrome(MCNS) Most common type ,affect younger children (2-5),and more in boys(until the puberty),it is thought to be due to defective electrostatic glomerular barrier (due to circulating lymphokine). An associated defect is proliferation of a T- cell subclass.MCNS characteristically shows fusion of epithelial foot process on electron microscopy Clinically , hypertension and haemeturia occur in 10% and in about 95%steroid responder 10%Focal segmental G.sclerosis ,histolegically,there is mesangial proliferation, increase in matrices, and segmental sclerosis,20% steroid responder and may lead to end stage renal failure 5%Mesangial proliferative deffuse mesangial l cell proliferation, increase in matrice, 50% steroid responder . Pathpphysiology Increase permeability of glomerular capillary wall lead to massive protein urea and hypoalbuminemia. The cause still unknown,in MGNS , there is possiple T- cell defect, In focal segmental sclerosis, plasma factor, perhaps prodused by lymphokines may responsible for increase in capillary wall permeability protein urea→hypoalbumin→↓oncotic pressure→shifting of fluid from intravascular spase to the interstitial compartment→↓↓intravascular volume →↓renal perfution→activate Renin-Angiotensen-Aldosteron system→stimulate tubuler reabsorption of NA+ alsoADH lead to reabsorption of water →Odem This theory not apply to all patients with nephrotic syndrome, however, because some patients actually have increase intravascular volume with diminished levels of rennin and aldosteron.Therefore, other factors, including primary renal avidity for sodium and water, may be involved in the formation of odema in some patients with nephrotic syndrome. Hyperlipidemia(cholesterol and trigyceride) is due to 1- Hypoalbuminamia may stimulate hepatic synthesis of lipoprotein 2- loss of lipoprotein lipase in urine which is responsible for degradation of lipoptotien. Minimal change disease nephrotic syndrome(MCNS) Clinical feature Most common age (2-6),reported as early as 6months of age The initial episode and subsequent relpse may flow minor infection,occusionaly related to insect bite. Mild edema noted around the eye and then to lower extremity ,may be misdiagnosed as allergic disorders. with time edema become generalized with ascitis,pleural effusion and genital odema Anorexia, irritability,abdominal pain,diarrhea are common Hypertension and grosse hematuria are uncommon D.DX Hepatic failure, congestive heart failure, acute or chronic GN, protein malnutrition , protein loosing enteropathy Diagnosis Any child with NS should probably have the following tests URINE 1-proteinin urine 3+ or 4+(1+=10- 20mg/dl,2+=100mg/dl,3+=300mg/dl,4+=1000-2000mg/dl)or proteinuria above 40 mg/m²/hr(or 1g/kg/24hr)or urinary protein (mg/dl)/creatinine(mg/dl)ratio of 2.0 or more ;alternative units-ratio more than 0.2mg/micromole 2- cellular cast which do not to occur in INS but may well occur in other glomerlonephropathies(note that halyine or waxy casts are common in INS 3- micro .RBC in 10-20%. BLOOD 1- Urea , creatinin and electrolytes(renal function usually normal in INS(10-20%increase in BUN); may be abnormal in other glomerlonephropathies 2- Albumin(less than2.5g/dl) and total serum protien 3- increase Serum cholesterol and triglyceride 4 Serum complement level C3,C4(low with msangial proliferative ,SLE., normal in INS) 5- Hepatitis B and C serology (Hep B is associated with membranous nephritis, Hep C is associated with msangial proliferative. Renal biopsy not required in most patients, and should be reserved for those very atypical feature. There is probably NO indication for biopsy before commencing non-steroid agents if the child completely responsive to predisolone (protein urea absent in the past 3 days).so indicated in the following 1- Age before 1year and above 8years 2- Macroscopically hematuria 3- Persistent hypertension and microscopically hematuria 4-Abnormal levels of complements 5- Elevated serum creatinin level Definitions in NS Remission=urinary protein excretion less than 4mg/ m²/hour or trace of protein in urine dipstick, or urinary protein (mg/dl)/creatinine(mg/dl)ratio of0.2 mg/dl for 3 consecutive days Relapse=recurrence of protein urea defined in INS 3- 4+dipstick +edema. Frequent relapser=2 or more relapse in the first 6months of initial response OR more than 4 relapse in 12months Corticosteroid dependence=2 consecutive relapse while on steroid (every other day) or within 2 weeks of ceasing steroid Corticosteroid resistance =failed response after 8weeks of 2mg/kg/day Treatment (supportive ) mild to moderate edema may be managed as outpatients , lowsodium diet , oral diuretics???? severe symptomatic edema, including large pleural effusions, ascites, or severe genital edema, should be hospitalized. In addition to sodium restriction, fluid restriction may be necessary if the child is hyponatremic . A swollen scrotum may be elevated with pillows to enhance the removal of fluid by gravity. Diuresis may be augmented by administration of furosemide (1–2 mg/kg/dose IV q 12 hr). IV administration of 25% human albumin (0.5 g/kg/dose q 6–12 hr administered over 1–2 hr) followed by furosemide (1–2 mg/kg/dose IV) is often necessary when fluid restriction and parenteral diuretics are not effective. Such therapy mandates close monitoring of volume status, serum electrolyte balance, and renal function. Symptomatic volume overload, with hypertension and heart failure, is a potential complication of parenteral albumin therapy, particularly with rapid infusions. Treatment(specific) In children with presumed MCNS, prednisone should be administered (after confirming a negative PPD test and administering the polyvalent pneumococcal vaccine) at a dose of 60 mg/m2/day (maximum daily dose, 80 mg) in a single daily dose for 4-6 consecutive wk. An initial 6-wk course of daily steroid treatment leads to a significantly lower relapse rate than previously recommended shorter courses of daily therapy. About 80-90% of children respond to steroid therapy (clinical remission, diuresis, and urine trace or negative for protein for 3 consecutive days) within 3 wk. The vast majority of children who respond to prednisone therapy do so within the first 5 wk of treatment. After the initial 6-wk course, the prednisone dose should be tapered to 40 mg/m2/day given every other day as a single daily dose for at least 4 wk. The alternate-day dose is then slowly tapered and discontinued over the next 12 mo. There is evidence that both an increased dose of steroids and a prolonged duration of therapy are important factors in reducing the risk of relapse. While planning the duration of steroid therapy, the side effects of prolonged corticosteroid administration must be kept in mind. Many children with nephrotic syndrome experience at least 1 relapse (3-4+ proteinuria plus edema). Although relapse rates of 60-80% have been noted in the past, the relapse rate in children treated with longer initial steroid courses may be as low as 30-40%. Relapses should be treated with 60 mg/m2/day (80 mg daily max) in a single am dose until the child enters remission (urine trace or negative for protein for 3 consecutive days). The prednisone dose is then changed to alternate-day dosing as noted with initial therapy, and gradually tapered over 4-8 wk. 2-Other agents,cytotoxic drugs(CLAIM C cyclophosphamide(CPA:2-3mg/kg for 8-12weeks),Chlorambucil 0.2mg/kg for 8-12 weeks), Cyclosporine(CSA:2.5mg/kg12hourly for 12months L levamisole(2.5mg/kg daily for 6-12 months) A angiotensin-converting enzyme ACE inhibitors I immunization with pnuemoccocal vaccine M mycopgenolate mofetil 25mg/kg /day for 1year CPA has significant side effect ,short term=bone morrow suppretion.risk of viral infections such as varicella,measles)long term (gonadal toxicity and risk of malignancy) CAS can cause nephrotoxicoty, hypertention,gingival hypertrophy and hirsutism Levemisole cause enhanced celluler immune response in certain conditionswith depressed immune function,and may help to maintain remission in steroid-dependent INS(neutropenia,rarly vasculitis,liver toxicity,convulsion ) ACE inhibitor reduce glomerular hyperfilteration (hypotention and cough) Immunization,heptavalent conjugate(7vPCV) in children less than 5years and polysaccharide pnuemoccocal vaccine (PPV23) 5YEARS AND OLDER mycopgenolate mofetil used in lopus type ALL the above medications are indicated in the following 1- steroid resistant type 2- steroid dependent type(only if side effect are unacceptable) 3- frequent relapse with hypertension or thrombosis 4- unacceptable steroid side effect(weight gain, cushnoid facies 3- Antibiotics Some unite treat all episodes of relaps with prophylactic daily penicillin to ovoid pnuemoccocal infection. Others not, some use hird generation cephalosporin ,however the use of prophylactic antibiotic during relapse remain controversial 4- Immunization Live viral vaccine should be avoided in patient taking steroid or other immune suppressive drug. pnuemoccocal vaccine is recommended and annual influenza vaccine. 5- Hypertension Minority, treated by nifedipine and beta blocker 6- Diet No added salt, no fluid restriction unless in very edematous and diuretics is required ,high biological value protein. 8- In hospital management Fluid balance chart, twice daily weight, 4-horly chart of vital sings. 9- Activity No need for bed rest or restriction of activity. Complications of NS 1- Infection More with encapsulated bacteria(pnuemoccocal, haemphilus ) including spontaneous bacterial peritonitis (SBP) , cellulites, UTI,pneumonia due to many factors •urinary loss of immunoglobulin •loss of B factor of alternate activation path. •loss of transferring •alter T- cell function •steroid and other immune suppressive therapy •mechanical factors such as edema and ascitis •malnutrition The occurrence of (SBP)is 2-6%and this risk is further increased by decrease mesenteric blood flow and increase coagulability causing micro infarction The (SBP) need high index of suspicion because the clinical signs some times are masked by the steroid (blood culture, peritoneal fluid culture then prompt antibiotic) 2- Thromboembolism NS associated with Hypercoagulabity (2-5%) state due to Due to increase prothrombotic activity(fibrinogen, thrombocytosis, haemoconcetration and relative immobilization ) and decrease fibrnolytic factor(loss of antithombin 111, and protie C, S), prophlyctic anticoagulant not recominded unless they have previous thromboemboliv event. Over use of diuretics, and use of indwelling catheter should be restricted. Prognosis Majority of child with steroid responsive NS had repeated relapse with time, decrease relapse specially if not getting relapse in the 1st 6months steroid responsive NS not lead to chronic renal failure, and not hereditary, normal sterility in absence of prolonged use of cyclophosphomide) child during remission no need for testing of Protienurea. Steroid resistant NS poor prognosis end stage renal failure dialysis and renal transplant(30-50% getting the same disease) Secondary NS 10% 1-drugs(pencillamine, gold 2- membranoprolefretive NS 3-PSGN, LOPUS, HSP 4- infection malaria, Hepatitis B,C, HIV 5- Malignancy H. lymphoma. Congenital NS In the 1st 3month most common type Finnish type autosomal recessive ,increase alpha feto protein, large placenta, marked edema, prematurely, RDA, separation of cranial suture Lead to end stage renal disease, no value of steroid or cytotoxic ACE inhibitor, endomethacine, unilateral nephrectomy Other form is due to infection(TORCH).