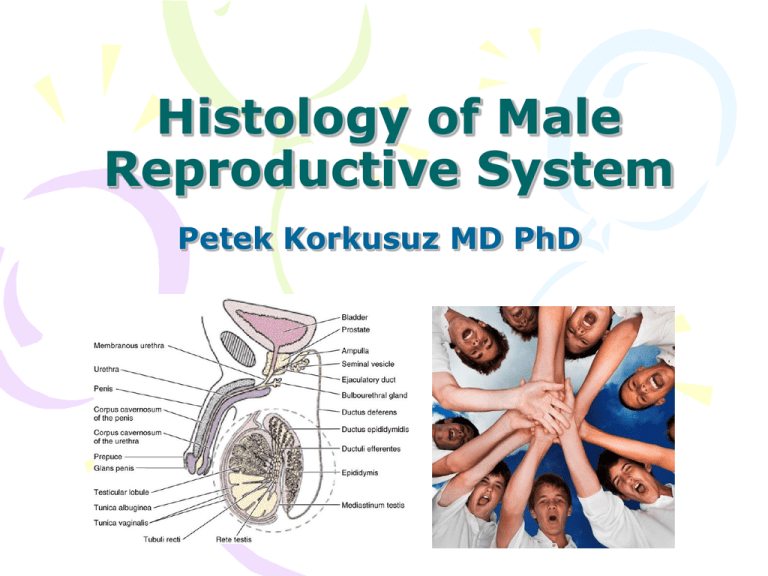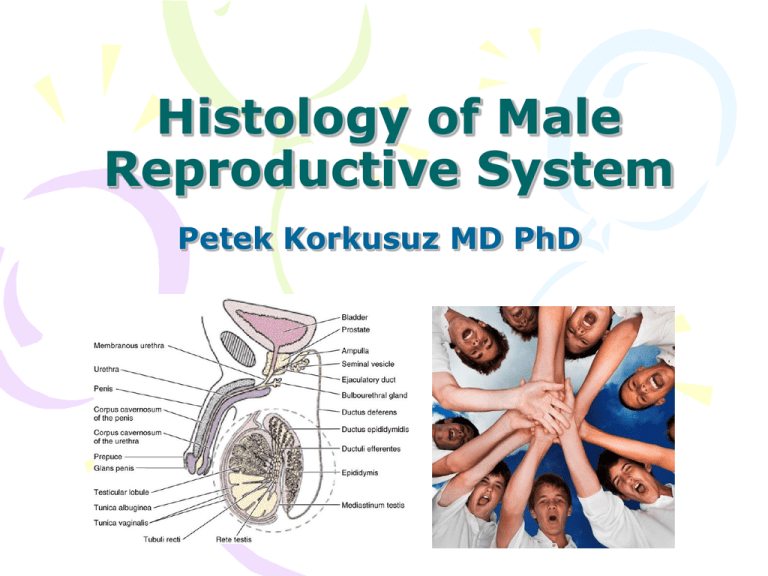
Histology of Male
Reproductive System
Petek Korkusuz MD PhD
Aim
• To learn
histological
structure and the
histophysiology of
male reproductive
organs
Learning Goals
• To learn the histology and histophysiology
of two testes
• To learn the histology and histophysiology
of the genital ducts
• To learn the histology and histophysiology
of the associated glands:
– Paired seminal vesicles
– Single prostate glands
– Bulbourethral (Cowper) glands
• To learn the histology and histophysiology
of the penis
Male Genital System
• Two testes..formation of
spermatozoa & synthesis,
release and storage of
testosterone
• Genital ducts
• Associated
glands..formation of
noncellular portion of semen
– Paired seminal
vesicles
– Single prostate
glands
– Bulbourethral
(Cowper) glands
• Penis...delivery of semen to
female reproductive system
Testes
• Paired oval organs, located
in the scrotum (approx
4x3x3cm)
• Testes develop
retroperitoneally, carry a
peritoneal outpouching
while descending in
scrotum: tunica vaginalis
• Tunica albuginea (irregular
dense connective tissue)
surrounds each testis
• Tunica vasculosa (highly
vascular loose connective
tissue) located
immediately deep to TA
forms the vascular
capsule.
Testes
• The posterior aspect of TA
is thickened to form
mediastinum testis.
• The connective tissue
septa radiate from MT to
subdivide each testis into
approx 250 pyramid
shaped lobuli testis.
• Each lobule has 1-4 blindly
ending seminiferous
tubules
• Richly vascularized and
innervated loose
connective tissue derived
from TV surrounds STs.
• Interstitial cells of Leydig
make groups within this
CT.
Testes
• Seminiferous epithelium of
STs produces
spermatozoa.
• Spermatozoa enter tubuli
recti that connect the open
end of each ST to rete
testis (labyrinthine spaces
within MT).
• Spermatozoa leave the RT
through ductuli efferentes
(10-20 short tubules)
which fuse with
epididymis.
Testes: vascular supply
• The vascular supply of each testis is derived from testicular
artery descending with testis into scrotum with ductus
deferens (vas deferens)
• The TA give branches before piercing the capsule to form
intratesticular elts.
• Testicular capillary beds are collected into pampiniform
plexus of veins which are wrapped around the testicular
artery
• Artey, veins and the ductus deferens form the spermatic
cord.
• PP blood is cooler than TA; reduce the arterial blood
temperature ...form a countercurrent heat exchange
system. Testes temp is kept lower (35 oC)...spermatozoa
develop normally
Seminiferous tubules
• 30-70 cm long, 150-250
m in diameter highly
convoluted tubules
(total1000 STs in two
testes, total length 0.5
km)
• Tunica propria (slender CT)
and thick seminiferous
(germinal) epithelium
make the wall of ST
• A basal lamina separates
SE and the TP
• TP contains type 1 collagen
bundles housing several
layers of fibroblasts (myoid
cells in aimals not
humans).
• There are spermatogenic
cells and the Sertoli cells
Seminiferous tubules, some of which are outlined, and groups
within the SE.
of pale-stained interstitial (Leydig) cells (arrowheads).
Pararosaniline—toluidine blue (PT) stain.
Sertoli cells
• Tall columnar cells, with a basal
clear oval nucleus and complex
infoldings at the apical and
lateral cell membranes
• Contain cytoplasmic inclusions
crystalloids of Charcot-Böttcher
with unknown function
• Cell cytoplasm is filled with SER,
has many mitochondria and a
well developed Golgi apparatus.
• Lat. cell membranes of adjacent
Sertoli cells form occluding
junctions subdividing the lumen
of the ST into narrower basal
and the wider adluminal
compartments.
• The ZOs of Sertoli cells establish
a blood-testis barrier that
isolates the adluminal
compartment from CT influences
thereby protecting the
developing gametes from the
immune systeme.
Blood-testis barrier
• Sertoli cells form the bloodtestis barrier.
• Basal compartment comprises
the interstitial space and the
spaces occupied by the
spermatogonia.
• Adluminal compartment
comprises the tubule lumen and
the intercellular spaces down to
the level of the occluding
junctions (OJ). In this
compartment are
spermatocytes, spermatids, and
spermatozoa.
• Cytoplasmic residual bodies
from spermatids undergo
phagocytosis by the Sertoli cells
and are digested by lysosomal
enzymes.
• Myoid cells surround the
seminiferous epithelium.
Sertoli cells function in:
• supporting the developing
spermatogenic cells;
• establishing the bloodtestis barrier;
• phagocytosis of cytoplasm
shed by developing
spermatogenic cells;
• manufacturing the
following substances:
androgen binding protein,
antimullerian hormone,
inhibin, testicular
transferrin, and a fructoserich medium.
Spermatogenic cells
•Most of the cells composing
the thick seminiferous
epithelium are
spermatogenic cells in
various stages of maturation.
Spermatogonia, are located
in the basal compartment,
•Primary spermatocytes,
secondary spermatocytes,
spermatids,spermatozoa
occupy the adluminal
compartment.
•Spermatogonia are diploid
cells that undergo mitotic
division to form more
spermatogonia, primary
spermatocytes, which
migrate from the basal into
the adluminal compartment.
Spermatogenesis
• Primary spermatocytes
enter the first meiotic
division to form
secondary spermatocytes,
which undergo the second
meiotic division to form
haploid cells known as
spermatids.
• Spermatids are
transformed into
spermatozoa by shedding
of much of their
cytoplasm, rearrangement
of their organelles, and
formation of flagella.
• Part of the wall of a
seminiferous tubule.
Several cells of the
spermatogenic lineage are
present: a
spermatogonium, primary
spermatocytes, and young
and late spermatids. The
approximate limits of a
Sertoli cell holding several
spermatids are delineated.
H&E stain. High
magnification.
• Spermatocytes and
spermatids in the
epithelium of a
seminiferous
tubule. The tubule
is covered by
myoid cells..
Spermatids
• Electron micrograph of a
mouse spermatid. In the
center is the nucleus,
covered by the acrosome.
The flagellum can be seen
emerging in the lower
region below the nucleus.
A cylindrical bundle of
microtubules, the
manchette, limits the
nucleus laterally. (Courtesy
of KR Porter.)
The maturation process
(spermatid....spermatozoa)
– Spermatocytogenesis:
spermatogonia
differentiate into primary
spermatocytes
– Meiosis: reduction
division whereby diploid
primary spermatocytes
reduce their
chromosome
complement, forming
haploid spermatids
– Spermiogenesis:
transformation of
spermatids into
spermatozoa (sperm)
Spermatogenesis
• Diagram showing the
clonal nature of the germ
cells. Only the initial
spermatogonia divide and
produce separate daughter
cells.
• Once committed to
differentiation, the cells of
all subsequent divisions
stay connected by
intercellular cytoplasmic
bridges.
• Only after they are
separated from the
residual bodies can the
spermatozoa be considered
isolated cells.
Spermiogenesis
• The
principal
changes
occurring
in
spermatids
during spermiogenesis are
demonstrated.
• The basic structural feature of
the spermatozoon is the
head, which consists primarily
of
condensed
nuclear
chromatin.
• The reduced volume of the
nucleus affords the sperm
greater mobility and may
protect the genome from
damage while in transit to the
egg.
• The rest of the spermatozoon
is structurally arranged to
promote motility.
• Bottom: The structure of a
mature spermatozoon.
Spermatozoon
• Spermatids discard much of
their cytoplasm and form a
flagellum to become
transformed into
spermatozoa, a process
known as spermiogenesis.
• Spermatozoa (sperm) are
long cells (~65 μm),
composed of a head, housing
the nucleus, and a tail, which
accounts for most of its
length
• Tail of the spermatozoon is
subdivided into four regions:
neck, middle piece, principal
piece, and end piece. The
plasmalemma of the head is
continuous with the tail’s
plasma membrane.
Spermatozoon
• Neck (~5 μm long) connects the
head to the remainder of the tail.
It is composed of the cylindrical
arrangement of the nine columns
of the connecting piece that
encircles the two centrioles, one
of which is usually fragmented.
The posterior aspects of the
columnar densities are continuous
with the nine outer dense
fibers.
• Middle piece (~5 μm long) is
located between the neck and the
principal piece. It is characterized
by the presence of the
mitochondrial sheath, which
encircles the outer dense fibers
and the centralmost axoneme.
The middle piece stops at the
annulus. Two of the nine outer
dense fibers terminate at the
annulus; the remaining seven
continue into the principal piece.
Spermatozoon
Principal piece (~45 μm long)
is the longest segment of the
tail and extends from the
annulus to the end piece. The
axoneme of the principal
piece is continuous with that
of the middle piece.
Surrounding the axoneme are
the seven outer dense fibers
that are continuous with
those of the middle piece and
are surrounded, in turn, by
the fibrous sheath.
End piece (~5 μm long) is
composed of the central
axoneme surrounded by
plasmalemma. The axoneme
is disorganized in the last 0.5
to 1.0 μm.
Spermatozoon
• Scanning electron
micrograph of a
spermatozoon in
the uterine cavity
of a rodent. The
tufts are ciliated
epithelial cells.
x2,000.
Leydig cells
• Luteinizing
hormone
(LH),
a
gonadotropin released from the
anterior pituitary gland, binds to LH
receptors on the Leydig cells,
activating adenylate cyclase to form
cyclic adenosine monophosphate
(cAMP).
Activation
of
protein
kinases of the Leydig cells by cAMP
induces
inactive
cholesterol
esterases to become active and
cleave
free
cholesterol
from
intracellular lipid droplets. The first
step in the pathway of testosterone
synthesis
is
also
LH-sensitive
because LH activates cholesterol
desmolase, the enzyme that
converts
free
cholesterol
into
pregnenolone.
• The various products of the
synthetic pathway are shuttled
between the smooth endoplasmic
reticulum and mitochondria until
testosterone, the male hormone,
is formed and is ultimately released
by these cells.
Leydig cells
• Epithelium of
seminiferous tubules
surrounded by myoid
cells. The spaces
between the tubules
contain connective
tissue, blood and
lymphatic vessels, and
interstitial cells.
Leydig cells
Interstitial cells and
cells of the
seminiferous
epithelium. H&E
stain. High
magnification.
Leydig cells
• Electron micrograph of
a section of an
interstitial cell. There
is abundant smooth
endoplasmic reticulum
as well as
mitochondria. Medium
magnification.
Hormonal relationships
• Because
blood
testosterone levels are not
sufficient to initiate and
maintain spermatogenesis,
FSH induces Sertoli cells to
synthesize
and
release
androgen-binding
protein (ABP). ABP binds
testosterone,
thereby
preventing the hormone
from leaving the region of
the seminiferous tubule
and
elevating
the
testosterone levels in the
local
environment
sufficiently
to
sustain
spermatogenesis.
Hormonal relationships
• Release of LH is inhibited by
increased
levels
of
testosterone
and
dihydrotestosterone, whereas
release of FSH is inhibited by
the hormone inhibin, which
is produced by Sertoli cells.
• Testosterone is also required
for the normal functioning of
the seminal vesicles, prostate,
and bulbourethral glands as
well as for the appearance
and maintenance of the male
secondary
sexual
characteristics. The cells that
require testosterone possess
5α-reductase, the enzyme
that converts testosterone to
its
more
active
form,
dihydrotestosterone.
Hypophyseal control of male
reproduction
• Luteinizing hormone
(LH) acts on the
Leydig cells,
• Follicle-stimulating
hormone (FSH) acts
on the seminiferous
tubules. A testicular
hormone, inhibin,
inhibits FSH secretion
in the pituitary.
Intratesticular genital ducts
• Tubuli recti
• Rete testis
•Connect seminiferous tubules to epididymis
Tubuli recti
• Short, straight tubules
delivering spermatozoa
from the seminiferous
tubules into rete testis.
• Lined by Sertoli cells in
their first half near the ST
• Formed by seminiferous
epithelium, lined by a
simple cuboidal epithelium
in their second half near
the rete testis
• Cuboidal cells have short
stubby microvilli and most
have a single flagellum
Rete testis
• Consists of labyrinthine
spaces lined by a simple
cuboidal epithelium within
the mediastinum testis.
• Cuboidal cells resemble
those of tubuli recti; have
numerous short microvilli
with a single flagellum
• Immature spermatozoa
pass from tubuli recti into
rete testis
Ductuli efferentes
• 10-20 short tubules that drain
spermatozoa from the rete
testis andpierce the tunica
albuginea of testis to conduct
the sperm to epididymis
• Simple epithelium contains
noncilliated cuboidal cells or
cilliated columnar cells
• Cillia of the columnar cells
move the spermatozoa
toward the epididimis
• Cuboidal cells having many
lysososomes and apical
plasmolemmal invaginations
are responsible of endocytosis
(resorb most of the luminal
fluid)
• Epithelium sits on a BL that
separates it from the thin
loose CT wall of each ductule
• CT is surrounded by a thin
layer of circularly arranged
smooth muscle.
Extra testicular genital ducts
• Epididymis
• Ductus deferens
• Ductus ejaculatorius
Epididymis
• Secrete numeruous factors that facilitate the maturation of
spermatozoa; but spermatozoa cannot fertilize a secondary
oocyte untill they undergo capacitation; a process trigered
by secretions produced in female genital system.
• Is a thin, long (4-6 m), highly convoluted tubule consisting
of a head, body and tail.
• The lumen is lined by pseudostratified epithelium composed
of two cell types: short basal cells with round nuclei
functioning as stem cells and the tall principal cells with
basally located oval nuclei and stereocillia, resorbing the
luminal fluid and manifacturing glycerophosphocholine (a
glycoprotein that inhibits spermatozoon capacitation
preventing spermatozoon from fertilizing a secondary
oocyte untill the sperm enters the female genital tract)
• Epith is separated from the underlying loose coonective
tissue by a BL
• Circularly arranged smooth muscle cells surround the CT
layer. Peristaltic contractions of this layer help conduct the
spermatozoa to the ductus deferens.
Epididymis
• Highly coiled ductus
epididymidis, sectioned
several times.
• Its wall is made of a
pseudostratified columnar
epithelium surrounded by
connective tissue and
smooth muscle.
• Inset: Higher magnification
of the epithelial cells with
their long microvilli
(stereocilia).
Ductus deferens (Vas
deferens)
• Each DF is a thick walled
muscular tube with a small
irregular lumen that conveys
the spermatozoa from the tail
of the epididimis to the
ejaculatory duct.
• Mucosa formed by
pseudostratified columnar
epithelium (principal cells are
shorter) with stereocilia and a
lamina propria.
• Thick outer wall is formed of
smooth muscle (three
layers:inner outer
longitudunal middle circular)
and collagen fibers (blue).
• SML isinvested by a thin layer
of fibroelastic connective
tissue
Extra testicular genital ducts
• The dilated terminus of
each ductus deferens is
known as ampulla
• As the ampula approaches
the prostate gland it is
joined by seminal vesicle.
• The continuation of the
junction of the ampulla
with the seminal vesicle is
known as ejaculatory duct.
Ejaculatory duct
• Ampulla of ductus deferens
joins the seminal vesicle to
form ejaculatory duct;
which then enters the
prostate gland and opens
in the prostatic urethra at
the colliculus seminalis.
• Is a short straight tubule
• Lumen is lined by simple
columnar epithelium
• Subepithelial CT is folded
• Has no smooth muscle in
its wall.
Accessory genital glands
• Paired seminal
vesicle
• Single prostate
gland
• Paired
bulbourethral
glands
Seminal vesicles
• About 15 cm long highly tubular structures located between post
aspect of the neck of the bladder and the prostate gland; and join
the ampulla of the ductus deferens just above the prostate gland
• Its mucosa is highly convoluted forming labyrinth-like cul-de-sacs
that are observed to open into a central lumen.
• Lumen is lined by a pseudustartified columnar epithelium (short
basal cells and low columnar)
• Each columnar cell cell-with numerous short microvilli and a single
flagellum
• Subepithelial fibroelastic CT is surrounded by inner circular outer
longitudinal smooth muscle coat
• SM is surrounded by fibroelastic CT again
• This gland produces a viscose yellow fructose rich seminal fluid
that makes 70% of the volume of the semen. It is the source of
the enery for the spermatozoa.
• The characteristic pale yellow colour of semen is due to the
lipochrome pigment released by seminal vesicles
Seminal vesicles
• Tortuous tubular
gland with a muchfolded mucosa
gives the
impression that the
gland consists of
many tubules.
Prostate
• Is the largest of the accessory
glands, is pierced by the
urethra and the ejaculatory
ducts.
• Slender
capsule
is
composed
of
a
richly
vascularized, dense irregular
dense
connective
tissue
interspersed with smooth
muscle cells.
• Connective tissue stroma of
the gland is derived from the
capsule and is, therefore, also
enriched by smooth muscle
fibers in addition to their
normal
connective
tissue
cells.
• Is a conglomeration of 30 to
50
individual
compound
tubuloalveolar glands,
• is arranged in three discrete,
concentric layers mucosal,
submucosal, and main.
Prostate
• Mucosal glands are closest
to the urethra and thus are
the shortest of the glands
• Submucosal glands are
peripheral to the mucosal
glands and are consequently
larger than the mucosal
glands.
• Largest and most numerous of
the glands are the
peripheralmost main glands,
which compose the bulk of the
prostate.
• Lumina of the tubuloalveolar
glands frequently house round
to oval prostatic concretions
(corpora amylacea),
composed of calcified
glycoproteins, whose numbers
increase with a person’s age.
Prostate
• Distribution of
its glands in 3
zones. The gland
ducts open into
the urethra.
Prostate
• Section of the
central region of
the prostate
showing the
prostatic urethra
and tubuloalveolar
glands surrounded
by connective
tissue and smooth
muscle.
Prostate
• Components of
prostate gland
are lined by a
simple to
pseudustratified
to columnar
epihelium;
surrounded by
connective tissue
and smooth
muscle.
Prostatic secretion
• Constitutes a part of
semen.
• Is a serous, white fluid
rich in lipids, proteolytic
enzymes,
acid
phosphatase,
fibrinolysin, and citric
acid.
• Formation,
synthesis,
and
release
of
the
prostatic secretions are
regulated
by
dihydrotestosterone,
the
active
form
of
testosterone
Bulbourethral (Cowper’s) glands
• Paired small (3-5 mm diam)
glands located at the root of
penis, just just at the
beginning of membranous
urethra
• Capsule contains fibroblasts,
smooth and skeletal muscle
cells (sk muscle derived from
the muscles of the urogenital
diaphragm)
• Capsule sends septa dividing
each gland into lobules
• Epith of these compound
tubuloalveolar glands varies
from simple cuboidal to
simple columnar
• The secretion is a thick
slippery fluid that lubricate
the lumen of the urethra
Penis
• Is composed of three columns of
erectile tissue, each enclosed by
its own dense, fibrous connective
tissue capsule, the tunica
albuginea.
• Two of the columns of erectile
tissue, the corpora cavernosa,
are positioned dorsally; their
tunicae albugineae are
discontinuous in places, permitting
communication between their
erectile tissues.
• Third column of erectile tissue, the
corpus spongiosum, is
positioned ventrally. Because the
CS houses the penile portion of the
urethra, it is also called the
corpus cavernosum urethrae.
• CS ends distally in an enlarged,
bulbous portion, the glans penis
(head of the penis). The tip of the
glans penis is pierced by the end of
the urethra as a vertical slit.
Penis
• Three corpora are surrounded
by a common loose connective
tissue
sheath,
but
no
hypodermis, and are covered by
thin skin.
• Skin continues distal to the
glans penis to form a retractable
sheath, the prepuce. When an
individual is circumcised, it is
the prepuce that is removed.
• Erectile tissue of the penis
contains
numerous
variably
shaped,
endothelially
lined
spaces.
• Vascular spaces of the corpora
cavernosa are larger centrally
and smaller peripherally, near
the tunica albuginea.
• Vascular spaces of the corpus
spongiosum are similar in size
throughout its extent.
Penis