Male Reproductive System
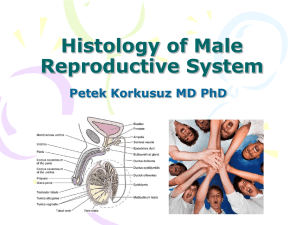
advertisement

Male Reproductive System Consists of 2 testes and penis, duct system between testes and penis, accessory sexual structures that include glands that contribute fluid secretions to semen upon ejaculation. Testis. o Functions as both exocrine gland that produces male germ cells (spermatozoa) and endocrine gland that produces testosterone. o Epididymis – consists of ductus epididymis (canal attached posteriolaterally to testis). Both structures consist of packed tubules that differ morphologically and functionally from each other. Purpose of tubules is to transport spermatozoa that have been produced in seminiferous tubules of testis. o Tunica albuginea of testis – dense connective tissue capsule that surrounds testis. Capsule covered by serous membrane – visceral layer of tunica vaginalis that forms a pouch around testis that is incomplete posteriorly. Parietal layer of tunica vaginalis (squamous epithelium) lines internal surface of scrotum. o Posterior surface of testis attached to wall of scrotum. o Endocrine interstitial cells of Leydig occur in angular interstitial spaces between profiles of seminiferous tubules, along with macrophages and fibroblasts – ovoid pale staining cells with frothy cytoplasm; has lipid droplets. o Semineferous tubules lined with complex stratified epithelium – germinal/seminiferous epithelium, and ensheathed in layer of connective tissue. Epithelium of tubules is engaged in progressive spermatogenic proliferation and differentiation that occurs in stages over 64 days. o Sertoli cells (sustentacular cells) – solitary/tall cells, radially oriented with their bases on basement membrane of tubule and apical cytoplasm extending to lumen. Nucleus lies variable distance from base of cell – large, oval, irregularly indented, pale staining, and radially oriented. o Spermatogonia – in contact with tubules’ basement membrane with nuclei near basement membrane and circumferentially disposed. Type A dense – diploid stem cells of tubule that give rise to type A pale and type A dense offspring. Type A pale divide and differentiate into type B spermatogonia. Type B will undergo several mitotic divisions and give rise to primary spermatocytes that will enter myosis. o Spermatocytes – largest germ cells that undergo 2 meiotic divisions. Nuclei are prominent and typically exhibit chromatin organizing into chromosomes as they enter final stages of meiosis I. o Spermatids – haploid cells that are products of final meiotic division of spermatocytes. No longer divide but will differentiate into mature spermatozoa. Spermiogenesis – process whereby spermatid undergoes morphological transformation to acquire final shape of spermatozoa. Typically located near lumen. Early spermatids – nuclei are small and densely stained. Late spermatids – radially elongated dark staining nuclei and flagella oriented towards lumen and still embedded in apical cytoplasm of Sertoli cells. o Spermatozoa – cells with small elongated head (acrosome + nucleus), no visible cytoplasm, long/slender tail that is mostly flagellum. Late spermatid becomes spermatozoon after sperm head is actively extruded from Sertoli cell, leaving much of residual spermatid cytoplasm either in apical cytoplasm of Sertoli cell where it is endocytosed and degraded, or as residual bodies, which are shed into lumen of seminiferous tubules. o Mediastinum testis – ducts, blood vessels, lymphatics, and nerves enter or leave tests through it. Radiating out from middle and sides of mediastinum are incomplete connective tissue septa (septula tests) that subdivide testis into about 250 lobules. Each long coiled loop or tube of seminiferous tubule is continuous with rete testis via short intervening tubulus rectus that is lined completely by Sertoli cells with no germ cells within epithelium. Rete testis consists of series of irregular anastomosing channels, forming network of interconnected chambers, embedded in well-vascularized mediastinum – simple cuboidal epithelium lines these channels, and there are many lymphatic vessels around rete testis. Ducts. o About 12-20 efferent ductules perforate tunica albuginea and pass from testis to epididymis, carrying spermatozoa from rete testes – they become very convoluted and collect in head of epididymis. Individual tubules are embedded in connective tissue and thin layer of circularly arranged smooth muscle surrounds each profile – epithelium is simple columnar and lumen appears scalloped due to presence of 2 types of cells: tall/columnar ciliated cells (cilia beating toward ductus epididymis) and shorter non-ciliated cells that actively absorb some of fluid secreted by Sertoli cells. Cilia assist in movement of sperm. o Ductus epididymis – occupies body and tail of epididymis. Lumen smooth and regular, with thick and uniform epithelium (pseudostratified with abundant/tall columan principal cells that reach lumen and have long nonmotile stereocilia). There are also rounded basal cells scattered along basement membrane – stem cells. Stereocilia perform absorptive function. Secretions from epidydimal cells add glycoprotein coat to spermatozoa that’s essential for maturation of sperm but is later removed by contact with female repro tract. Epididymal duct surrounded by layer of smooth muscle and embedded in fibrous connective tissue – muscle layer is thin over most of length but thickens markedly near ductus deferens. o Ductus deferens – pseudostratified epithelium but shorter stereocilia. Mucosa thrown into 4-6 longitudinal folds, giving lumen a stellate profile in transverse section. Epithelium not as tall as of ductus epididymis, with thin/dense lamina propria that contains many elastic fibers. Muscular coat is very thick and ordered into 3 layers (inner longitudinal, middle circular, outer longitudinal). Travels toward periotenal cavity in spermatic cord – bilateral bundle of vessels, nerves, ducts associated with testis and connects with abdominal structures. Has cremaster muscle – raises testicle. Blood vessels are testicular artery (tends to be coiled) and extensive pampiniform plexus of veins (unusually thick walls; function is to cool arterial blood as it approaches testis). After entering abdominal cavity, ductus deferens passes anterior to urinary bladder, then expands to form ampulla of ductus deferens (storage section for spermatozoa) on posterior surface of urinary bladder. o Tube continues as ejaculatory duct that travels into body of prostate gland. o Within prostate gland, right and left ejaculatory ducts flow into prostatic urethra. Seminal vesicle – as ductus deferens passes around urinary bladder, it’s joined by seminal vesicle. o Secretes nutrients into seminal fluid. o Has relatively large lumen in most of profiles of coiled seminal vesicle. o Highly complex honeycomb arrangement of branching chambers such that when tube is sectioned tangential to lumen, epithelial cells appear to be isolated secretory acini. o Prominent muscular wall arranged into inner circular and outer longitudinal layers that contract during ejaculation to expel seminal fluid. Prostate gland – surrounds beginning of male urethra as it leaves urinary bladder. o Tuboloalveolar compound gland with little evidence of ducts among secretory elements. o Secretory nature of epithelium – varies from simple cuboidal to simple columnar to pseudostratified. o Lumens of secretory elements expanded by accumulated secretory product with folds of epithelium allowing further expansion. o Prostatic concretions – calcified glycoprotein and coagulated prostatic secretion in umen of peripherally situated glandular acini. o Fibromuscular stroma, dense with collagen and irregularly arranged smooth muscle is continuous with thin/strong capsule. Penis. o Corpora cavernosa – separated by incomplete midline septum penis (present in proximal but not distal portion of penis). Composed of true erectile tissue that increases in size by filling with blood, enabling penis to change from flaccid to rigid state. Spaces are lined with typical endothelium and bordered by trabecular walls of connective tissue and smooth muscle. o Corpus spongiosum – contains penile urethra located in its center as narrow epithelial lined slit. Tunica albuginea is thin and includes many elastic fibers. Trabeculae are thinner and more elastic than in corpora cavernosa. Penile urethra has folded mucosa in relaxed state – epithelium is variable, being transitional near bladder, pseudostratified or stratified columnar throughout most of its length, and stratified squamous at end near meatus. Periurethral mucous glands of Littré may appear in lamina propria near or outside urethra – produce mucus and lubricate lumen of penile urethra. o Tunica albuginea of penis – surrounds each cavernous body. o Penis enveloped by thin skin with tall dermal papillae. Testes – spermatozoa produced in testes enter urethra via epididymis, ductus deferens, ejaculatory ducts. Seminal vesicles – secretions enter urethra via ejaculatory ducts, which are continuations of ductus deferens within prostate. Prostate gland – around 25 ducts empty into urethra. Bulbourethral gland (Cowper’s) – each with single opening into urethra. Testis – primary reproductive organs (gonads) in male. o Suspended within scrotum (thin skin, no subcutaneous fat, dartos muscle) that creates lower temperature to facilitate spermatogenesis. o Cremaster – functions to raise or lower testis within scrotal sac. o In embryo, development of gonads under control of testosterone – testes originate from within abdominal cavity in retroperitoneal space. Gubernaculum guides descent of testes through inguinal canal into scrotum. Remnant of embryonic connection creates weak spot that can lead to inguinal hernia. o Each testis encapsulated by tunica albuginea of testis, which thickens at posterior margin of testis and projects testis as mediastinum testis, with blood vessesl/lymphaticsnerves/ducts. o Radiating from mediastinum to capsule, connective tissue gives rise to delicate septa that divide testis into lobules. o Seminiferous tubules lined with seminiferous (germinal) epithelium consisting of cells producing spermatozoa and testicular fluid: Sertoli cells and spermatogenic cells. o Spaces between seminiferous tubules are occupied by highly vascular connective tissue containing fibroblasts, macrophages, Leydig cells (round nuclei, cytoplasm with lipid droplets; secrete testosterone to blood stream). Spermatogenesis – entire process that begins with primitive germ cell (spermatogonium), continues through multiple stages of cell division and ends with production of male gametes (spermatids). o Spermatocytogenesis – includes all mitotic divisions of spermatogonia, eventually producing primary spermatocytes. o Meiosis – haploid spermatids are generated from primary spermatocytes. o Spermiogenesis – morphological transformation of spermatids into spermatozoa. o Spermiation – release of spermatozoa from luminal epithelium of seminiferous tubules. Spermatogenesis. o Sertoli cells – supporting cells of seminiferous tubules. Provide support, protection, nutrition, developmental regulation for spermatozoa. Phagocytose excess spermatid cytoplasm. Continuously secrete fluid that’s used for sperm transport in proximal genital ducts. Secrete androgen binding protein (concentrates testosterone in cells lining reproductive tract), inhibin (inhibits FSH production by pituitary). Produce anti-mullerian hormone during fetal development, inhibiting development of female reproductive structures. Form blood-testis barrier that protects haploid gametes from blood-borne noxious agents and contact with immune system. o Begins with activation of single peripherally located restine Type A dense spermatogonium (reserve cells that may enter cell cycle and divide to produce Type A dense and Type A pale). o Type A pale induced by testosterone to proliferate and differentiate dividing into 2 Type B (progenitor cells). o Type B undergo 4 additional mitotic divisions, final one giving rise to primary spermatocytes, that will then undergo 1st meiotic division, resulting in secondary spermatocytes, which divides again to produce haploid cells that no longer divide but being morphological differentiation, at which point they’re termed spermatids. o Seminiferous epithelium divided into 2 compartments – blood-testis barrier formed by connection of neighboring Sertoli cells with each other via tight and adhering junctions – primary spermatocytes pass through these junctions from basal compartment to adluminal side, as they enter leptotene stage of meiotic prophase. o Primary spermatocytes reside exclusively in basal compartment and secondary spermatocytes in adluminal compartment. o Initial Type A divide and produce separate daughter cells and progenitor Type B and all subsequent divisions stay connected by intercellular cytoplasmic bridges – spermatozoa can be considered to be isolated cells only after they’re separated from residual bodies. Spermiogenesis – final stage of production of germ cells with no cell division. o Haploid spermatids begin as small spherical cells with small dense nuclei (early spermatids) and gradually mature into pointed cells with flagella (late spermatids) that are embedded in apical cytoplasm of Sertoli cells. o First recognizable change is formation of acrosome (contains hydrolytic enzymes that dissociate cells of corona radiate and digest zona pellucida that surround oocyte). o Acrosome shapes condensing nucleus into elongate form. o Cytoplasm deforms under control of specialized mictrotubule element manchette. o Further development includes flagellum synthesis, packaging of mitochondria, loss of cytoplasm in residual bodies, loss of intercellular bridges. o When complete, late spermatids released from enveloping apical cytoplasm of Sertoli cell into lumen of seminiferous tubules as mature spermatozoa – consists of pyriform head, with acrosomal cap; tail that consists of neck, middle piece with mitochondria, principal piece with 9+2 arrangement, end piece (fine filaments only). o Capacitation – glycoprotein coat acquired by spermatozoa in ductus epididymis facilitates longterm storage in male repro tract. Coat removed through contact with uterine epithelium in capacitation process. Final step in sperm maturation. Duct system – tubuli recti at end of seminiferous tubule → rete testis → ductuli efferentes → ductus epididymis → ductus deferens → ampulla → ejaculatory duct → prostatic urethra → penile urethra. o Current, produced from fluid produced in testes and absorbed further along duct, first carries sperm. o Ductili efferentes contain cilia that are important in moving sperm. o Sperm are propelled by increasingly thick layer of smooth muscle, which contracts forcibly during ejaculation. o Flagellar motor is largely reserved for movement after ejaculation. o Tubuli recti and rete testis. Seminiferous tubules connect with rete testis by straight short tubuli recti. Transition from seminiferous tubules – gradual loss of germinal elements from epithelium until only Sertoli cells line tubules; this short portion ends abruptly with simple cuboidal epithelium characteristic of rete testis (consists of series of interconnected channels within bed of highly vascular connective tissue, mediastinum testis). o Ductuli efferentes – have 2 types of epithelial cells lines (tall columnar ciliated cells and shorter cells that are absorptive in function). Lumen has characteristic scalloped outline. Creates a flow of fluid from rete testis that carries spermatozoa toward ductus epidiymis. o Ductus Epididymis and Ductus Deferens. Some of final differentiating steps in sperm development occur in ductus epididymis – lined with tall pseudostratified columnar epithelium bearing stereocilia, and macsular wall. Ductus epididymis along with connective tissue and blood vessesl forms body and tail of epididymis. Epithelium participates in elimination of any residual bodies that have accompanied spermatozoa. Cells secrete glycoproteins and other materials essential for maturation of spermatozoa. Maturing spermatozoa stored in lumen of ductus epididymis. Smooth muscle becomes thicker as epididymis followed sitally toward junction with ductus deferens. Ductus deferens – thick walled tube that is continuation of epididymis, that extends into abdominal cavity and to prostate gland. Lumen is highly folded and lined by pseudostratified epithelium with stereocilia, with principal cells not as tall or stereocilia as long as in epididymis. Has thin lamina propria. Most striking feature is 3-layered muscular coat. Ductus deferens forms part of spermatic cord, which is palpable through upper scrotum, and invested with fascia. Contains arteries and pampiniform plexus, which drain testis and epididymis. o Ampulla and Ejaculatory Duct. Before entering prostate gland, each ductus deferens dilates into ampulla – epithelium is thicker than that of distal ductus deferens and extensively folded. After seminal vesicle joins duct, duct enters prostate gland as ejaculatory duct – opens into prostatic urethra within central elevation of urethral mucosa as seminal colliculus. o Urethra – near origin, epithelium is transitional (as in bladder); prostatic urethral epithelium largely transitional; pseudostratified/stratified columnar arrangement in penile urethra. Within penis, patches of stratified squamous epithelium present. o Along course of urethra, can have occasional mucus goblet cells and glands of Littré. Seminal vesicle, prostate, bulbourethral gland. o Seminal vesicle – formed from outpouching of ductus deferens. Central large lumen is lined by meshwork of thin trabeculae that form slender primary folds that branch into secondary and tertiary folds. Muscular coat has outer longitudinal and inner circular smooth muscle. Epithelium is nonciliated pseudostratified epithelium. Secretion formed represents substantial portion of whole ejaculate and contains many substance that serve as spermatozoa-activating substances – fructose (principal energy source) and prostaglandins. o Prostate – branched tuboloalveolar glands whose ducts empty into lateral edges of prostatic urethra. Central zone occupies 25% and surrounds ejaculatory ducts; peripheral zone (70%) comprises outermost portion which is major site of prostate cancer; transitional zone surrounds prostatic urethra proximal to ejaculatory ducts which is where most BPH originates. Glandular epithelium of prostate generally appears simple columnar, but may be called pseudostratified due to presence of sparse basal cells (stem cells). Interstitial tissue is abundant and consists mainly of dense CT. Secretion is rich in proteolytic enzymes, including fibrinolysyin and acid phosphatase and citric acid. Lumens of individual glands may have prostatic concretions (corpora amylacea) – increase in number with age and present in ejaculate. Prostatic utricle – small blind outpouching of urethra. Abundant smooth muscle of seminal vesicle and prostate is innervated by sympathetic nervous system, which stimulates contractions that empty these glandular structures during ejaculation. BPH – occur in portion of gland surrounding urethra, can cause difficulty in urination/increased incidences of UTI due to incomplete voiding. Sensitive to androgens and estrogens – treatment involves antiandrogen drugs and surgical resection. Prostate cancer occurs in distal portion of glands – PSA often overproduced. Blood acid phosphatase levels can also be used to detect prostate cancer. o Bulbourethral glands (Cowper’s) – tubuloalveolar mucus glands with ducts and secretory parts of irregular form. Connected with penile urethra by ducts. Clear viscous secretion may function as lubrication, to displace urine, and/or provide basic environment in urethra, and is ejected primarily during sexual stimulation prior to ejaculation. Penis – consists principally of urethra and 3 parallel cavernous bodies. o Sebaceous glands are absent and sweat glands are sparse. o Erectile tissue consists of paired corpora cavernosa and single corpus spongiosum. o Urethra lies in center of corpus spongiosum. o Erectile tissue is sponge-like system of large number of venous spaces lined with endothelial cells and separated by trabeculae of CT and smooth muscle. o Helicine arteries – empty directly into vascular spaces. o Tunica albuginea of penis envelops corpora cavernosa. o Incomplete septum allows pressure to equalize in corpora cavernosa. o Albuginea enclosing spongiosum is thinner and contains circularly arranged smooth muscle fibers and more elastic fibers than that of paired cavernous bodies. o Penile erection controlled by parasympathetic neural input to both arterial muscle and smooth muscle in walls of erectile tissue – corpora cavernosa fill with blood through relaxation of helicine arteries and compression of veins and arteriovenous shunts via compression against surrounding tunica albuginea. o Erectile dysfunction – PDE-5 (degrades cGMP) inhibited through pharmacological intervention and prolongs action of cGMP and NO.