Running head: DISCHARGE PLANNING PROJECT
Discharge Planning Project
Ivan Kirk II
19 June 2015
University of South Florida
DC PLANNING PROJECT
Kirk
2
During my time on the transplant unit at Tampa General hospital, I had the opportunity to
observe the discharge process of a patient I assisted in caring for. The patient was a 44 year-old
female that was admitted for a seven-pound weight gain within one week. She had a history of a
heart transplant in February of 2013. Her other pertinent medical history included hypertension,
glaucoma, hypertrophic lupus erythematosus, and chronic kidney disease. Upon her admission,
this patient was assessed to exhibit shortness of breath upon exertion, diminished lung sounds to
bilateral bases, and moderate (+3) edema to bilateral lower extremities.
The physician’s note stated the discharge diagnosis was renal failure. The patient was found to
have a decreased glomerular filtration rate (55 mL/min). With this decrease in renal function,
the associated weight gain and decreased respiratory capacity are expected due to the
accumulation of fluid volume (Huether, 2014). When asked to describe the reason for her
admission, the patient stated, “My kidneys are not working as well as they should and that’s what
caused me to gain weight.” Teaching specific to the management of this disease includes
nutritional management, knowledge of signs and symptoms of acute renal failure. Nutritional
management encompasses the modified diet necessary to optimize and preserve the function of
the kidneys (Huether, 2014). However, due to the significant heart health history of this patient,
the options for nutrition are severely limited. Currently there are no core measures associated
with acute renal failure.
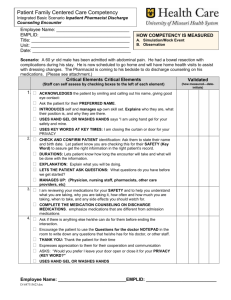
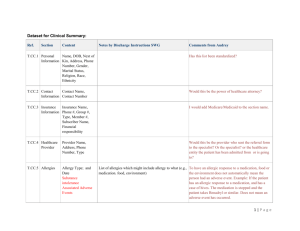
A reconciled list of medications was completed and given to the patient during the process of her
discharge. This list included the last dose she received, the time of the next scheduled dose, and
how many refills that were associated with this discharge prescription. The patient was able to
DC PLANNING PROJECT
Kirk
3
verbalize understanding of the indications and significant side effects of all her provided
medication. It was noted that while no new medications were being added, some dosages of
previously prescribed were adjusted. However, were the patient to have been unfamiliar with her
medications, I would educate her on the intended use, how the medication works, and side
effects to watch for. For example, the patient is prescribed Valcyte (valganciclovir) as an antirejection medication. This med is an anti-viral that prevents infection. However, this medication
is particularly harsh on the kidneys (Adams, 2014)
The patient lives with her husband that is extremely involved in her care and provides an ideal
living situation for this patient. As they are both retired, transportation to and from any
destination is available. Additionally, the patient’s children visit on regular bi-weekly intervals
to assist wherever necessary. Financially, the cost of the medications is a “manageable burden”
as described by the husband. The husband explained the Medicare “donut hole” concept in depth
as it pertained to their finances. Due to the high cost of the medications, they did not spend
much time in the “hole” of the donut.
Presently, there are no additional resources necessary within the home of this patient. She
displays no hindrance or complication while performing activities of daily living. A follow-up
appointment was scheduled with her primary care physician within one week of the discharge
date. No consultation with a specialist is currently required at this point in time. However, as the
chronic kidney disease continues to progress I anticipate a comprehensive plan to be developed
by nephrology, cardiology, and the primary care physician. Also included in the discharge plan
are nutrition therapy, social work, and physical therapy. As stated above, the patient must make
DC PLANNING PROJECT
Kirk
4
some adjustments to her dietary intake for her kidney and heart to operate at an optimal level.
Social work may be able to identify additional resources to decrease the financial burden of
medications and other health care associated costs. Also, physical therapy can assist with
teaching exercises to maintain and possibly increase the patient’s physical strength, balance, and
coordination.
The most important considerations to prevent readmission for this patient are to continue
following her medication regimen, adjust her nutritional intake as recommended, and monitor
her health for any signs of complications. These complications include but are not limited to
rapid weight loss or gain, fatigue, confusion, decrease or increase in urinary frequency an
amount, swelling/edema, and malodorous urine.
DC PLANNING PROJECT
Kirk
References
Huether, S.E., & McCance, K.L. (2014). Understanding Pathophysiology. Salt Lake City,
UT: Elsevier.
Osborn, K.S., Wraa, C.E., Watson, A.,& Holleran, R.S. (2014). Medical-Surgical
Nursing:Preparation for Practice (2nd ed.) Upper Saddle River, NJ. :Pearson
Prentice Hall.
Patrick Adams, Michael, Holland, Leland, & Urban, Carol. (2014). Pharmacology for
Nurses: A Pathophysiological Approach (4th ed.) Upper Saddle River, NJ:
Pearson Prentice Hall.
5
DC PLANNING PROJECT
Kirk
6





![Cheat Sheet []](http://s3.studylib.net/store/data/007481385_1-17686b575c10c412131e43e77ac5fd99-300x300.png)