Scenario for Inpatient Pharmacist Discharge Counseling Encounter
advertisement

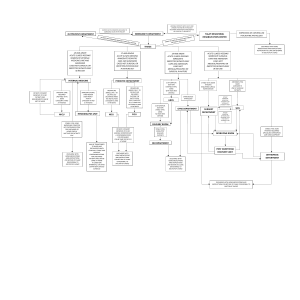
Patient Family Centered Care Competency Integrated Basic Scenario Inpatient Pharmacist Discharge Counseling Encounter Employee Name: _____________________________ EMPLID: ____________________________________ Title: _______________________________________ Unit: _______________________________________ Date: _______________________________________ HOW COMPETENCY IS MEASURED A. Simulation/Mock Event B. Observation Scenario: A 60 yr old male has been admitted with abdominal pain. He had a bowel resection with complications during his stay. He is now scheduled to go home and will have home health visits to assist with dressing changes. The Pharmacist is coming to his bedside to do discharge counseling on his medications. (Please see attachment.) Critical Elements Critical Elements Validated (Staff can self assess by checking boxes to the left of each element) (how measured—dateinitials) 1. 2 ACKNOWLEDGES the patient by smiling and calling out his name, giving good . eye contact: 2. 3. 4. Ask the patient for their PREFERRED NAME. INTRODUCES self and manages up own skill set. Explains who they are, what their position is, and why they are there. USES HAND GEL OR WASHES HANDS says “I am using hand gel for your safety and mine. USES KEY WORDS AT KEY TIMES: I am closing the curtain or door for your PRIVACY CHECK AND CONFIRM PATIENT identification: Ask them to state their name and birth date. Let patient know you are checking this for their SAFETY (Key Word) to assure get the right information in the right patient’s record. DURATIONS: Lets patient know how long the encounter will take and what will be done with the information. EXPLANATION: Explain what you will be doing. LETS THE PATIENT ASK QUESTIONS: What questions do you have before we get started? MANAGES UP: (Physician, nursing staff, pharmacists, other care providers, etc) I am reviewing your medications for your SAFETY and to help you understand what you are taking, why you are taking it, how often and how much you are taking, when to take, and any side effects you should watch for. COMPLETE THE MEDICATION COUNSELING ON DISCHARGE MEDICATIONS. emphasize medications that are different from admission medications Ask if there is anything else he/she can do for them before ending the interaction. Encourage the patient to use the Questions for the doctor NOTEPAD in the room to write down any questions that he/she has for his doctor, or other staff. THANK YOU: Thank the patient for their time Expresses appreciation to them for their cooperation and communication ASKS: “Would you prefer I leave your door open or close it for your PRIVACY (KEY WORD?” USES HAND GEL OR WASHES HANDS Employee Name: ___________________________EMPLID: ____________________________ D:\687315623.doc _______ COMPETENCY DEMONSTRATED _______ ACTION PLAN REQUIRED VALIDATOR_________________________________________________ DATE___________________________ VALIDATOR_________________________________________________ DATE___________________________ VALIDATOR_________________________________________________ DATE___________________________ VALIDATOR_________________________________________________ DATE___________________________ Comments: D:\687315623.doc Additional Information for the Pharmacist Scenario Allergies: sulfa (itchy rash) Weight: 110 kg HbA1C on admission: 10.2% SCr on admission 1.1 mg/dL, 1.3 mg/dL on day of discharge PMH per medical record: DM Type 2, onset 15 years ago – managed by primary care practitioner Medications Patient was taking at home prior to admission: Lisinopril 20 mg po daily aspirin 325 mg po daily ginko biloba, unknown dose insulin 70/30, 40 units subcue with breakfast and 30 units subcue with supper Medications on Discharge Lisinopril 20 mg, 1 tab po daily aspirin 325 mg, 1 tab po daily Insulin glargine 35 units subcue qhs Insulin aspart 15 units tid with meals Amoxicillin/clavulanic acid 875mg/125mg, 1 tablet q12hrs x 10 days Oxycodone / acetaminophen 5/325 mg, 1-2 tablets q 6 hours prn pain Docusate sodium 100 mg, 1 tablet po bid until no longer taking pain pills Bisacodyl 10 mg, 1 tablet by mouth daily until no longer taking pain pills According to Resident Physician’s Discharge Orders and Instructions: follow up with general surgery clinic in two weeks scheduled for diabetes education class AND endocrine clinic appointment in three weeks D:\687315623.doc