Crohn`s disease
advertisement

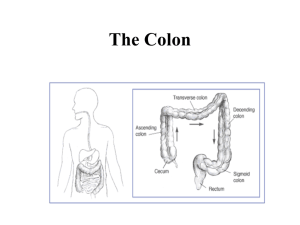
MINISTRY OF HEALTH OF THE REPUBLIC OF UZBEKISTAN Tashkent Medical Academy Department: Surgical Diseases for GP Subject: diarrhea syndrome Methodical recommendation for medical students , postgraduate residents and medical residents Tashkent-2012 Compiled by: Navruzov S.N. - MD Professor of the department of Surgery for GP- TMA. Ahmedov M.A.- MD Professor of the department of Surgery for GP- TMA. Sapaev D.A - PhD, Assistant of the department of surgery for GP- TMA. Mavlyanov A.R. - MD Professor of the department of Surgery for GP- TMA. Sapaeva Sh.A. - PhD, the senior lecturer of chair of anatomy, operative surgery and pathological anatomy of Urgench branch TMA. Reviewers: Nazirov F.N. – MD Professor of the chairs of faculty and hospital surgery of the Tashkent medical Academy. Dautov F.A - MD Professor of the department of Surgery and Pediatric Surgery, Tashkent Institute of Postgraduate Medical improvement . The purpose of these methodological recommendations is a detailed introduction to the students and doctors with one of the most important problems of coloproctology - diarrheal syndrome. This pathology is considered to be one of the common and serious medical and social problem because of the lack of the information about the etiology, pathogenesis, treatment and prevention. Methodical development reviewed and discussed at a meeting of the department of surgical diseases for GP of the medical faculty TMA, protocol №3 from December, 29th, 2011. Reviewed and recommended for publication by Central Methodical Commission. Protocol № Chairman, Professor: Teshaev O.R Considered and approved by the Scientific Council of TMA. The protocol № from _____________________ 2012 Scientific Secretary: Salomova F.I. Translated into English by Ollanazarov H.D – 2 year postgraduate resident of the department of Surgical diseases for GP . Introduction Diarrhea - is a frequent loose or watery stools. The main symptoms of diarrhea: bulky stools, increased defecation, soft and loose stools. Diarrhea is very common in many diseases. The most likely causes of acute diarrhea : acute gastroenteritis, food poisoning, overeating, side effects of antibiotics, chronic infections of gastrointestinal tract. Diarrheal syndrome manifests in such diseases of the large intestine : as ulcerative colitis, amebiasis , Crohn's disease, diffuse polyposis of the colon. In Uzbekistan often diagnosed ulcerative colitis and Crohn's disease.Diffuse polyposis is often is inherited in a family. Amebiasis of the colon can be considered as regional pathology of Uzbekistan. General practitioner will often encounter patients with a syndrome of diarrhea, therefore, should know these diseases, in order to reduce the number of complications of this syndrome ,the number of complicated forms of the syndrome of diarrhea ,to diagnose on time , to determine the timing of planned and emergency hospitalization of patients with these pathologies. Intersubject and Interdisciplinary connection. Anatomy, regional anatomy, pathological anatomy, pathophysiology, clinical pharmacology, gastroenterology, infectious disease, endocrinology, surgery, oncology, anesthesiology and resuscitation. The theoretical part (etiopathogenesis, diagnosis, clinical treatment - the main points). The term "inflammatory bowel disease" is a collective and is usually used to refer to ulcerative colitis and Crohn's disease, as they have much in common in the etiopathogenesis and clinical picture . This term is particularly useful for differentiating between these diseases and other inflammatory bowel diseases with well-known etiology, such as infectious, ischemic, or radiation. One of the most severe inflammatory diseases are: Crohn's disease, ulcerative colitis, amebiasis of the colon. Accurate data on the prevalence of ulcerative colitis is difficult to obtain because it has often unaccounted mild cases, especially in the initial stage of the disease. These patients are usually observed in non-specialized outpatient facilities and that’s why are difficult to calculate. Ulcerative colitis is most common in urbanized countries, particularly in Europe and North America. In these regions, the incidence of ulcerative colitis (primary disease) ranges from 4 to 20 cases per 100 000 population, amounting to around 8-10 per 100 000 population per year. According to modern ideas, NUC (nonspecific ulcerative colitis) occurs with a frequency of 1:10,000. Crohn's disease is less common than the NUC, and corresponds to the latter as 1:5 - 1:10. Amoebiasis - protozoal disease and caused by Entamoeba histolitica which is characterized by the development of chronic relapsing hemorrhagic - ulcerative colitis. The greatest number of cases in the age of 20-40 years. The second peak of incidence observed in the older age group - after 55 years. The highest death rates occurs within 1 year of disease due to the extremely difficult cases of fulminant disease course and 10 years after its start because of the development of colorectal carcer in some patients . The main functions of the colon - is absorption, secretion and evacuation. All of them are closely related, violation of one function leads to the frustration of others. Ulcerative colitis - a chronic disease characterized by hemorrhagic-purulent inflammation primarily mucosal and submucosal layer of the colon with the development of systemic and local complications. Crohn's disease is a nonspecific inflammatory disease of the intestine, which can affect any part of the gastrointestinal tract. Regional enteritis usually causes abdominal pain and diarrhea. The prevalence of ulcerative colitis and especially Crohn's disease, in comparison with other forms of not high, but by the severity, by the needs for hospitalization- surgical treatment of these two diseases occupy an important place, and is actively discussed in the literature. This discussion is almost always parallel to the clinic because both diseases are very similar: constant, intermittent, or dispensed abdominal pain, diarrhea with blood and mucus, sharp, up to cachexia weight loss, anemia, marked dysbiosis .. Most clear differences between the NUC and Crohn's disease seen in pathological forms. The inflammatory process in the NUC always starts in the mucosa and always involved the rectum. In Crohn's disease in 20-25% of patients inflammatory changes in the rectum is not found. In contrast to the NUC in Crohn's disease inflammatory process starts in the submucosal layer of the intestine, so mucosa is less affected. Ulcerative colitis on the base of the inflammation of the mucosal layer stands -ulceration so-called crypt-abscesses, while in Crohn's disease inflammation starts in the submucosal layer and therefore does not drain as ulcers in ulcerative colitis, as well as separated cracks, which penetrate deeply, sometimes to the entire thickness of the bowel wall, and interspersed with healthy-looking areas that creates the characteristic picture of a “cobblestone street”. The etiology and pathogenesis. The exact etiology of ulcerative colitis is unknown to date. We discuss three basic concepts: 1. The disease is caused by the direct influence of some exogenous environmental factors, which have not yet been established. The main reason is considered an infection. 2. Ulcerative colitis is an autoimmune disease. If there is a genetic predisposition of the body ,influence of one or more factors triggers a cascade of launching mechanisms directed against its own antigens. A similar model is characteristic of other autoimmune diseases. 3. This disease is caused by an imbalance of the immune system of the gastrointestinal tract. Against this background, the impact of various adverse factors leads to an excessive inflammatory response, which occurs due to an inherited or acquired disorders of the mechanisms of regulation of the immune system. Repeated attempts to link the development of NUC with infectious factors have been unsuccessful. More encouraging were the results of studies of immunological disorders in this disease. In the patients' blood were found specifically sensitized lymphocytes to intestinal antigens and immune complexes. The opinion of the leading etiologic role of psychogenic factors expressed by Muray, on closer examination also proved inconclusive. More interesting are the views of the importance of genetic factors in the occurrence of NUC. However, due to limited and insufficient studies of this question it is still in doubt the possible impact of this factor on the nature of the disease. Normal colon Mild inflammation in NUC Pathogenesis In the development of inflammation in ulcerative colitis involved multiple mechanisms of tissue and cellular damage. Bacterial and tissue antigens causes stimulation of T and B lymphocytes. In the exacerbation of ulcerative colitis detected immunoglobulin deficiency, which contributes to the penetration of microbes, the compensatory stimulation of B cells with the formation of immunoglobulins M and G. Deficiency of T-suppressor cells leads to increased autoimmune response. Intensive synthesis of immunoglobulin M and G accompanied by the formation of immune complexes and activation of the complement system has a cytotoxic effect, which stimulates the chemotaxis of neutrophils and phagocytes with subsequent release of inflammatory mediators that cause destruction of the epithelial cells. Among the mediators of inflammation the cytokines IL-1ß, IF-y, IL-2, IL-4, IL-15, which affect to the growth, movement, differentiation and effector functions of many cell types involved in the pathological process in ulcerative colitis . Besides pathological immune reactions, damaging action on the tissues have the active oxygen and protease; detected a change in the apoptosis, i.e. the mechanism of cell death. Important role in the pathogenesis of ulcerative colitis is given to the disturbance of the barrier function of the intestinal mucosa and its ability to recover. It is believed that through the defects of the mucous membrane into the deeper tissue can penetrate a variety of food and bacterial agents, which can then trigger a cascade of inflammatory and immune responses. Of great importance in the pathogenesis of ulcerative colitis and provocation of recurrence have features of a patient's personality and psychogenic influence. Individual response to stress with abnormal neurohumoral response may be the trigger for the disease. In the neuro-psychological status of patients with ulcerative colitis there are marked features, which are expressed in emotional instability. Pathologic anatomy In the acute stage of ulcerative colitis there is a marked exudative edema and hyperemia of the mucous membrane with thickening and smoothing of the folds. As the process develops or its transition to chronic increases destruction of the mucous membrane, and formation of ulcers that penetrate only up to the submucosal or, more rarely, to the muscler layer. For chronic ulcerative colitis is characterized by the formation of the pseudopolips (inflammatory polyps). They are islands of mucous membrane, which are maintained , or conglomerate, formed as a result of excessive regeneration of glandular epithelium. Inflammatory polyps (pseudopolyps) of the colon caused by ulcerative colitis In severe chronic course of illness there is a shortened intestine, the lumen is narrowed, wiht no haustrum. Muscular layer is usually not involved in the inflammatory process. Strictures are uncommon for ulcerative colitis. Any part of the colon may be affected in the Ulcerative colitis ,but rectum is always involved in the pathological process, which has a diffuse continuous character . The intensity of inflammation in different segments can be different, and changes are gradually transmits to the normal mucosa, with no clear boundaries. Histological examination in the phase of exacerbation of ulcerative colitis detects expansion of the capillaries and hemorrhage in mucous layer , ulceration as a result of necrosis of the epithelium and the formation of the crypt-abscesses. A decrease in the number of goblet cells, infiltration of the lamina propria by lymphocytes, plasma cells, neutrophils and eosinophils is also discovered . In the submucosal layer changes only slightly expressed, except for the cases of penetration of ulcers in the submucosa. The clinics. Modern clinical classification of ulcerative colitis takes into account the prevalence of the process, the severity of clinical and endoscopic manifestations, the nature of the course of the disease. By the length of the process are distinguished: - Distal colitis (proctitis or in the form of proctosigmoiditis); - Left-sided colitis (lesion of the colon to the right flexure); - Total colitis (affection of the entire colon with involvement in the pathological process in some cases, the terminal segment of the ileum); By the severity of clinical manifestations of the disease- distinguished: light, moderate and severe forms. By the nature of the disease: - Fulminant form; - The acute form (first attack); - Chronic relapsing form (with repeated exacerbations, no more than 1 time in 68 months.) - Continuous form (prolonged worsening - more than 6 months .Despite adequate treatment). There is a correlation between the extent of lesions and the severity of symptoms, which in turn determines the amount and nature of treatment. The diagnosis of ulcerative colitis is formulated on the basis of the nature of the flow (recurrence) of the disease, the prevalence of the process (distal, leftsided and total colitis), disease severity (mild, moderate, severe), the phases of the disease (exacerbation, remission) with local and systemic complications. For example, ulcerative colitis, a total affection, chronic relapsing course, of moderate severity. By the time of diagnosis in approximately 20% of the patients revealed total colitis, 30-40% - left-sided affetion, 40-50% - proctitis or proctosigmoiditis. The clinical picture of ulcerative colitis is characterized by local symptoms (intestinal bleeding, diarrhea, constipation, abdominal pain, tenesmus) and general manifestations of toxemia (fever, weight loss, nausea, vomiting, weakness, etc.). The intensity of the symptoms of ulcerative colitis correlates with the extent of the pathological process in the intestine and the severity of inflammatory changes. Severe total affection of the colon is characterized by profuse diarrhea with a mixture of a significant amount of blood in the stool, sometimes blood clots , cramping abdominal pain before the act of defecation, anemia, symptoms of intoxication (fever, weight loss, severe generalized weakness). In this variant of ulcerative colitis there may develop complications that threaten life - toxic megacolon, perforation of the colon and massive gastrointestinal bleeding. Particularly unfavorable course observed in patients with fulminant form of ulcerative colitis. There are frequent stools up to 5-6 times a day with a constant mixture of blood, cramping abdominal pain, sub febrile fever , body fatigue in moderate exacerbation . A number of patients have extraintestinal symptoms - arthritis, erythema nodosum, uveitis ..etc.Moderate attacks of ulcerative colitis in most cases successfully treated by conservative treatment with modern antiinflammatory drugs, especially corticosteroids. Severe and moderate acute ulcerative colitis is characteristic for total and, in some cases, left-sided affection of the colon. Mild attacks of the disease in total affection of the colon manifested with slightly more frequent stools and with a small mixture of blood in the stool. The clinical picture of patients with proctitis and proctosigmoiditis often manifests no diarrhea, but a constipation and a false urge to defecate with the release of fresh blood, mucus and pus, tenesmus. If in the inflamed distal colon transit of intestinal contents accelerated , but in the proximal segments, there is stasis. This pathophysiological mechanism of constipation associated with distal colitis. Patients may not notice for a long time blood in the stool, general condition suffers little, patients remain not disabled. This latent period between the occurrence of ulcerative colitis before the diagnosis ,can be very long sometimes a couple of years. Complications. In ulcerative colitis observed a variety of complications, which can be divided into local and systemic. Local complications include perforation of the colon, acute toxic dilatation of the colon (toxic megacolon or), massive intestinal bleeding, colon cancer. Acute toxic dilatation of the colon - one of the most dangerous complications of ulcerative colitis. It develops due to severe necrotizing process and the associated toxicity. Toxic dilatation is characterized by the expansion of a segment or all of the affected bowel during a severe attack of ulcerative colitis. Patients with toxic dilatation of the colon at the initial stages requires intensive conservative therapy. If it’s inefficient , then surgical intervention is performed . Perforation of the colon is the most common cause of death in fulminant forms of ulcerative colitis, especially in the development of acute toxic dilatation. Due to extensive necrotizing process , the colon wall becomes thinner, loses its barrier function and is permeable to a variety of toxic products that are in the intestinal lumen. In addition to the overstretching of the intestinal wall, a decisive role in the occurrence of perforation plays bacterial flora, especially Escherichia coli with pathogenic properties. In the chronic stage of the disease this complication is rare and occurs mainly in the form of pericolical abscess. Treatment of perforation is only surgical. Massive intestinal bleeding is relatively rare and as a complication is less complex problem than acute toxic dilatation and perforation of the colon. In the majority of patients with bleeding adequate anti-inflammatory and hemostatic therapy can avoid surgery. In patients with continuing massive intestinal bleeding -urgent surgical intervention is indicated. The risk of colon cancer in ulcerative colitis sharply increases with duration of disease more than 10 years, if colitis began under the age of 18 and, especially, at age of 10. Colorectal cancer of the large intestine caused by ulcerative colitis Systemic complications of ulcerative colitis are also called extraintestinal manifestations. Liver, oral mucosa, skin and joints get affected . The exact genesis of the extraintestinal manifestations is not fully understood. Their formation involves toxic agents that enter the body from the intestinal lumen, and immune mechanisms. Erythema nodosum is found not only in response to receiving sulfasalazine (associated with sulfapiridinom), but occurs in 2-4% of patients with ulcerative colitis or Crohn's disease, regardless of intake of this medicine. Pyoderma gangrenosum - a rare complication that is seen in 1-2% of patients. Episcleritis occurs in 5-8% of patients with acute exacerbation of ulcerative colitis, acute arthropathy - 10-15%. Arthropathy manifests in asymmetrical affection of large joints. Ankylosing spondylitis diagnosed in 1-2% of patients. Liver damage observed in 33.3% of patients with ulcerative colitis and Crohn's disease, which manifests itself in the majority cases in transient increase of transaminase levels in the blood, or hepatomegaly. The most typical serious hepatobiliary disease in ulcerative colitis is primary sclerosing cholangitis, a chronic stenosing inflammation of intra-and extrahepatic bile ducts. It occurs in approximately 3% of patients with ulcerative colitis. Diagnostics. The main research methods: 1) Endoscopy (colonofibroscopy, rectoscopy) - is the primary method of research, which makes it possible to determine the activity of inflammatory and ulcerative process. Pseudopolyps and chronic ulcer of the mucous membrane of the transverse colon. Marked edema with fibrinous raids of mucosa of sigmoid colon. 2) Irrigography - the main radiological signs of ulcerative colitis: narrowing of the intestine, the disappearance of haustrum, jagged and blurred contours of bowel , changes in the structure of mucosa in the form of fine and coarse reticulation (pseudopolyps). . 3) The histological and cytological examination. Histological picture of ulcerative colitis. Additional research methods: a study of the intestinal microflora , immunological parameters, elektrocolography, passage of contrast material in the gastrointestinal tract, ballonography, ballonomanometrical examination, virtual colonoscopy, CT. The diagnosis of ulcerative colitis is set on the basis of an evaluation of the clinical picture of disease, sigmoidoscopic, endoscopic and radiologic studies. On endoscopic picture there are four degrees of activity of inflammation in the intestine: minimum, moderate, severe and sharply expressed. I degree (minimal) is characterized by the swelling of the mucous membrane, hyperemia, lack of vascular pattern, easy contact bleeding, Punctate hemorrhages. II degree (moderate)is determined by edema, hyperemia, granularity, contact bleeding, presence of erosions, drain hemorrhages, fibrinous plaque on the walls. III degree (expressed) is characterized by the formation of multiple merging erosions and ulcers on the background of the developments described above in the mucosa. In the lumen of intestine pus and blood. IV degree (sharply marked), in addition to these changes, is determined by the formation of pseudopolyps and bleeding granulations. A severe form of ulcerative colitis of A severe form of ulcerative colitis of the the rectum sigmoid colon In the remission stage mucosa is thickened and vascular pattern restored, but not completely . Mucosa grain can be stored , thickened folds are retained. In some countries, to assess endoscopic activity of ulcerative colitis proposed endoscopic index Rahmilevich , that accounts for the same symptoms, evaluated on a scale. Endoscopic index (Rahmilevich ) (1989) 1. The scattering light granular mucosal surface (grain): No - 0, yes - 2. 2. Vascular pattern: normal - 0, deformed or blurred - 1, absent - 2. 3. Mucosal bleeding: absent - 0, a small contact – 2 marked (spontaneous) - 4. 4. Damage to the mucosal surface (erosion, ulceration, fibrin, pus): None - 0, moderately expressed - 2, considerably expressed - 4. Often at high activity of the process surface of the intestinal mucosa completely covered with fibrinopurulent raid, after the removal of which revealed diffuse granular bleeding surface with multiple ulcers of varying depth and shape with no signs of epithelialization. For ulcerative colitis typical round and star-shaped sores, ulcers- prints, usually which do not penetrate deeper lamina propria mucosa, rarely - in the submucosal layer. In the presence of multiple ulcers or erosions micro mucous membrane looks like a moth-eaten. For ulcerative colitis in the active stage of the process under study with barium enema X-ray very typical following symptoms: the absence of haustrum, smoothed contours, ulceration, edema, serrated surface, double loop, pseudopolyps, the restructuring of the longitudinal folds of the mucous membrane, the presence of free mucus.At the late stages of ulcerative colitis due to edema may develop thickening of the mucosal and submucosal membranes. This increases the distance between the rear wall of the rectum and the anterior surface of the sacrum. After emptying the colon of barium , the absence of haustrum, predominantly longitudinal and rough transverse folds, ulcers and inflammatory polyps can be revealed. X-ray examination is of great importance not only to diagnose the disease, but its severe complications, including acute toxic dilatation of the colon. That is why radiography of the abdomen is performed . When I degree dilatation ; the diameter of intestine in its widest point is about 8-10 cm, II - 10 - 14 cm and III - over 14cm. In the process of treatment of ulcerative colitis attack- positive dynamics of all major radiologic manifestations of the disease is noted - reducing of the length, size and tonus of intestine. This is due to the fact that during irrigoscopy these changes manifest themselves with spasm, not with organic narrowing typical for granulomatous colitis and intestinal tuberculosis. The differential diagnosis. The clinical picture of ulcerative colitis requires the differential diagnosis of diseases of the colon infectious and noninfectious etiologies. The first attack of ulcerative colitis can occur under the mask of acute dysentery. Correct diagnosis can be obtained by the help of sigmoidoscopy and bacteriological study. Salmonellosis often simulates the clinic of ulcerative colitis, as occurs with diarrhea and fever, but unlike him, bloody diarrhea appears only at the 2nd week of illness. From other forms of colitis of infectious origin, which requires differentiation from ulcerative, it should be noted gonorrheal proctitis, pseudomembranous enterocolitis, viral diseases. The most difficult differential diagnosis is between ulcerative colitis, Crohn's disease and ischemic colitis. Ulcerative colitis Crohn’s disease It is necessary a colonoscopy with biopsies from different parts of the colon, a comparison of macroscopic changes (broad ulceration in non-specific colitis and longitudinal ulcers, fissures in Crohn's disease) and microscopically (crypt abscesses, in the first case , and sarcoid granulomas in the latter). The main modern diagnostic method for verification of non-specific colitis colonoscopy. In the active form of ulcerative colitis diffuse erythema, ulceration, and friability (contact bleeding) of mucosa is revealed, granulation can be traced from the anorectal level - proctitis; to the cecum - pancolitis. The rectum is almost always affected. In Crohn's disease the picture is somewhat different: ulcers are more outlined in the borders, intestinal fistulas are detected, pseudopolyps, narrowed parts, which creates the above mentioned picture of a cobblestone street. The rectum is affected not always, while the terminal ileitis is very typical. Biopsies from different parts of the inner wall of the colon in ulcerative colitis reveals the infiltration with polymorphic and mononuclear cells of the basement membrane cells, there are multiple crypt abscesses, intestinal crypts are underwent to atrophy , in goblet cells the amount of mucus is decreased. J. Rumessen (1996)in electron microscopy of resected preparations in ulcerative colitis in submucosal layer discovered the so-called Cajal cells and believed that this is the pacemaker of smooth muscles of the intestinal wall and that the primary or secondary destruction of these cells plays an important role in the pathogenesis of ulcerative colitis. In Crohn's disease infiltration of basement membrane with macrophages and leukocytes deeper (at the surface of the biopsy may not be visible), in 20-40% of cases are detected tuberculoid granuloma, based on which many believed that Crohn's disease is a variant of intestinal tuberculosis, which not only proved but now completely denied. W. Chen et al. (1997) brings result in the greatest, perhaps, in recent years, the experience of observation and treatment of tuberculosis of the colon: in 30 years they have seen 70 patients, of whom in 59 correct diagnosis was made only during surgery, and in 11 in the preoperative biopsy.The clinical picture and changes in the colon did not match ulcerative colitis or Crohn's disease. In addition, the greater part of the patients (48 patients) had an active or old pulmonary tuberculosis, including in 18 bacillary form, while another 22 had disseminated form of tuberculosis. Symptoms mainly consisted of intestinal obstruction of varying severity, and in colonoscopy and irrigoscopy intestine constriction is found. Of the 70 patients 59 were operated on the background of active specific chemotherapy, while the remaining 11 was successfully carried out only with chemotherapy. In 19 cases performed right- sided hemicolectomy , segmental resection of the narrowed sections of intestine or, more often, a biopsy, after which was held active specific medication. After this work it can be assumed that tuberculosis of the intestine, and Crohn's disease - are different diseases. There is a very informed opinion about the importance in the pathogenesis of non-specific colitis circulatory disorders of the colon in some of its parts, for example, in the left flexure of the colon, which can partly be explained by structural features of the arteries of this area which are relatively far removed from the bowel wall. In other words, it is believed that in many cases, ulcerative colitis is ischemic colitis. In support of this hypothesis there are a few facts older age at onset of disease in many patients, the combination of colitis with ischemic heart disease and prolonged hypotension, original or accompanying atherosclerosis. On the other hand, in specialized clinics we can see young patients with ulcerative colitis who do not have any circulatory disorders. There are reliable data on the relatively greater incidence of disease among certain racial groups, etc. But while all this information can not be systemized, the true etiology of nonspecific colitis remains unclear. The differential diagnosis, again, very difficult, especially due to the prolonged unskilled treatment and, especially, inadequate self-application of antibiotics and steroid hormones. Infectious colitis, differ from these diseases mainly with epidemiological history and findings at feces seeding. In all cases, it is important to study the feces for eggs of intestinal worms and parasites, microbiological examination of the most common of cultures in our time, agents of dysentery - campilobacter, salmonella, shigella. Multiple comparisons of clinics and course of ulcerative colitis and Crohn's disease, attempts to bring it into the scheme, often help the researchers visualize at least their basic differences. One of these scheme is the data about systemic complications which are very characteristic of these non-specific colitis. This arthritis (Crohn's disease), sacroiliitis, affection of the eye (iritis, uveitis), erythema nodosum, pyoderma gangrenosum, sclerosing cholangitis (ulcerative colitis). Our previous long-term experience in treating ulcerative colitis (A. Bronstein, 60-70s, the work of other employees of the Moscow Institute of Proctology - MH Levitan et al., 1974.1984) and our own observations of recent years in the United States allow highlight though similar, but distinguishable for the clinician important details of the course of the two major forms of chronic nonspecific inflammatory diseases of the colon. Let's start with Crohn's disease. You can identify at least five major symptoms and characteristics: 1) Pain in the abdomen. Almost constant, especially in the right iliac region (regional ileitis) associated with increased peristalsis , less often pain alternate with intervals of light periods and appear in different parts of the abdomen depending on the severity of inflammation in the segments of the colon. Often before stool there is colicky pain that precedes the release of semi-liquid stool. After defecation, such kind of pain usually disappears; 2) Diarrhea - liquid, or more often semisolid stools with mucus and blood. The more distal location of affected part , the more often stools and thus false urges. The number of defecations usually no more than 4-6 per day, which is clearly different from the profuse diarrhea in ulcerative colitis; 3) Almost pathognomonic sign of Crohn's disease is a fever, especially "for no apparent reason." But anyway the reason is quite apparent ; subfebrilitet is a clear indication of system complications; the formation of perianal abscesses and fistula ,the formation of intraabdominal infiltration along the colon and in the right iliac region (regional ileitis) 4) pararectal fistula with the release of pus, mucus, and sometimes a liquid stool. Fistulas are usually multiple, with several external openings and with a very difficult verification of their internal openings. This typical sign, marked by the author of the first descriptions of the disease (A. Penner, B. Crohn, 1938). Fistulas can be superficial, subcutaneous, or even extrasphinctral transphincintral , reaching outward from the primary rectal sphincter muscle ,; fistula causes almost constant local pain , for patients it is difficult to sit, it is necessary to use always the pads, etc. 5) Malnutrition. Weight loss, followed by electrolyte imbalance , anemia - typical signs of chronic suppurative ulcerative process of the colon in Crohn's disease. At the same time often observed seizures of partial or even total intestinal obstruction due to inflammatory bowel strictures and intestinal adhesions. This complication dramatically aggravates the patients condition . Now about ulcerative colitis. The disease begins suddenly and can manifest itself in moderate, severe, and fulminant forms. In moderate forms disease starts with diarrhea with insignificant amount of blood and mucus. This can last constantly for a long time or with a short breaks for many months. In severe and, especially, fulminant forms, disease begins explosively, with serious profuse diarrhea with profuse bleeding and the development of toxic dilatation of colon (toxic megacolon), which represents a threat to the lives of patients. We can distinguish four characteristic and a bit different from Crohn's disease symptoms: 1) Diarrhea- have different intensities - from loose stools 3-4 times a day to almost constant watery discharge (in fulminant forms of the disease). Very typical diarrhea at night, greatly aggravating the condition of patients, and false urges (tenesmus).Note that sometimes, however, very rarely, there are no diarrhea, but constipation. 2) Rectal bleeding - from a small mixture of blood in feces to massive hemorrhage requiring urgent measures; 3) Abdominal pain can be constant, but more often they are colicy, preceded by the act of defecation, and disappear after stool. In acute and fulminant forms of the disease with the occurrence of acute toxic dilatation of the colon there appears signs of irritation of the peritoneum, the pain intensifies and do not stop; 4) Anorexia and weight loss are characteristic, as well as in Crohn's disease, especially in younger patients. There is a sharp weakness, anemia, fever up to 38-39 ° C, "sick look" up to cachexia. From extraintestinal manifestation there are often already mentioned above, arthritis, nodular erythema of the skin, aphthous ulcers in the mouth. Note that for a long-lasting ulcerative colitis with frequent relapses in 5-10% of patients there is a severe complication called acute toxic dilatation of the colon, often early in the disease At colonoscopy, which is absolutely necessary, will be specified the prevalence and severity of the process of inflammation. Endoscopic picture shows the contact vulnerability of the mucous membrane, swelling of the intestine walls , areas covered with granulations. Multiple ulcers can be mixed with very small intact areas.Polypous growth (pseudopolyps) on the legs and on broad bases covered by hyperemic and easily bleeding mucosa are determined. Pseudopolyps appear early, and their inflammatory nature is confirmed by biopsy, but the world and our personal experience has clearly shown the possibility of malignant transformation sites in colonic mucosa in these patients, as already mentioned and will be discussed below. Differentiate ulcerative colitis and Crohn's disease from other inflammatory bowel diseases is difficult, but distinctive features are present, and they need to be noted. More about this will be discussed below, often after intensive antibiotic therapy , various intercurrent diseases there are colitis characterized by the presence of pseudomembranous findings and clostridia in the feces, and right-sided colitis, often caused by Klebsiella. It is important to differentiate non-specific colitis with intestinal infections in homosexual men in whoh may be found Gonorrheal, Chlamydia, syphilis, cytomegalovirus colitis and infection with herpes simplex. In these patients, as in immunosuppressive (especially AIDS), visually detected by endoscopy violet mucosal sites with clear boundaries, and swelling of the mucous, as well as in Crohn's disease, stenosis and bowel pseudopolyps. For diverticular disease of the colon is characteristic localized areas of hyperemia on the tops of the folds of hypertrophic mucosa , at colonoscopy the holes of the diverticulas are visible , mostly in the sigmoid colon. There is also a form of colitis, clinically similar to non-specific, in which revealed elongated, twisted and extended intestinal crypts and polypous growths, which ulcerated surfaces as if covered with a hat ("pileate" polyposis). Radiation damage of the colon is very similar during endoscopy with nonspecific colitis. They are differentiated by history. Nonspecific colitis should be distinguished from lymphoma, changes in the hemolytic uremic syndromes ,Behcet's disease, etc., but in practice the differential diagnosis is conducted between ulcerative colitis and Crohn's disease, which, again, very difficult. Even after removing the entire colon in 1015% of cases, pathologists can not fully determine the nature of the lesion. Treatment. Therapeutic tactics in ulcerative colitis determined by the localization of the pathological process in the colon, its extent, severity of attacks, presence of local and / or systemic complications. Conservative therapy is aimed at the most rapid relief of an attack, preventing disease recurrence and progression. Distal forms of ulcerative colitis - proctitis or proctosigmoiditis - characterized by a mild course, so ,often treated as outpatients. Patients with left and total affection of the colon, as a rule, are treated in the hospital, as the disease has more clinical symptoms and greater organic changes. Food of patients should be high-calorie and include products rich in proteins, vitamins, should be limited -animal fat and crude fiber should be excluded . Recommended low-fat varieties of fish, meat (beef, chicken, turkey, rabbit) boiled or steamed, pureed oatmeal, potatoes, eggs, dried bread, walnuts. Should be excluded from the diet raw fruits and vegetables, as they contribute to the development of diarrhea. Often, patients have lactase deficiency, so dairy products are added only when they are well tolerated. These recommendations are consistent with diets 4, 4B, 4B, Institute of Nutrition of RAMN. All drugs used in treatment regimens of ulcerative colitis can be divided into two groups. The first combines the basis anti-inflammatory drugs and includes aminosalicylates, ie, drugs that contain 5-aminosalicylic acid (5-ASA, mesalazine), corticosteroids and immunosuppressants. All other drugs play a supporting role in the treatment of ulcerative colitis, or are under clinical study. The first drug in its composition containing 5-ASA- sulfasalazine was (salazosulfapiridina) introduced into clinical practice in 1942. Sulfasalazine consists of two components associated with each nitrogen bond - sulfapiridina sulfanilamide and 5-ASA. It is proved that anti-inflammatory action has only 5ASA. Sulfapiridin was forcibly included in the molecule sulfasalazine, as "pure" 5-ASA is well absorbed in the small intestine mucosa and converted into an inactive metabolite - N-acetyl-5-ASA. Sulfapiridin sulfasalazine acts solely as a "carrier" that can deliver 5-ASA to the affected areas of the colon. Under the influence of colonic microflora nitrogen bond is destroyed. Sulfapiridin absorbed in the colon and exposed in the liver to detoxification by acetylation and is excreted in the urine, and 5-ASA by contacting with mucous membranes provides its anti-inflammatory effect. Mechanisms by which 5-ASA provides anti-inflammatory effects are not fully understood. However, many effects are known by which mesalazine inhibits the development of inflammation. Thus, through inhibition of cyclooxygenase mesalazine inhibits the formation of prostaglandins. Also inhibited lipooxyginase pathway of arachidonic acid, leukotriene B4 inhibited the release of leukotrienes and sulfopeptida. At high concentration mesalazine can inhibit certain functions of neutrophilic granulocytes in humans (eg, migration, degranulation, phagocytosis and the formation of toxic free oxygen radicals). In addition, mesalazine inhibits the synthesis of a factor, which activates platelets. Due to its antioxidant properties, mesalazine is capable to capture free oxygen radicals. Mesalazine inhibits effectively production of cytokines - interleukin-1 and interleukin-6 (IL-1, IL-6) - in the intestinal mucosa, but also suppresses IL-2 receptor. Thus mesalazine interferes directly in the immune processes. It was shown that the "ballast" component sulfapiridin is primarily responsible for the entire frequency of side effects of sulfasalazine. The literature data on the incidence of adverse effects caused by sulfasalazine, ranges from 5 to 55%, averagely 21%. In addition to nausea, headache, male infertility there may be anorexia, dyspepsia, haematological reactions (leukopenia, and hemolytic anemia) and hypersensitivity reactions with polyorganic insufficiency. In order to maintain anti-inflammatory activity inherent in the sulfasalazine and avoid side effects associated with sulfapiridin component in recent years developed products containing "pure" 5-ASA. As an example of a new generation of aminosalicylates can cause drug “salofalk” developed by German pharmaceutical company, "Dr. Falk Pharma." The drug is available in three dosage forms: tablets, suppositories and micro enema. In tablets, mesalazine is protected from contact with gastric contents using a special acid-resistant polymer shell, which dissolves at pH above 6.5. These are the pH values usually recorded in the lumen of the ileum. After dissolution of the shell in the terminal ileum a high concentration of the active component in noted in the lumen of the colon. The choice of the dosage form is determined by the extent of the affected zone in the colon. If proctitis it is advisable to use suppositories ,in left –side colitis –micro-enemas and in total colitis - pills. Recently appeared in Russia pentasil, being as effective, has several features. It differs from other drugs of mesalazine with microgranulated structure and character of the coating. The tablets are composed of pentasil microgranules in ethylcellulose shell dissolution of which is independent of pH in the gastrointestinal tract. This provides a slow, gradual and steady release of 5-ASA throughout the intestine, from duodenum. The steadiness of the release contributes to a constant concentration of drug in different parts of the intestine, which does not depend not only on pH but also on the speed of transit, so the pentasil can be successfully used in inflammatory bowel diseases and diarrhea without actual loss. This feature allows to use the drug not only in ulcerative colitis and Crohn's disease with lesions of the colon and ileum, but also, more importantly, in patients with highly localized (duodenum) Crohn's disease. Daily dose of aminosalicylates determined by the severity of attack of ulcerative colitis and the nature of clinical response to the drug. For relief of severe and moderate attacks 4-6 g of sulfasalazine or mesalazine 3-3.5 g per day is administered, divided into 3-4 doses. In the absence of good clinical response daily dose of mesalazine may be increased to 4.0-4.5 g, but to increase the daily dose of sulfasalazine is usually not possible because of side effects. Sulfasalazine blocks the conjugation of folic acid in the brush border of jejunum, inhibits the transport of the this vitamin, inhibits the activity of the associated enzyme systems in the liver. Therefore, in complex treatment of these patients should include folic acid in a dose of 0.002 g 3 times a day. Relief of attacks of ulcerative colitis usually takes 3 - 6 weeks treatment . After that should be continued anti- relapse therapy in a dose of sulfasalazine (3 g / day) or mesalazine (2 g / day). Of modern drugs for the treatment of proctosigmoiditis and left-sided colitis most commonly used suspension of salofalk. In the disposable containers respectively containing 4 g mesalazine in 60 mL of a suspension or 2 g mesalazine in 30 mL of suspension. The drug is introduced into the rectum 1-2 times a day. The daily dose is 2-4 g, depending on the severity of the process . If the extent of inflammation in the rectum not more than 12 cm from the edge of the anus, it is advisable the use of salofalk suppositories. The usual daily dose in these cases - is 1.5-2. By using aminosalicylates can be achieved remission in 75-80% of cases of ulcerative colitis. The most effective anti-inflammatory drugs in the treatment of ulcerative colitis are steroid hormones, which in severe forms of disease by activity surpass aminosalicylates. Corticosteroids accumulate in the inflamed tissues and block the release of arachidonic acid, preventing the formation of prostaglandins and leukotrienes, which determine the inflammatory process. Blocking chemotaxis, by steroid hormones indirectly exhibit immunomodulatory effects. The effect on tissue fibrinolysis reduces bleeding. Indications for steroid therapy are: - Acute severe and moderate forms of the disease and the presence of extraintestinal complications; - left sided and total forms of ulcerative colitis with severe and moderate course in the presence of the III degree of inflammatory changes in the bowel( endoscopic examination); - Lack of effect from other treatments for chronic forms of ulcerative colitis. In acute severe ulcerative colitis or severe attacks of chronic forms of disease treatment should be started with the intravenous administration of prednisolone at least 120mg/day evenly distributed on 4-6 injections with simultaneous correction of fluid and electrolyte disturbances, administration of blood and blood substitutes, and (if possible) of the hemosorption for the rapid elimination of endotoxemia. Suspension of hydrocortisone should be administered intramuscularly, but the duration of such issuance is limited to 5-7 days because of the probable development of abscesses at injection site and possible fluid retention. After 5-7 days treatment should be switched to oral administration of prednisolone. During this time, gastroscopy should be performed to exclude gastric ulcer and duodenal ulcer. In the moderate forms and in the absence of clinical signs, as well as anamnestic indications for gastroduodenal ulcers , treatment should be immediately started with oral administiration of prednisolone. Usually prednisolone administered at a dose of 1.5-2 mg / kg body weight per day. Dose of 100 mg should be considered as a maximum. If there is a good tolerability to hormonal drugs, prescribed dose is recommended to take until obtaining stable positive result - within 10-14 days. After this dosage decrease is carried out by the so-called step scheme - to 10 mg every 10 days. From 30-40 mg it is recommended a single dose of prednisone in the morning, that practically cause no serious complications. At the same time, to the regimen should be included mesalazine or sulfasalazine, which must be taken to the full cancellation of hormones. From 30mg, withdrawal of prednisolone conducted more slowly - by 5mg per week. Thus, the full course of hormone therapy lasts from 8 to 12 weeks depending on the form of ulcerative colitis. At the distal forms and I-II degree of activity of the process according to sigmoidoscopy hydrocortisone in drips or microenema should be administered rectally .Moreover, if patients can’t hold large volumes, then hydrocortisone should be administered (65-125mg) in 50 ml of isotonic sodium chloride solution and as the extent of inflammation subsides and the frequency of false urges reduces therapeutic enema is gradually increased up to 200-250 ml . The drug is usually administered after stool in the morning or at bedtime. In ulcerative proctitis and sphinctiritis fairly good effect have suppositoruim with prednisolone (5 mg) administered 3-4 times a day. In more severe distal forms accompanied by fever, general weakness, anemia, and III - IV degree of activity according to rectoscopy, where there is no effect of sulfasalazine or mesalazine treatment - indicated prednisone orally at a dose of 30-50 mg / day. In middleaged and elderly patients the dose of prednisolone should not exceed 60 mg, since this age is characterized by the presence of concomitant diseases: atherosclerosis, hypertension, diabetes, etc. In cases where ulcerative colitis occurs on the background of atherosclerosisof mesenteric arteries, to medical complex should be included cardiovascular drugs: trental, prodektini etc. Hormonal therapy is associated with adverse effects: retention of tissue fluid and sodium chloride (possible edemas), hypertension, hypokalemia, loss of calcium, osteoporosis, and various vegetative disorders, carbohydrate metabolism disturbance, adrenal insufficiency, gastric ulcers, gastrointestinal bleeding . In these cases it is recommended adequate symptomatic therapy : antihypertensive drugs, diuretics, calcium preparations, antacids. In case of carbohydrate metabolism disturbance , required diet with the restriction of carbohydrates ,by indications – fractional adminidtration of insulin (or glucose) or oral antidiabetic drugs. For the prevention of thrombosis in patients with severe ulcerative colitis receiving hormonal treatment should be conducted continuous monitoring of blood coagulation and simultaneously administered Antiplatelet: kurantil , prodektin. In recent years at the treatment of inflammatory bowel diseases, especially Crohn's disease, widely used preparations containing as an active component glucocorticosteroid budesonide. In contrast to conventional glucocorticosteroids budesonide has a very high affinity to receptors, and high (90%) metabolism in the liver at first pass. Due to this, he has a very strong local anti-inflammatory action with minimal systemic side effects. As an alternative to prednisone and hydrocortisone can be recommended drug budenofalk. At he development of budenofalk accounted physiological characteristics of the gastrointestinal tract. Each capsule contains about 350 budenofalk microspheres consisting of budesonide, coated with polymer coating which is resistant to gastric juice. Exemption of budesonide from the microspheres occurs in the ileum and colon at pH values above 6.4. Budenofalk is used to treat light and moderate exacerbations of ulcerative colitis. The recommended daily dose is 1 capsule of budenofalk containing 3 mg of budesonide, 4-6 times a day. The most serious problem in the treatment of ulcerative colitis is a hormonal dependence and resistance. In this contingent of patients recorded the worst results of conservative treatment and the highest surgical activity. According GNTSK, hormonal dependence is formed in 20-35% of patients with severe ulcerative colitis. Often the symptoms of dependence and resistance are observed simultaneously, forcing to use unsafe and aggressive methods of treatment. Hormonal dependence - a reaction to the glucocorticoid therapy, in which a positive therapeutic effect followed by a reactivation of the inflammatory process in the background of dosage reduction or cancellation of corticosteroids. This is a special variant of refractory colitis. We believe that there are at least four different etiopathogenetic variants of hormonal dependence: real hormonal dependence, combined with steroid-resistence, false, due to inadequate treatment, actual chronic adrenal failure, and its mixed or combined forms. At the present time the causes and mechanisms of hormonal dependence is unknown . Nevertheless, we believe that a number of etiologic factors undoubtedly find a place : defects of hormonal therapy, persistent activity of inflammation, transient or persistent reduction of pituitary-adrenal function. Probably, in some cases, hormonal dependence and resistance are hereditary, in others - defect of hormonal receptors and an imbalance between cell proliferation and cell death, ie, the misalignment of apoptosis are acquired. The hypothesis of a low density of hormone receptors in patients with inflammatory diseases of the colon, especially in refractory course, recently received a convincing proof. Immunosuppressive drugs play crucial role in the treatment of patients with inflammatory bowel diseases with hormonal dependence and resistance. However, the role of various drugs is considered ambiguous. Among the products of the 1st line and long-term use are 6-mercaptopurine and azathioprine. They are excellent sparring partners for glucocorticoids. Purine analogs allow to reduce and cancel the hormones in 60-70% of patients with hormonal-dependence under certain rules, namely, they should be given simultaneously with hormones so that their action has had time to manifest. The daily dose of azathioprine should be no more than 150 mg. The effect can only be expected by the end of third month of continuous reception. Purine analogues give relatively few side effects and should be used in patients with hormonal dependence as long as possible - 2-3 years or more. Medication of the 2nd line for long-term therapy is methotrexate, which is used in the case of intolerance for azathioprine or to accelerate effect. It is administered orally or intramuscularly at a dose of 30 mg / week. The result can be obtained within 2-4 weeks. Side effects are rare. Unfortunately, like azathioprine, it does not provide a consistent effect. After cancellation occurs quickly exacerbation. Sometimes outbreaks lighter than before can occur during therapy after 6 months, from the beginning of the reception. Cyclosporine can be used orally, intravenously at a dose of 4-6 mg / kg body weight with a good and quick effect, coming within 5-7 days. Unfortunately thee effect is briefly. Its often used to interrupt the attack with subsequent switch to immunosuppressive drugs that are suitable for prolonged administration. Disturbance at the barrier function of the colon in ulcerative colitis may be the cause of the toxemia syndrome. Its correction requires the administration of an appropriate complex of treatment : eubioz restoration, antibiotic therapy, hemosorbtion, UV of blood. Due to marked metabolic disturbances and the catabolic actions of steroid hormones , advisable parenteral administration of protein drugs: human serum albumin, plasma proteins, essential amino acids. To improve the processes of microcirculation and transcapillary exchange indicated administration of reopoliglyukin, gemodez (in normal dosages). When anemia (hemoglobin 90 g / L and below), which is a sign of severe attacks of ulcerative colitis, recommended to perform blood transfusion in a volume of 250 ml of single-group blood with intervals of 3 - 4 days. If there is decrease in the level of serum iron , iron preparations is administered . Immunomodulaters like timalin , levamisole , etc are used in immulogical disorders . However, their role is unclear, the therapeutic effect of their is shortterm, the use of these drugs as the basic is questionable. It is advisable to use immunomodulators in conjunction with the basic antiinflammatory medication. Vitamins B complex, C, A, D, K, are administered to o contribute to the restoration of normal eubioz . To the medical complex should be included psychotropic drugs in normal dosages, focusing on individual tolerance. Exacerbation of ulcerative colitis in some cases accompanied by irritable bowel syndrome with constipation . In this case approved the use of the wheat bran or preparations containing ballast substances (mukofalk, etc.) that contribute to the normalization of the stool and at the same time effect as enterosorbent . Inpatient treatment ends when there is a clinical and endoscopic remission obtained , after which the patient should be discharged to the control of therapist, gastroenterologist or proctologist. Surgical treatment. Surgical interventions in ulcerative colitis requires 10-20% of patients. Surgical technique may be radical, but it means complete removal of the colon as a possible substrate of disease recurrence. However, this severe traumatic surgery results in the vast majority of patients to the loss of anal defecation and the formation of a permanent ileostomy in the anterior abdominal wall. In fact, the operated patients become disabled, and this significantly limits the use of surgical treatment. Indications for surgery currently divided into three main groups: 1. Inefficiency of conservative treatment; 2. Complications of ulcerative colitis (intestinal bleeding, toxic dilatation of the colon, perforation of the colon); 3. Emergence of colorectal cancer in the background of ulcerative colitis. GNTSK has experience of surgical treatment of more than 500 patients with ulcerative colitis. In recent years, developed and introduced an integrated approach for the management of patients, including intensive therapy in the preoperative period, early identification of the indications for surgery, effective rehabilitation in the postoperative period. New technologies are used in surgical intervention, including a sparing operating (laparoscopically assisted surgery, Ultracision, Ligasure). Objective of surgical rehabilitation is a differentiated approach with various options to restore anal defecation. All these approaches have helped to reduce the frequency of postoperative complications from 55 to 12%, and mortality from 26 to almost 0%. Primary and delayed reconstructive operations became possible in 53% of operated patients. Indications for surgery. Inefficiency of conservative treatment. In most patients it is impossible to prevent the progression of inflammatory changes with medication, including hormones (hormone-resistant form). Continues attack of ulcerative colitis, severe intoxication and blood loss leads to the depletion of the patient , profound metabolic disturbances, anemia carry the risk of septic complications. In these cases, the necessity of the surgical intervention is decided. Preoperative preparation includes intensive conservative treatment, correction of anemia, hypoproteinemia, and electrolyte disturbances. Duration for the effect of conservative therapy is 2-3 weeks , after the beginning of a complex intensive therapy with an adequate dose of glucocorticoids (prednisone 2 mg / kg / day). In a certain group of patients (20-25% of severe) noted so-called hormonedependent ulcerative colitis. In these group of patients continuous hormonal therapy (oral prednisone 15-30 mg per day necessary to retain remission. Longterm hormone treatment for 6 months and more involves the development of serious adverse effects: a steroid diabetes, osteoporosis with pathologic fractures, arterial hypertension, etc. This also dictates the need for surgery, which allows not only to cancel the corticosteroids, but also to eliminate the focus of the inflammation. Intestinal bleeding. Loss of blood through the rectum in ulcerative colitis is rarely dangerous. However, sometimes the blood loss can not be conservatively corrected and in these cases it becomes life-threatening . In such cases, a decision about the operation should be made , without waiting for the effect of the ongoing anti-inflammatory drugs, including steroids, haemostatics, transfusion of blood products, control of hypovolemia. It is important to objectively assess the amount of blood in patients faeces ,a visual assessment, not only by the patient, but the doctor is usually inadequate. The most accurate method of determining blood loss is a radioisotope study, which allows you to label red blood cells withchromium , technetium isotope and determine the daily amount of erythrocytes in the stool. When blood loss 100 mL per day or more – operation is indicated . Such an objective assessment of blood loss is not possible everywhere and always. Indirect criteria of severity of bleeding is diarrhea more than 10 times a day with the intense bloody stool at the volume of more than 1,000 ml per day, maintaining initial indications despite blood transfusion. Toxic dilatation of the colon is the result of cessation of peristaltic contractions of the colon wall, which leads to the accumulation intestinal contents, including a large amount of gases. Colon in these conditions significantly expands up to a critical level - 9-15 cm in diameter. Threatening symptoms of dilatation are sudden slow of stool against the background of the original diarrhea, bloating, increased pain and an increase of the symptoms of intoxication. A simple and valuable diagnostic technique is the dynamic X-ray of the abdomen, in which maybe noted the growth of pneumatosis of the colon and expansion of its lumen. At the dilation of 6-9 cm (I degree of dilatation) should be conducted attempt of endoscopic decompression (the evacuation of the contents through the colonoscope). The preservation dilation, as well as its increase (9-11 cm - II degree, 11-15 cm - III degree) is an indication for emergency surgery. Perforation of the colon usually occurs on the background of increasing toxic dilatation if there is unreasonable refusal from timely surgery. The cause of the perforation is a deep ulcerated defect with necrotic changes in all layers of the intestinal wall. It is important to keep in mind that on the background of the intensive hormonal therapy, antibiotics, antispasmodics and analgesics in patients with perforations a classical picture of acute abdomen is absent , so to put correct diagnosis is very difficult . Appearence of the free gas in the abdomen in x –ray helps in this situation. The success of surgery depends on the timeliness of diagnosis and duration of peritonitis. Cancer on the background of ulcerative colitis. In a population of patients with ulcerative colitis colon cancer occurs significantly more often, especially when disease duration is more than 10 years. Adverse features are: poorly differentiated malignant forms of tumor, multiple and rapid metastasis, massive destruction of the colon by tumor. In ulcerative colitis sometimes occurs so called total form of colon cancer, when tumor growth histologically found in all parts, while visually colon may remain characteristic of chronic inflammatory process. The main methods of secondary prevention of cancer in ulcerative colitis is an annual clinical examination of patients, especially with total forms of the disease with duration over 10 years, and multiple mucosal biopsies, even in the absence of visual changes. Detection of dysplasia in mucosal biopsy specimens should be regarded as precancerous and be reason for a more thorough and frequent examination. The choice of surgical intervention. In ulcerative colitis radical surgery is the total removal of the colon with the formation of a permanent single-barrel ileostomy by Brooke. However, surgeons are looking for ways to rehabilitate this severe category of patients by developing various reconstructive operations with the restoration of anal defecation. In addition, single-stage traumatic colprockectomy may be the cause of increased morbidity and mortality in patients in a critical initial state. Operation of choice in surgical treatment of severe ulcerative colitis is the subtotal resection of the colon with ileostomy and sigmoidostomy formation. In this case, should be carried out intensive treatment of stored segment of the colon in the postoperative period - hormones in microenema and suppositorias, mesalazine-locally , metronidazole, intestine decontamination with antiseptic and astringent solutions. A variant of resection may be the type of colectomy – Hartmann operation , for example, if perforation has occurred at the distal part of sigmoid colon or sigmoid colon was the source of bleeding. In the late postoperative period at terms of 6 months up to 2 years the 2 stage of surgical intervention is decided.Formation of ileorectal anastomosis is performed in the absence of relapses of ulcerative colitis at the rectum(with preventive ileostomy or not). If stricture has developed at the rectum ,then abdomino-anal resection of rectum and stored part of the colon is performed. Reconstructive phase in this case may be the formation of reservoir from small intestine (rectum ampulla autoprotesis) with ileoanal anastomosis and preventive ileostomy. Preventive ileostomy in both cases is shut after the healing of anastomosis in 1 - 2 months. it should be noted that even the formation of anastomosis between the small intestine and anorectal line can not guarantee recovery from ulcerative colitis, since in 25-30% of patients in 3-5 years after such an operation rectal mucosa regenerates at small intestine reservoir even with the possible malignancy. One-stage colectomy with abdominoanal resection of rectum is used in massive intestinal bleeding when the source of bleeding is rectum. Moderate course of ulcerative colitis with the satisfactory condition of the patient may also be a reason for surgery if the disease is hormone-dependent form. In this case, itbis possible to perform one-stage surgery with reconstructive phase - a colectomy with the formation of ileorectal anastomosis or colectomy with abdomino-anal resection of the rectum, formation of ileoreservoir with preventive preventive ileostomy. Colectomy with abdomino-anal resection of the rectum is used in the development of the colon cancer on the background of ulcerative colitis. Colectomy with abdominoperineal extirpation of the rectum is performed when tumor is located in rectum. Surgery for cancer is usually finished with the formation of a permanent single-barrel ileostomy by Brooke. Post-operative complications. Poor initial condition of the majority of patients prior to surgery affects to the postoperative period,to the development of postoperative complications and mortality. Complications commonly associated with poor tissue regeneration in debilitated patients (eventration, intestinal suture failure )serous peritonitis, pleural effusion as a manifestation of poliserositis, abdominal abscesses, ileostomy dysfunction and pneumonia.Active tactics of the surgeon are very important in the development of complications associated with debilitated condition of patients. In operations for intestinal bleeding, toxic dilatation and perforation of the colon after surgery reaches 60-80% and mortality ranges from 12 to 50%. In cases of early surgical intervention in the specialized hospital complications and mortality is not higher than for other abdominal operations, accounting for 812% of postoperative complications and postoperative mortality of 0.5-1.5%. Prognosis after surgical treatment. Timely performance of the operation with dynamic observation makes the prognosis favorable. If rectum is stored it requires annual monitoring with multiple biopsies . Most patients are long-term disabled (need disability registration). Scenario of POO for diarrhea syndrome The teacher offers to discuss the management of patients with diarrhea and constipation syndrome. The teacher divides the group into 2 subgroups. By tossing assignment is pulled. 1"Dispensary observation of patients with the syndrome of diarrhea." 2. "Dispensary observation of patients with the syndrome of constipation." Then time is given for writing the answer in the workbooks. Then one of the member of the group reads the answer. At this time, the competing group, together with the teacher is the expert. Briefing - 3 min, the division into groups of 2 minutes, preparation time - 10 minutes, the performance of groups for 10 minutes (30 min). Dispensary observation of patients with the syndrome of diarrhea. Clinical examination of the patient: 1) Diarrhea - loose stools from 2-3 to 20-30 times or more a day. 2) Liquid stools with mucus or blood mixed with tissue detritus. 3) Abdominal pain - constant, aching, cramping 4) Weight Loss 5) Fever 6) Pale skin color - a sign of anemia 7) Extraintestinal manifestations - swelling and pain in joints, conjunctivitis, allergic skin rash, stomatitis, etc. Collect history: • onset of the disease • duration of the disease • received treatment, the types of drugs • the effect of treatment • the frequency of exacerbations Laboratory investigations: • full blood and urine tests • biochemical analysis of blood • coagulogram • scatological study • culture of feces for dysbiosis Conduction of instrumental methods of research: • Ultrasonography of the abdomen • EGDFS • rectoscopy • irrigography • colonofibroscopy The tactics of the doctor depends on the form and degree of activity of inflammatory and ulcerative process in the colon. - In light course and the minimum degree of activity of inflammation outpatient treatment is indicated . - In moderate and severe forms , with moderate or maximum activity of inflammation, patients are hospitalized in specialized institutions. - When the manifestation of intra-abdominal complications of ulcerative colitis as perforation, toxic dilatation, including profuse intestinal bleeding conducted emergency hospitalization in a specialized institution or a surgical hospital. Practical skills on Diarrhea syndrome A digital examination of rectum. Goal: Diagnosis of diseases of the rectum andperianal area. № Action not fulfilled (0 points) Fully correctly executed points) 1 to put on gloves 5 2 The general approach to the patient. The patient's position knee- elbow, on the side, or on the back at the gynecological chair 20 3 Description of external examination of the anus there are no space-occupying lesions, fistulous opening, and fissures. T. Etc. 20 4 Wearing a glove lubricated with Vaseline of second finger, and carefully insert into the anal canal 20 5 Sequentially examine the entire circumference of the rectum, noting the presence of pain, tumor formation, state of the external sphincter, prostate or uterus with appendages. 25 6 After manipulation inspect finger for abnormal discharge (pus, blood, mucus). 10 total 0 and (20 100 Sigmoidoscopy Indications: Disorders of the the rectum and intestine, and various inflammatory diseases and tumors of the colon and rectum, paraproctium. Required tools: proctoscope, transformer, glycerin or vaseline. The patient's position knee-elbow. Student task: Explain indications, necessary instruments, training methods and techniques of production of sigmoidoscopy. Tell semiotics of diseases and possibilities for additional research. Information for trainer :Evaluate the knowledge and skills of students through the steps separately. № Steps Not Fully, correctly fulfilled executed (0 points) (10 points) 1. Prepare the patient with siphon enema or with administration 0 of-fortransa before the examination. 10 2. Proctoscope is lubricated with glycerine or vaseline. 0 10 3. End of the tube with an obturator carried through the anal 0 canal to a depth of 4-5 cm and obturator removed. 10 4. Move forward the tubus to a depth of 10 - 12 cm under eye 0 control . 10 5. If the walls of the rectum are collapsed inflate with ballon 0 the rectum ( peripheral end of the ballon should be closed )adn gradually promote proctoscope in the proximal direction 10 6. You should not force the tube move, if it rests on the mucous 0 membrane – the latter may get damaged . The physician must see the lumen of colon. 10 7. Mucosa of the colon in catarrhal proctosigmoiditis dark red 0 and stagnant, swollen, covered with mucus; If purulent catarrhal proctosigmoiditis there are focal accumulations of pus on the mucous membrane; In hemorrhagic proctosigmoiditis there are diffuse redness with hemorrhage , mucus and blood in the lumen, contact bleeding. In ulcerative proctosigmoiditis ulcers with irregular and saped edges detected with fibrinous coating on the bottom. 10 8. In ulcerative polypoid proctosigmoiditis polypous-islets are 0 revealed between normal mucosa . Muco-purulent mass of blood in the lumen . 10 9. In Crohn's disease polypoid bulging over mucosa in the form 0 of “cobblestones” are detected. Total points Recommended main literature 1. Каримов Ш.И. Хирургик касалликлар. Т. 2004 2. Каримов Ш.И. Хирургические болезни Т.2004 г. 0 3. Наврузов С.Н. Хирургические болезни Т.2004 4. Кузин М.И. с соавт. Хирургические болезни М.1987 5. Р.Кондена и Л.Найхуса. Клиническая хирургия. М.1998 6. Орипов У.О.,Каримов Ш.И. Қорин бўшлиғи аъзоларининг ўткир ошиғич жаррохлиги. Т.1991 7. Наврузов С.Н., Наврузов Б.С. Неспецифический язвенный колит. Т.2008 8. Наврузов С.Н., Наврузов Б.С. Болезнь Крона. Ташкент 2009, С.351 9. Федоров В.Д., Дульцев Ю.В. Проктология. М. 1984. 10. Рывкин В.Л., Бронштейн А.С., Файн С.Н. Руководство по колопроктологии М. 2003 С.-123-150. Additional literature: 1. Абдужаббаров С.Б. К тактике консервативного лечения НЯК// «Актуальные вопросы заболеваний толстой кишки» Матер. Респ. науч. конф. –Ташкент, 1998. –С. 9-10. 2. Балтайтис Ю.В. Неспецифический язвенный колит. – Киев: Здоровье, 1986. -189 3. Наврузов С.Н.Наврузов Б.С. Неспецифический язвенный колит Т.2008 4. Наврузов С.Н.Наврузов Б.С. Болезнь Крона Т.2009 5. Рывкин В.Л., Бронштейн А.С., Файн С.Н. Руководство по колопроктологии М. 2003 С.-123-150. 6. Савельев В.С. Руководство по неотложной хирургии органов брюшной полости. Триада – М.2004 7. Клинические рекомендации для практических врачей, основанные на доказательной медицине. М. 2002. 8. Брискин Б.С., Верткин А.Л., Вовк Е.И. и др. Догоспитальная помощь при хирургических заболеваниях органов брюшной полости. Лечащий врач. №6, 2002, стр. 72-77. 9. Дж. Мерте. Справочник врача общей практики. М. 1998. 10. 2000 касаллик Адан Хгача УАШ шифокорлари учун қўлланма. М.2000. 11. Ситуационные задачи. 12. Стандартные протоколы. 13. Тестовые вопросы 14. Алгоритм диагностики и лечения заболеваний хирургического профиля. Ташкент. 2003.г. Под ред. Акад. Каримов Ш.И. 15. Rumessen J. Ultrastructure of intesnitial ceelles of Cajal at the colonic submuscular border in patientis with ulserative colitis. Gastroenterology 1996 111, 6: 1447-55.