Biochemistry Ch 26 477-492 [4-20
advertisement
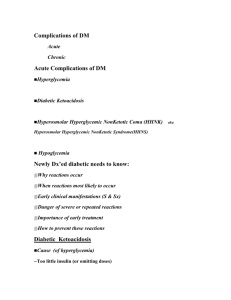
Biochemistry Ch 26 477-492 Basic Concepts in Regulation of Fuel Metabolism Metabolic Homeostasis – cells need ATP for maintenance of normal cell function; control of balance between substrate need and substrate availability is called metabolic homeostasis 1. Concentration of plasma nutrients/metabolites affects rate of usage in tissues 2. Hormones tell tissues about physiologic body state and level of nutrient demand 3. CNS uses neural signals to control tissue metabolism through hormone release -concentration of fatty acids in blood is major factor whether skeletal muscles will use fatty acids or glucose for fuel -hormones are intravascular carriers of messages between site of synthesis and tissues -epinephrine – hormone used in times of stress where increased fuel demand exists -insulin – major anabolic hormone of the body promoting fuel storage and use -glucagon – major hormone of fuel mobilization -many tissues depend on glycolysis for their energy, necessitating that tissues have constant supple to glucose to meet their ATP need -adult requires minimum of 190g glucose/day (140 for brain and 40 for other tissues) -decreases in glucose metabolism leads to hypoglycemic symptoms -if glucose and AA could not enter cells, they would be at such high concentrations in the blood that the hyperosmolar effect would cause progressive neurologic deficit/coma -glucose/AA would rise above renal tubular threshold for absorption and they’d spill into urine -nonenzymatic glycosylation would rise to alter function of many tissues -triacylglycerols (those in chylomicrons and VLDLs) would rise and cause atherosclerotic buildup) -hyperglycermia can cause polyuria/polydipsia; caused by osmotic diuresis resulting from high levels of glucose in urine, which would decrease plasma volume Major Hormones of Metabolic Homeostasis – insulin is major anabolic hormone promoting storage of nutrients: storage of glycogen in liver and muscle, converts glucose to triacylglycerols in liver and storage in adipose, and AA uptake/protein synthesis in skeletal muscle Glucagon maintains fuel availability in absence of dietary glucose by stimulating release of glucose from liver glycogen -also stimulates gluconeogenesis from lactate, glycerol, and AA; and mobilizes fatty acids from adipose to provide alternate source of fuel -release of insulin from β-cells of pancreas dictated by high levels of glucose in blood touching the B cells in the islets of Langerhans (highest is 30-45 minutes after high carb meal) -release of glucagon from α-cells is controlled through reduction of glucose/rise in insulin -lowest concentration of glucagon is right after a carb rich meal -circulating hormones like epinephrine, norepinephrine, cortisol oppose insulin/mobilize fuels -release of these hormones is mediated by neuronal signals Synthesis and Release of Insulin/Glucagon 1. Endocrine Pancreas – α cells secrete glucagaon/β cells secrete insulin into portal vein 2. Synthesis and Secretion of Insulin – insulin is a peptide composed of A and B chain linked by disulfide bonds a. Insulin synthesized as a preprohormone that is converted in rER to proinsulin (presignal is cleaved as it enters ER) b. Proinsulin is folds into conformation, acquires disulfide bonds and transfers to golgi i. During secretion from golgi vesicles, a protease removes the inactive C peptide to create functional insulin ii. Exocytosis of insulin is stimulated by glucose levels rising in blood iii. Zinc coprecipitates with insulin -glucose enters β cell through a glucose transporter GLUT 2; glucose is phosphorylated through glucokinase G6P metabolized through glycolysis, TCA, oxphos to increase ATP in β cell -as ATP:ADP increases, membrane bound ATP-dependent K channel is inhibited, leading to membrane depolarization which activates voltage-gated Ca channel that allows Ca to enter B cell such that intracellular Ca levels rise -as Ca rises, stimulates fusion of insulin exocytotic vesicles in plasma membrane for secretion Stimulation and Inhibition of Insulin Release – stimulation occurs within minutes of exposure to glucose; threshold is 80mg glucose/dL, above which is proportional to glucose concentration -pancreatic islets are autonomically innervated (including branch of vagus) to help with insulin secretion -Gastric inhibitory polypeptide (GIP) and Glucagon-like peptide 1 (GLP-1) -epinephrine, secreted in response to fasting, stress, trauma – decreases insulin release Synthesis and Secretion of Glucagon – glucagon is synthesized by α-cells of pancreas through cleavage of preproglucagon to proglucagon in RER -cleavage produces 29-AA glucagon sequence GLP-1 and GLP-2; rapidly metabolized by kidneys and liver and lives in plasma only 3-5 minutes -circulating levels of glucose and insulin regulate secretion of glucagon. Increasing levels of each inhibit glucagon release -catecholamines (epinephrine) and cortisol stimulate glucagon secretion -many amino acids stimulate glucagon release -insulin release stimulates AA uptake by tissues and enhances protein synthesis, but glucagon levels also increase in response to protein meal, and critical factor is the insulin-glucagon ratio -synthesis of glycogen and TGs is reduced when glucagon levels in blood rises -in fasting patients, average glucagon is 75 pg/mL Mechanisms of Hormone Action – hormones affect activity of specific enzymes or transport proteins that regulate flux through a pathway -ultimately, hormone must cause amount of substrate to increase, change conformation of active site by phosphorylating enzyme, change concentration of allosteric effector, or change amount of protein by inducing or repressing synthesis -insulin and glucagon use ALL of the above methods to determine rate of flux -phosphorylation causes immediate effects or within minutes, but hours for enzyme synthesis Signal Transduction by Hormones that Bind to Plasma Membrane Receptors – hormones bind to specific receptors or proteins (insulin/glucagon/catecholamines) act through membrane -1st message of hormone is transmitted to intracellular enzymes by activated receptor and intracellular second messenger (steroids enter cytoplasm) -3 types of signaling occur for hormones on receptors: 1. receptor coupling to adenylyl cyclase - cAMP 2. receptor kinase activity 3. receptor coupling to hydrolysis of PIP2 Signal Transduction by Insulin – insulin binds receptor on membrane of target cells -insulin receptor has 2 subunits: α which binds insulin, and β which protrudes into cytosol -the β subunit has tyrosine kinase activity -when insulin binds, tyrosine kinase phosphorylates tyrosine on β subunit as well as other substrates, such as insulin receptor substrate 1 (IRS-1) that recognizes and binds transduction proteins in SH2 domains -IRS-1 is involved in many physiologic responses to insulin grouped into 5 categories 1. insulin reverses glucagon-stimulated phosphorylation 2. insulin phosphorylates many enzymes 3. insulin induces and represses synthesis of various enzymes 4. acts as growth factor and has stimulatory effect on protein synthesis 5. stimulates glucose and AA transport into cells Signal Transduction by Glucagon – glucagon receptor/G protein = adenylate cyclase/cAMP -cAMP activates cAMP dependent protein kinase (PKA) which phosphorylates serines in enzyme -G proteins are membrane bound proteins that and GTP and have dissociable subunits -in absence of glucagon, the stimulatory Gs-protein complex binds GDP + cannot bind receptor -Once glucagon binds, receptor binds Gs-complex, which exchanges GDP for GTP -α subunit dissociates from βγ subunit and binds adenylate cyclase to activate it, hydrolyzing GTP to GDP -inhibitory G proteins are called Gi-complex proteins. Glucagon activates glucose in liver from glycogen but not skeletal muscle, because receptors are present in liver but not muscle -cAMP is degraded to membrane bound phosphodiesterases -cAMP is low in a cell, and fluctuates only in response to hormone -cAMP transmits signal by binding PKA subunits, which dissociate from catalytic subunits to activate them; activated PKA phosphorylates serines on key regulatory enzymes in carb and fat metabolism -changes in phosphorylation state of proteins that bind cAMP response elements (CREs) in promoter region of genes contribute to regulation of gene transcription by several cAMP coupled hormones -cAMP response element CREB protein is directly phosphorylated by PKA, necessary for transcription -major actions of glucagon occur in liver, adipose, and kidney -another principle is amplification of first message; glucagon present in blood at low concentrations, and only a small amount required to initiate cellular response because one molecule of glucagon can activate many PKA molecules -third principle is integration of metabolic responses; glucagon stimulated phosphorylation of enzymes activates glycogen degradation, inhibits glycogen synthesis, and inhibits glycolysis -fourth principle is augmentation and antagonism of signals -augmentation example is glucagon and epinephrine – these hormones bind different receptors which can each increase cAMP and stimulate glycogen degradation -fifth principle is rapid signal termination Signal transduction by cortisol and other hormones interacting intracellularly – hormones like cortisol bind intracellular receptors and moves into nucleus where it interacts with chromatin to regulate gene transcription -cortisol is synergistic to other hormones, for example: rates of transcription of enzymes in pathway of glucose synthesis from amino acids (gluconeogenesis) induced by cortisol Signal Transduction by Epinephrine and Norepinephrine – both can act as hormones or neurotransmitters -both prepare for fight/flight -bind to adrenergic receptors (9 of them) and work through adenylate cyclase-cAMP system by activating a Gs-protein to activate adenylate cyclase PKA -B1 receptor is major adrenergic receptor in human heart stimulated by norepinephrine, increases the rate of heart muscle contraction because of PKA mediated phosphorylation fo phosphlamban -B2 receptor is present in liver, skeletal muscle, and other tissues and is involved in mobilization of fuels and mediates vascular, bronchial, and uterine smooth muscle contraction -epinephrine is more potent for this than norepinephrine (major function is neuro) -B3 receptor found primarily in adipose and lesser extent in skeletal muscle. Activation stimulates fatty acid oxidation and thermogenesis; may help with weight loss -alpha1-receptors – postsynaptic receptors mediate vascular and smooth muscle contraction through PIP2 system via activation of Gq-protein and phospholipase C-B; also mediates glycogenolysis in liver Actions of Insulin – proposed mechanisms include inhibition of adenylyl cyclase, reduction of cAMP levels, stimulation of phosphodiesterase, production of insulin factor -mRNA for phosphoenolpyruvate carboxykinase (key enzyme in gluconeogenesis) is increased by glucagon and decreaed with insulin -insulin triggers phosphorylation cascade to phosphorylate protein subunits that bind to protein synthesis initiation factors (eIFs), and when phosphorylated, inhibitory proteins are released from eIFs allowing translation of mRNA to be stimulated -insulin receptor mediates internalization of receptor bound insulin molecules for degradation -receptor can be irreversibly degraded after prolonged occupation by insulin, called receptor downregulation, could lead to chronic hyperglycemia