Chronic Obstructive Pulmonary Disease Specification 2015
advertisement

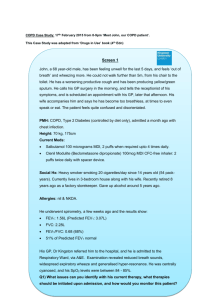
Barns Medical Practice Service Specification Outline: The Diagnosis and Management of Chronic Obstructive Pulmonary Disease DEVELOPED February 2015 REVIEW DATE February 2017 Introduction Chronic Obstructive Pulmonary Disease (COPD) is characterised by airflow obstruction that is not fully reversible. It is progressive and predominantly caused by smoking. The damage is the result of chronic inflammation that differs from that seen in asthma. The object of correct management of COPD is to reduce mortality, reduce exacerbations and cut down hospital admissions. It also hopes to achieve optimum health benefits. Symptoms tend to be breathlessness on exertion, chronic cough, regular sputum production, frequent winter bronchitis or wheeze. Consideration should also be given to those complaining of fatigue, effort intolerance, weight loss, ankle swelling, chest pain and haemoptysis (coughing up blood). Diagnosis The diagnosis should be based on signs and symptoms, history taking and supported by a breathing test called spirometry and reversibility. Patients are generally over 35, smokers and with one or more of the above symptoms. The MRC, 1 to 5 dyspnoea score is recorded to ascertain the degree of breathlessness incurred. If spirometry results show an FEV1 (Forced Expiratory Volume) less than 80% predicted and FEV1/FVC is less than 0.7 a diagnosis can be confirmed. If FEV1 greater than 80% refer back to GP for differential diagnosis. Annual Review - - A 20min appointment should be offered with practice nurse and the Long-term review template for COPD within consultation manager in Vision software. MRC score must be recorded Pulse oximetry should be taken and recorded Smoking status and cessation advice offered Inhaler technique observed/taught. Spacer devices should be compatible with the patient’s metered dose inhaler. Inhaled drugs should be administered by repeat single actuations and tidal breathing used. They should be cleaned no less than once per month and replaced annually. Vaccinations for influenza and pneumococcal should be offered Self management and medication in reserve should be discussed and appropriate education given. Where indicated the anticipatory care plan should be completed. If MRC score is greater than 3, a referral to pulmonary rehabilitation should be offered. A practice information leaflet regarding this service is stored on Barnsnet. Guidance on referral for Pulmonary Rehabilitation can be found by following the link below. - http://athena/pdu/respiratory/Documents/Pulmonary%20Rehab%20Guidance%20for%20R eferrers_Feb%202015.pdf The criteria for referral to pulmonary rehab can be found by following this link http://athena/pdu/respiratory/Documents/PULM%20REHAB%20CRITERIA_Jan%2013.pdf Treatment 1. Breathlessness and exercise limitation. Offer short-acting bronchodilators. This can be administered via a spacer device. 2. Exacerbation or persistent breathlessness. If FEV1 is greater or equal to 50%-Add twice daily Salmeterol MDI 25mcgs two puffs via spacer. 2nd choice Glycopyrronium Breezhaler 50mcgs one puff daily If FEV1 is less than or equal to 50 % then add Glycopyrronium 50mcgs one puff daily. Add inhaled steroid, i.e Symbicort 400/12mcg one puff twice daily or Seretide 500 one puff daily if LAMA not controlling symptoms. Oral mucolytic therapy should be considered in patients with a chronic cough and productive sputum. Do not use mucolytic to prevent exacerbations. Carbocysteine 375mg capsules in divided doses initially as 2.25g daily then reduce to 1.5g daily. Resources for Staff and or Patients Information leaflets regarding COPD can be found on the internet. Patient.co.uk is useful as a source of information. Patients can be signposted to Fresh –air-shire if they wish any additional assistance with smoking cessation. See links below. http://www.patient.co.uk/health/chronic-obstructive-pulmonary-disease-leaflet http://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease/Pages/Introduction.aspx http://www.nhsaaa.net/services-index/f-fresh-air-shire.aspx http://inps80081w2k3/Clinical%20Protocols/Respiratory%20System/COPD%20quick%20guide% 20for%20primary%20care.pdf NHS A&A Pulmonary Rehab Programme June 2015 http://www.clydesideactiononasbestos.org.uk/ http://mylungsmylife.org/ Chest heart and stroke Scotland Frequently asked questions re. pulmonary rehabilitation. Follow link belo w http://athena/pdu/respiratory/Documents/F32_Pulmonary_Rehabilitation.pdf Staff involved and training required 1. All RGNs within the practice have completed COPD education and are committed to regular update sessions and review via appraisal. 2. For the purpose of diagnosis, the HCA assistant has been delegated the task to carry out the spirometry procedure. She has been taught by trained staff and has been deemed as competent. She must report to GP or RGN if encounters any problems. The GP or practice nurse who orders spirometry must prescribe Salbutamol via vision prior to procedure if this is requested. (See appendix 1) Advertising of service to patients Patients are invited annually by letter. Reminders can be sent by post and reminders about appointments by text. Barns Medical Practice advertises this service on the internet and actively encourages patients to make annual review appointments. REFERENCES http://www.goldcopd.org/uploads/users/files/GOLD_Report_2014_Jan23.pdf Protocol for Spirometry and Reversibility Management by Health Care Assistants DATE CREATED 2/02/2015 REVIEW DATE 2/02/2017 PURPOSE OF PROTOCOL To enable suitably trained Health Care Assistants working for or on behalf of BARNS MEDICAL PRACTICE who have undertaken relevant training (as outlined below), to carry out spirometry and reversibility as a duty delegated by the General Practitioner or a registered nurse. The results of the test are then examined / assessed by a GP or nurse with a special interest in Chronic Obstructive Pulmonary Disease (COPD) and is used as an add to diagnosis of the condition COPD. AIM To help provide a service in prompt diagnosis of COPD where indicated. AUTHORITY TO PROCEED In accordance with HCA code of conduct (Scottish Gov., 2009) and with the training and skills listed below. TRAINING + SKILLS Completion of HCA induction training course on the use of the spirometer for reversibility testing and to be given a basic understanding of this condition and its complications. Completion of period of supervised practice and completion of assessment of competence Training and competence in the correct procedure for onward referral or management of any concerning features on the day of review. Appropriate anatomy and physiology knowledge Access to and knowledge of relevant guidance/ protocols re. COPD Demonstration of competence in relation to this delegated duty within the PDP and appraisal ELIGIBILITY CRITERIA INCLUSION/EXCLUSIONS All patients who have been referred by a trained clinician, working within BARNS MEDICAL PRACTICE. This protocol requires that there is a written instruction regarding the administration of salbutamol within the patient record. Exclude patients who present with an active infection and arrange another visit. CLINIC PROTOCOL 1. A 20 minute appointment will be offered allowing the patient to have the initial breathing test and salbutamol administered. They will then be asked to wait in the waiting area for the medication to take effect for 20minutes and then a further 20 minute appointment will be given to allow completion of the investigation. 2. Consultation will be carried out in privacy of a consulting room. 3. Computerised notes will be made available. Assessment Patients should not have used salbutamol or smoked a cigarette for 4 hours prior to this investigation They should be advised to wear loose fitting clothes They should wear nose plugs They should not be fighting any active respiratory tract infection at time of investigation The investigation should aim to achieve x3 relaxed blows and x 3 forced blows within 5% of best blow. Record Keeping An entry will be made by the HCA and the spirometry report will be electronically uploaded and attached to the notes. 1. With the spirometer switched off, connect the data cable and insert dongle into side of communication port. 2. Open Care Fusion software and hightlight spirometer. 3. Click upload, new file 4. Search for patient’s name and click review results. 5. Click data-export-selected examination-export examination to pdf and attach. 6. Open patients records, add attachment and save. Name file spirometry Audit Health Care Assistants will be expected to participate in audit in relation to patient outcomes and the development of this role. Management of Significant Event Any significant event which occurs during a COPD consultation must be reported to the Practice Manager / General Practitioner or the Registered Nurse / Manager and the incident reported via the Barns Medical Practice significant event document.