Discharge Planning Project
advertisement

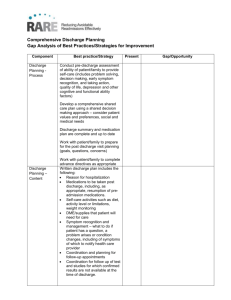
Running head: DISCHARGE PLANNING PROJECT Discharge Planning Project Johan Diaz University of South Florida College of Nursing NUR4216L November 19, 2013 1 DISCHARGE PLANNING PROJECT 2 Discharge Planning Project The 59-year-old Hispanic female with a history of hypertension, hypothyroidism and chronic renal insufficiency presented to the Emergency Department (ED) with epigastric pain on 09/30/13. The patient stated that the onset of the epigastric pain was “around 4 p.m.” on the day of the admission. The patients characterized the pain as constant and sharp. The patient denied radiating pain, nausea/vomiting, and diarrhea. An EKG revealed sinus bradycardia (54 bpm) with no evidence of acute ischemic changes. Abdominal ultrasound revealed cholelithiasis. BUN was 64, and creatinine was 4.28, indicating renal failure. Patient was kept NPO until laparoscopic cholecystectomy was completed. The patient is now on a renal diet. Discharge diagnosis The patient understands that she was hospitalized because of the pain related to cholelithiasis (gallstones). The patient also understands that during the laparoscopic cholecystectomy her gallbladder was surgically removed. Associated Core Measures The associated core measures for this patient were all met and are provided by the Joint Commission in the table below. (The Joint Commission, 2012) 3 DISCHARGE PLANNING PROJECT Medications There is a reconciled list of the patient’s medications. There are no new prescriptions or refills needed for this patient. The discharge plan includes information on when the last dose of medication was given and when the next dose is due. The only medications that this patient will continue at home until follow-up will be her clonidine (0.2mg, TD patch, 1xweek) and her synthroid (30 mcg, PO, 1xdaily). The patient verbalized understanding of all of her medications, including the indications and side effects. Sweating, headache, abdominal cramps, insomnia, and irritability are the common side effects for synthroid. Drowsiness, dry mouth, dizziness, nausea/vomiting are the common side effects for clonidine. The patient understands that she must remove the patch before placing a new one and alternate placement locations. The patient understands that she must take her synthroid 30 minutes before breakfast. Home assessment The patient lives in a one story home with her husband of 32 years. The patients living situation has been assessed and determined to be safe. The patient’s husband and children are reliable mechanisms for self-care upon discharge including the following: transportation to get medications, food, follow-up appointments, etc. The patient verbalized understanding of not driving until she is no longer taking her pain medication. The patient has insurance and has no financial concerns regarding medications or access to follow-up appointments at this time. Follow up There is no need for home health services or durable medical equipment at the home. A follow up appointment will need to be scheduled with the primary care provider and the surgeon within a month of discharge. The patient will also need to follow up with her nephrologist to determine the plan of care for her chronic renal insufficiency. Physical therapy should be 4 DISCHARGE PLANNING PROJECT included in the discharge planning process. This will allow the patient to prevent complications from surgery by increasing mobility. Summary Patient education is an essential part of preventing readmission for this patient. Not only education about her admitting diagnosis but also about her pre-existing co-morbidities. The nutritional consult was completed for the patient before discharge. The new diet will be part of the treatment plan. The patient will be taught how to care for her incision site. The patient will be educated on the importance of maintaining the follow-up appointments. The patient will be educated on the signs/symptoms of infection (especially at the incision site) and when it is appropriate to call the provider. 5 DISCHARGE PLANNING PROJECT References The Joint Commission. (2012). Surgical Care Improvement Project. Retrieved from http://www.jointcommission.org/core_measure_sets.aspx