Module B: Clinical Care – Diagnosis

Module B: Clinical Care – Diagnosis
Standard 3
The practice will demonstrate evidence of a system for early and accurate diagnosis of respiratory disease
Rationale
There is significant under-diagnosis of COPD in the community and practices should be able to demonstrate that they provide COPD screening at suitable opportunities.
Early and accurate diagnosis of respiratory disease is vital for appropriate and successful interventions.
The ability to investigate appropriately and interpret the information leads to accurate diagnoses and relevant successful treatments. Practices will be able to provide evidence, reflecting current national guidance, on how asthma and COPD are diagnosed. Evidence of spirometry should demonstrate that it meets current diagnostic standards and interpretation of spirometry should be in keeping with ATS/ERS standards.
1
Evidence required to support application (2 parts, both must be completed)
Evidence Case finding
5
The practice will describe (maximum one side A4, Arial font point size 12) the systems available for case finding in COPD and provide a reflective paragraph on the successes/challenges of case finding in COPD .
Evidence Diagnosis
8
7b
6a (asthma)
6b (COPD)
7a
The practice will provide its policy for the diagnosis of asthma and COPD and include evidence of the use of spirometry in the diagnostic process according to nationally recognised standards.
1,2
The practice will demonstrate that its diagnosis policy is effective by providing an example of a patient journey or case study on the diagnosis of asthma OR COPD.
The practice must include a reflective narrative including an action plan for maintaining or improving the standards of diagnosis of respiratory conditions in the practice including identification of misdiagnosed or undiagnosed patients 1
The practice will provide an audit of a representative sample (Either 10% or
20 patients whichever is the greater) of its spirometry practice using the audit template provided including reflection and action plan (See Appendix
5). Practices should be able to demonstrate that 90% of patients diagnosed with COPD have had their diagnosis confirmed by spirometry (with
1
legitimate exceptions taken into account – details must be provided)
References
1.
Levy ML, Quanjer PH, Booker R, Cooper BG, Holmes SGT, Small I. Diagnostic spirometry in primary care: proposed standards for general practice compliant with
American Thoracic Society and European Respiratory Society recommendations. Prim
Care Respir J 2009;18(3):130–47. http://www.thepcrj.org/journ/view_article.php?article_id=653
2.
An outcomes strategy for people with chronic obstructive pulmonary disease (COPD) and asthma in England. Department of Health 2011. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_127974 Last accessed 6 Feb 2013
Further information
1.
National Institute for Health and Clinical Excellence NICE. Quality Standard for
Asthma. QS25, Feb 2013. http://publications.nice.org.uk/quality-standard-forasthma-qs25 [accessed 25/03/2013]
2.
"Invisible Lives Key Findings: A Summary" http://www.blf.org.uk/Files/94ff4ae1-
1858-485f-ae85-a06200ded618/Invisible-Lives-report.pdf
[accessed 16/03/2013
3.
Department of Health COPD Consultation document. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_116716 [accessed 16/03/2013]
4.
ATS/ERS spirometry standards: Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi
R, Coates A, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. http://www.thoracic.org/statements/resources/pfet/PFT2.pdf
[accessed
16/03/2013].
5.
Levy ML, Quanjer PH, Booker R, Cooper BG, Holmes SGT, Small I. Diagnostic spirometry in primary care: proposed standards for general practice compliant with
American Thoracic Society and European Respiratory Society recommendations. Prim
Care Respir J 2009;18(3):130–47. http://www.thepcrj.org/journ/view_article.php?article_id=653
6.
An Outcomes Strategy for COPD and Asthma: NHS Companion Document.
Department of Health 2012. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_134000 Last accessed 16/03/2013
7.
Starren ES, Roberts NJ, Tahir M, O'Byrne L, Haffenden R, Patel IS, Partridge MR. A centralised respiratory diagnostic service for primary care: a 4-year audit. Prim Care
Respir J 2012;21(2):180-186. DOI: http://dx.doi.org/10.4104/pcrj.2012.00013
2
[accessed 25/03/2013]
8.
The PCRS-UK has a wide range of tools and resources ranging from nurse patient group directions, nurse protocols and checklists, a series of well respected PCRS-UK opinion sheets and other supported materials. You can access all these materials by using resource directory - http://www.pcrs-uk.org/resource/search
More information on the spirometry audit
Spirometry Audit
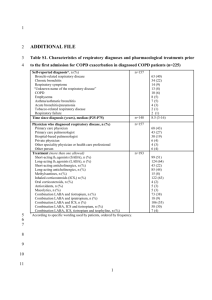
Each participating practice is required to complete an audit of spirometry in primary care.
This audit may be conducted manually in the practice using the standards shown below and the patient data collection template (see page 28) or electronically using our online audit facility which provides an auto-generated report upon completion and allows practices to compare their own results with other practices who have participated in the audit. If you wish to use the electronic version please contact the award administrator for a username and password (tricia@pcrs-uk.org). The electronic audit can be accessed at http://www.guideline-audit.com/pcrsuk_copd_dx/instructions.php
The standards for this audit are shown below:
1.
90% of patients diagnosed with COPD have current smoking status recorded.
2.
90% of patients diagnosed with COPD have had their diagnosis confirmed by spirometry.
3.
100% of patients who have had spirometry should have a tracing/spirogram in the records.
4.
100% of diagnosed COPD patients have a record of an FEV1/FVC ratio
<70% OR FEV1/RelaxedVC ratio <70%.
5.
In 90% of patients there should be a minimum of three good relaxed and three forced post-bronchodilator readings.
6.
In 90% of patients the two best FEV1 and two best FVC readings should be within 150ml of each other. This should also apply to the relaxed vital capacity.
Note: Practices failing to achieve the standards set will not necessarily be penalised provided they can provide an adequate explanation for the failure to achieve the standards and/or have a clear action plan in place detailing how they plan to address the issues highlighted as a result of the audit.
Number of records required
Please list all the patients diagnosed with COPD in your practice and then randomly select at least 20 patients. There are various ways of getting a random selection of patients; the important thing is to try get a fairly representative sample. Example methods for selecting a
3
sample from the list of COPD patients include: If there are a small number of COPD patients in the practice, then choose every 5th patient in the list. In larger practices choose every
11th or 21st patient, for example, so that a selection is made across the spread of the list.
Please continue from the top of the list if you get to the bottom and do not have 20 selected.
4
5