Dataset for Clinical Summary
advertisement
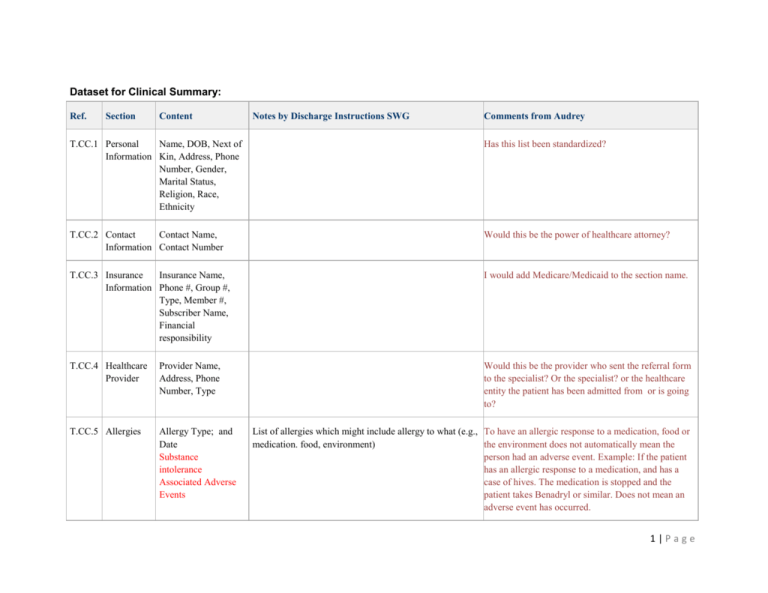
Dataset for Clinical Summary: Ref. Section Content Notes by Discharge Instructions SWG Comments from Audrey T.CC.1 Personal Name, DOB, Next of Information Kin, Address, Phone Number, Gender, Marital Status, Religion, Race, Ethnicity Has this list been standardized? T.CC.2 Contact Contact Name, Information Contact Number Would this be the power of healthcare attorney? T.CC.3 Insurance Insurance Name, Information Phone #, Group #, Type, Member #, Subscriber Name, Financial responsibility I would add Medicare/Medicaid to the section name. T.CC.4 Healthcare Provider Provider Name, Address, Phone Number, Type Would this be the provider who sent the referral form to the specialist? Or the specialist? or the healthcare entity the patient has been admitted from or is going to? T.CC.5 Allergies Allergy Type; and Date Substance intolerance Associated Adverse Events List of allergies which might include allergy to what (e.g., To have an allergic response to a medication, food or medication. food, environment) the environment does not automatically mean the person had an adverse event. Example: If the patient has an allergic response to a medication, and has a case of hives. The medication is stopped and the patient takes Benadryl or similar. Does not mean an adverse event has occurred. 1|Page T.CC.5 Other Adverse Reactions T.CC.6 Allergy Type; and Date Substance intolerance Associated Adverse Events Problem List Active Problems (R/N)/Chief Complaint (overriding problem at the time of discharge) - chronic illness and congenital problems Yes/No/Unknown, and if Yes or Unknown how does it affect care. Other history that guide care. Patient supplied information about reaction Current Diseases & Conditions monitored for the patient and status If a patient is allergic to latex or tape, this is a product allergy. An adverse event would be if the patient was listed as having a latex allergy and latex was used in the care of the patient and the patient had a skin reaction. This is an adverse event because it could have been prevented. In some places these events are called “never events” because they are preventable. List of problems/complaints (what was diagnosis, complaint and/or descriptor of problem/complaints, symptoms). Is a list, of diagnosis, complaints some of these may have been resolved and some are active. How do these problems/complaints impact interventions, orders or instructions. Discharge instructions usually are for the encounter just ending. Patient's perception or description of problems/complaints Is usually in notes or history. Not part of a formal problem list. T.CC.7 History of Past Illness Diseases & Conditions Patient has suffered in the past May be a list with dates onset and/or resolution T.CC.8 Chief Complaint (see change in T.CC.6 Problem List) Description of Patient's Complaint (narrative) If not listed in the problem list. T.CC.9 Reason for Transfer Reason Patient is being referred May come from Utilization Review (UR) or Medicare rules, insurance or HMO rules or the patient may be well. T.CC.10 History of Present Illness Sequence of events that occurred to change the state of the patient’s health proceeding patient's disease/condition 2|Page T.CC.11 List of Surgeries List of types of surgeries and dates T.CC.12 Hospital Admission Diagnosis List of Hospital Diagnosis and dates Hosp Adm diagnosis is different for list of hosp diagnosis and dates. This should be the current encounter adm date T.CC.13 Discharge Diagnosis Conditions/Diseases identified during hospital stay and dates Current encounter list only T.CC.14 Medications List of Current Medication Names ; date, route, dose, frequency list of prescribed medications or other medications. Should be the reconciled list (which should have been done on admission) If to be reconciled then list needs to be inclusive of self administered medications (herbals, over the counter) See notes on medication reconciliation regarding expectations such as discontinued medications from inpatient if not included in discharge summary 3|Page T.CC.15 Admission Medications History List of historical medication names, dose, route, frequency, date patient has taken prior T.CC.16 Hospital Discharge Medications Medications names, doses, frequency, route ordered for the patient for after discharge T.CC.17 Medications Administered Medications administered to patient during the course of an encounter; name, dose, route, frequency T.CC.18 Advanced Directives A summary of patient's expectations for care T.CC.19 Pregnancy Pregnant, Yes/NO T.CC.20 Immunizations Immunizations name, dose, route, date administered to the patient T.CC.21 Physical Examination Physical Findings of the Patient; VS, Biometrics, Review of Systems T.CC.22 Vital Signs Vital Signs (R/N) including Pain Scale Assessment, Smoking Status Patient's Vital Signs ; Heart rate, Instructions regarding the capture of vital signs at points along Resp Rate, Pulse Ox, Temp, B/P, the care plan and any special instructions regarding how to Pain capture T.CC.23 Review of Systems Functions of various body systems; Neuro, Derm, GI, GU, Cardiac, Pulmonary, MS, Repro, Nervous, Endocrine Yes/No Yes/No if POLST form returned Where is last known version/original is located Going forward how the "state" and how it affects care Comprehensive list of immunizations (have - patient reported, got, need):* list of immunizations necessary to get after discharge.* list of education or information about immunizations they received while hospitalization 4|Page T.CC.24 Hospital Course Sequence of (name, diagnosis associated with) events and dates from admission to discharge of hospital stay T.CC.25 Diagnostic Results Results and dates of Diagnostic Procedures T.CC.26 Assessment and Plan Assessment of patients conditions and expectations/goals of care T.CC.27 Plan of Care Plan of Treatment/Treatment Plan/Care Plan (R/N) - Covers the considerations that encompass a range of scopes and/or timeframe (could be a description of a single encounter or across multiple encounters Proposed interventions and procedures for patient Corresponding results to the scheduled procedures and interventions. T.CC.28 Family History Dates with Disease Suffered, Age of Death, other genetic information T.CC.29 Social History Patient's beliefs, home life, social/risky habits, family life, work history T.CC.30 Encounters Current and historical encounters; dates T.CC.31 Medical Equipment Medical Devices (C/N) - includes assistive devices and is related to functional status Implanted and External Medical Devices; Dates Goals. Active interventions and orders (short term direct instructions - in the long run as validated by the patient and those contributed by the patient/caregiver). Yes/No - has the discharge instruction been reviewed with the patient. Yes/No - has the discharge instruction been accepted by the patient, if no then how addressed List of devices and where the device is to be secured/prescribed/embedded. Duration of medical devices. History of devices for this patient. 5|Page T.CC.32 Preoperative Diagnosis Diagnosis ( Date) assigned to patient prior to surgery T.CC.33 Postoperative Diagnosis Diagnosis ( Date) assigned to patient after surgery T.CC.34 Surgery Description Particulars of Surgery (narrative) (images) T.CC.35 Surgical Operation Note Findings Clinically significant observations found during surgery T.CC.36 Complications Section Known risks or unidentified problems T.CC.37 Operative Note Surgical Procedure Date and Description of Procedure Performed ADDED Education Patient education provided or needed. To included classes, educational sessions, printed materials. ADDED Electronic Links How to get to future results, summaries, etc. Updated PHR ADDED Facility Checklist List of facility dependent items (e.g., pain scale at discharge, last ECG, etc. 6|Page ADDED Diet/Diet Restrictions (R/N Diet: - All instructions that describe the expected diet. Restrictions: - List of limitations being placed on the diet ADDED Fluids Management (C/N) Fluids: - All instructions that describe the expected fluids and method of administration. Restrictions: - List of limitations being placed on fluids ADDED Functional Status (O/N) - Might be Smoking SHOULD be present when any assessments of functional status are performed on the patien Baseline, current and desired:* Functional status* End state/goal expressed/Projected change in functional status (will relate to the goals identified) ADDED Procedures and Interventions (C/N) Scheduled procedures and interventions, such as labs, etc. (procedure/intervention, schedule, etc. 7|Page