The liver dual body supply portal vein: 60-70% hepatic artery: 30
advertisement
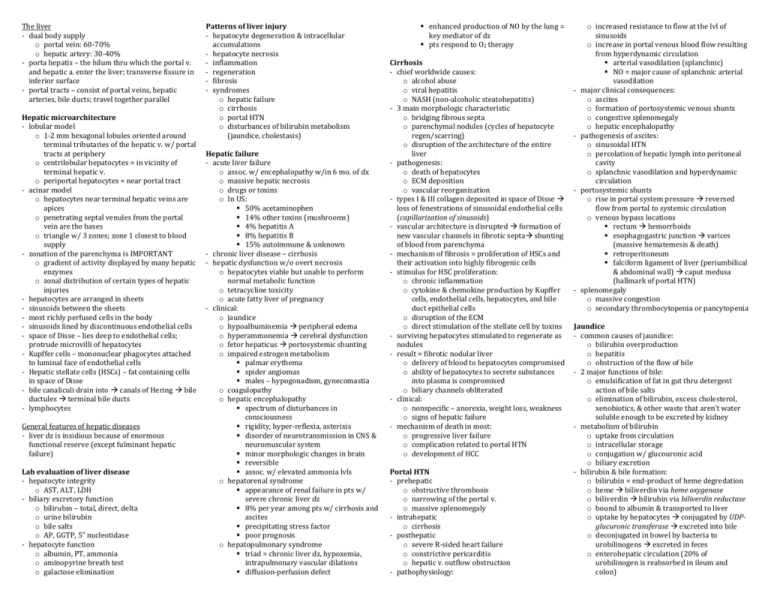
The liver - dual body supply o portal vein: 60-70% o hepatic artery: 30-40% - porta hepatis – the hilum thru which the portal v. and hepatic a. enter the liver; transverse fissure in inferior surface - portal tracts – consist of portal veins, hepatic arteries, bile ducts; travel together parallel Hepatic microarchitecture - lobular model o 1-2 mm hexagonal lobules oriented around terminal tributaries of the hepatic v. w/ portal tracts at periphery o centrilobular hepatocytes = in vicinity of terminal hepatic v. o periportal hepatocytes = near portal tract - acinar model o hepatocytes near terminal hepatic veins are apices o penetrating septal venules from the portal vein are the bases o triangle w/ 3 zones; zone 1 closest to blood supply - zonation of the parenchyma is IMPORTANT o gradient of activity displayed by many hepatic enzymes o zonal distribution of certain types of hepatic injuries - hepatocytes are arranged in sheets - sinusoids between the sheets - most richly perfused cells in the body - sinusoids lined by discontinuous endothelial cells - space of Disse – lies deep to endothelial cells; protrude microvilli of hepatocytes - Kupffer cells – mononuclear phagocytes attached to luminal face of endothelial cells - Hepatic stellate cells (HSCs) – fat containing cells in space of Disse - bile canaliculi drain into canals of Hering bile ductules terminal bile ducts - lymphocytes General features of hepatic diseases - liver dz is insidious because of enormous functional reserve (except fulminant hepatic failure) Lab evaluation of liver disease - hepatocyte integrity o AST, ALT, LDH - biliary excretory function o bilirubin – total, direct, delta o urine bilirubin o bile salts o AP, GGTP, 5” nucleotidase - hepatocyte function o albumin, PT, ammonia o aminopyrine breath test o galactose elimination Patterns of liver injury - hepatocyte degeneration & intracellular accumulations - hepatocyte necrosis - inflammation - regeneration - fibrosis - syndromes o hepatic failure o cirrhosis o portal HTN o disturbances of bilirubin metabolism (jaundice, cholestasis) Hepatic failure - acute liver failure o assoc. w/ encephalopathy w/in 6 mo. of dx o massive hepatic necrosis o drugs or toxins o In US: 50% acetaminophen 14% other toxins (mushrooms) 4% hepatitis A 8% hepatitis B 15% autoimmune & unknown - chronic liver disease – cirrhosis - hepatic dysfunction w/o overt necrosis o hepatocytes viable but unable to perform normal metabolic function o tetracycline toxicity o acute fatty liver of pregnancy - clinical: o jaundice o hypoalbuminemia peripheral edema o hyperammonemia cerebral dysfunction o fetor hepaticus portosystemic shunting o impaired estrogen metabolism palmar erythema spider angiomas males – hypogonadism, gynecomastia o coagulopathy o hepatic encephalopathy spectrum of disturbances in consciousness rigidity, hyper-reflexia, asterixis disorder of neurotransmission in CNS & neuromuscular system minor morphologic changes in brain reversible assoc. w/ elevated ammonia lvls o hepatorenal syndrome appearance of renal failure in pts w/ severe chronic liver dz 8% per year among pts w/ cirrhosis and ascites precipitating stress factor poor prognosis o hepatopulmonary syndrome triad = chronic liver dz, hypoxemia, intrapulmonary vascular dilations diffusion-perfusion defect enhanced production of NO by the lung = key mediator of dz pts respond to O2 therapy Cirrhosis - chief worldwide causes: o alcohol abuse o viral hepatitis o NASH (non-alcoholic steatohepatitis) - 3 main morphologic characteristic o bridging fibrous septa o parenchymal nodules (cycles of hepatocyte regen/scarring) o disruption of the architecture of the entire liver - pathogenesis: o death of hepatocytes o ECM deposition o vascular reorganization - types I & III collagen deposited in space of Disse loss of fenestrations of sinusoidal endothelial cells (capillarization of sinusoids) - vascular architecture is disrupted formation of new vascular channels in fibrotic septa shunting of blood from parenchyma - mechanism of fibrosis = proliferation of HSCs and their activation into highly fibrogenic cells - stimulus for HSC proliferation: o chronic inflammation o cytokine & chemokine production by Kupffer cells, endothelial cells, hepatocytes, and bile duct epithelial cells o disruption of the ECM o direct stimulation of the stellate cell by toxins - surviving hepatocytes stimulated to regenerate as nodules - result = fibrotic nodular liver o delivery of blood to hepatocytes compromised o ability of hepatocytes to secrete substances into plasma is compromised o biliary channels obliterated - clinical: o nonspecific – anorexia, weight loss, weakness o signs of hepatic failure - mechanism of death in most: o progressive liver failure o complication related to portal HTN o development of HCC Portal HTN - prehepatic o obstructive thrombosis o narrowing of the portal v. o massive splenomegaly - intrahepatic o cirrhosis - posthepatic o severe R-sided heart failure o constrictive pericarditis o hepatic v. outflow obstruction - pathophysiology: - - - - o increased resistance to flow at the lvl of sinusoids o increase in portal venous blood flow resulting from hyperdynamic circulation arterial vasodilation (splanchnic) NO = major cause of splanchnic arterial vasodilation major clinical consequences: o ascites o formation of portosystemic venous shunts o congestive splenomegaly o hepatic encephalopathy pathogenesis of ascites: o sinusoidal HTN o percolation of hepatic lymph into peritoneal cavity o splanchnic vasodilation and hyperdynamic circulation portosystemic shunts o rise in portal system pressure reversed flow from portal to systemic circulation o venous bypass locations rectum hemorrhoids esophagogastric junction varices (massive hematemesis & death) retroperitoneum falciform ligament of liver (periumbilical & abdominal wall) caput medusa (hallmark of portal HTN) splenomegaly o massive congestion o secondary thrombocytopenia or pancytopenia Jaundice - common causes of jaundice: o bilirubin overproduction o hepatitis o obstruction of the flow of bile - 2 major functions of bile: o emulsification of fat in gut thru detergent action of bile salts o elimination of bilirubin, excess cholesterol, xenobiotics, & other waste that aren’t water soluble enough to be excreted by kidney - metabolism of bilirubin o uptake from circulation o intracellular storage o conjugation w/ glucouronic acid o biliary excretion - bilirubin & bile formation: o bilirubin = end-product of heme degredation o heme biliverdin via heme oxygenase o biliverdin bilirubin via biliverdin reductase o bound to albumin & transported to liver o uptake by hepatocytes conjugated by UDPglucuronic transferase excreted into bile o deconjugated in bowel by bacteria to urobilinogens excreted in feces o enterohepatic circulation (20% of urobilinogen is reabsorbed in ileum and colon) o hepatic conjugating enzyme UGT1A1 product of UGT1 gene responsible for bilirubin glucuronidation mutation in UGT1A1 can cause CriglerNajjar syndrome type I & II and Gilbert syndrome o bile acids = highly effective detergents human bile acids = cholic & chenodeoxycholic acid - pathophysiology: o unconjugated bilirubin insoluble in H2O at physiologic pH exists in tight complexes w/ albumin (can’t be excreted in urine) o small amt exists as albumin-free anion in plasma can increase if becomes unbound from albumin by protein-binding drugs or in severe hemolytic dz can diffuse into tissues kernicterus – neurologic damage from erythroblastosis fetalis accumulation of unconjugated bilirubin in brain o conjugated bilirubin soluble, non-toxic, and only loosely bound to albumin excess can be excreted in urine o delta bilirubin covalently bound to albumin if there is prolonged elevated conjugated hyperbilirubinemia o jaundice occurs when equilibrium btwn bilirubin production & clearance is disturbed by: unconjugated excessive extrahepatic production o hemolytic anemias o resorption of blood from internal hemorrhage o ineffective erythropoiesis reduced hepatocyte uptake o drug interference w/ membrane carrier system o some cases of Gilbert syndrome impaired conjugation o physiologic jaundice of the newborn o breast milk jaundice o genetic deficiency of UGT1A1 activity o Gilbert syndrome o diffuse hepatocellular dz conjugated decreased hepatocellular excretion (deficiency of canalicular membrane transporters) impaired bile flow Hereditary hyperbilirubinemias o unconjugated Crigler-Najjar syndrome type I – hepatic UGT1A1 completely absent; severe jaundice & icterus; fatal w/o surgery type II – UGT1A1 activity greatly reduced; very yellow skin Gilbert syndrome – decreased UGT1A1 activity; mild hyperilirubinemia; o conjugated Dubin-Johnson syndrome – mutation in canalicular multidrug resistance protein 2 (MRP2); impaired biliary excretion; liver darkly pigmented Rotor syndrome – asymptomatic; multiple defects in hepatocellular uptake & excretion of bilirubin pigments Cholestasis - impaired bile formation and flow - extra-hepatic or intrahepatic obstruction of bile channels - defects in hepatocyte bile secretion - clinical: o jaundice, pruritus, skin xanthomas, malabsorption, fat-soluble vitamin deficiency o AP, GGTP - morphology: o accumulation of bile pigment in hepatic parenchyma o feathery degeneration o bile lakes - progressive familial intrahepatic cholestasis o PFIC-1 begins in infancy severe pruritus from high serum bile acid lvls liver failure b4 adulthood o PFIC-2 mutation in hepatocyte cannalicular bile salt export pump (BSEP) severely impaired bile salt secretion into bile extreme pruritus, growth failure, progression to cirrhosis in 1st decade of life risk for cholangiocarcinoma o PFIC-3 cholestasis w/ high serum GGT toxic destruction of biliary tree epithelia Infectious disorders Hepatitis A - benign, self-limited dz - incubation 3-6 weeks - ssRNA, fecal-oral, raw shellfish - never causes chronic liver dz - sporadic febrile dz - vaccine available Hepatitis B - acute hepatitis w/ recovery - incubation 1-4 mo. - partially dsDNA; parenteral, sexual, perinatal - HBV can cause: o nonprogressive chronic hepatitis o progressive chronic dz ending in cirrhosis o fulminant hepatitis w/ massive liver necrosis o asymptomatic carrier state - 10% chronic liver dz - chronic liver dz can cause HCC - vaccine available - highest carrier rate is in perinatally acquired infection - HBV genome codes for: core protein, envelope glycoproteins, polymerase, HBx protein - host immune response is prime determinant of outcome of infection - acute infection: - chronic infection: Hepatitis C - MC chronic blood-borne infection - ssRNA; enveloped; parenteral; intranasal cocaine - incubation 7-8 weeks - 80% of chronic liver dz - MC cause of chronic liver dz in US - MC reason for liver transplant - risk factors: o IV drug use (54%) o multiple sex partners o surgery within last 6 mo. o needle stick injury o multiple contacts w/ HCV-infected person o employment in medical/dental field o unknown (32%) - inherently unstable = multiple genotypes & subtypes; quasispecies in one person (hampered vaccine efforts) - elevated titers of anti-HCV IgG occurring after active infection do not consistently confer effective immunity - characteristic feature of HCV infection = repeated bouts of hepatic damage (result of reactivation of a preexisting infection or emergence of an endogenous, newly mutated strain) - incubation 6-12 weeks - persistent infection & chronic hepatitis are hallmarks of HCV infection - 85% acute infection is asymptomatic - HCV RNA to assess viral replication; RNA persists in many pts with chronic HCV infection - characteristic of chronic HCV infection = episodic elevation in serum aminotransferases, with intervening normal periods - fulminant hepatic failure rare - acute: - chronic: Hepatitis D - circular defective ssRNA - dependent on HBV for life cycle - 2 types: o acute coinfection – HBV established first o superinfection of chronic carrier – may cause severe acute hepatitis o helper-independent latent inf. in liver transplant Hepatitis E - unenveloped ssRNA; fecal-oral; zoonotic - incubation 4-5 weeks - no chronic liver dz - high mortality rate in pregnant women (20%) Hepatitis G - not hepatogropic; doesn’t cause rise in serum aminotransferase - blood and sexual contact - replicates in bone marrow and spleen - no human dz - protective against HIV if coninfects with HIV+ Clinicopathologic syndromes of viral hepatitis - acute asymptomatic hepatitis w/ recovery (serologic evidence only) - acute symptomatic hepatitis w/o recovery (anicteric or icteric) - chronic hepatitis w/ or w/o progression to cirrhosis o MC = HCV o fatigue, spider angiomas, palmar erythema, mild hepatomegaly, hepatic tenderness, mild splenomegaly o younger age at infection = higher chance of chronicity - fulminant hepatitis w/ massive to submassive hepatic necrosis - carrier state Morphology of HBV infected hepatocytes - cytoplasm packed w/ spheres & tubules of HBsAg - ground glass hepatocytes Morphology of HCV infected hepatocytes - lymphoid aggregates within portal tracts - focal lobular regions of hepatocyte macrovesicular steatosis Morphology of acute hepatitis - ballooning degeneration - cholestasis - macrophage aggregates - apoptosis - bridging necrosis - Kupffer cells hypertrophy + hyperplasia - portal tracts infiltrated w/ mix of inflammatory cells - interface hepatitis - ductular rxn Morphology of chronic hepatitis - smoldering hepatocyte apoptosis - lymphoid aggregates - bile duct reactive changes - macrovesicular steatosis (MC in HCV genotype 3 infections) - interface hepatitis - bridging necrosis - deposition of fibrous tissue = hallmark Fulminant hepatic failure - hepatic insufficiency hepatic encephalopathy within 2-3 wks in individuals w/o chronic liver dz - causes: o viral hepatitis (12%) o acetaminophen toxicity o unknown - morphology o HBV induced = massive apoptosis o entire liver or only random areas may be involved o massive loss of mass limp red organ covered by wrinkled capsule o necrotic areas = mushy appearance w/ hemorrhage - survival may cause proliferation & differentiation of stem cell population ductular rxn Other liver infections - TSS – S. aureus - Typhoid fever – Salmonella typhi - Syphilis – T. pallidum - ascending cholangitis - parasitic infections – malaria, schistosomiasis, strongyloidiasis, cryptosporidiosis, leishmaniasis, echinococcosis, liver flukes - liver abscesses o common in developing countries o caused by echinococcal and amebic infections o in developed countries – usually pyogenic o organisms reach liver by: portal vein arterial supply ascending infection in biliary tract direct invasion from nearby source penetrating injury o clinical: fever, RUQ pain, tender hepatomegaly, jaundice Autoimmune hepatitis - chronic & progressive hepatitis of unknown etiology - triggers: o viral infections o drugs (minocycline, atorvastatin, simvastatin, methyldopa, interferons, nitrofuantoin, pemoline) o herbal products (black cohosh) - occurs concurrently w/ other autoimmune disorders o celiac, SLE, RA, thyroiditis, Sjögren, ulcerative colitis - female predominance (young & perimenopausal) - Type 1 (MC) o ANA (anti-nuclear) o SMA (anti-smooth muscle) o AAA (anti-actin) o anti-SLA/LP (soluble liver antigen/liverpancreas antigen) o HLA-DR3 serotype - Type 2 o ALKM-1 (anti-liver kidney microsome) o ACL-1 (anti-liver cytosol) - clusters of plasma cells in the interface of portal tracts and hepatic lobules = characteristic - Tx – immunosuppresives; transplant (recurrence in 22-42%) Drug and toxin-induced liver disease - drug-induced liver injury o 10% of adverse drug rxns o MC cause of fulminant hepatitis in US - injury from: o direct toxicity o hepatic conversion of xenobiotic active toxin o immune mechanisms - acetaminophen = leading cause of drug-induced acute liver failure - antibiotics, isoniazid, non-steroidal analgesics, anti-seizure meds = MC Rx drugs causing idiosyncratic injury - Reye syndrome o mitochondrial dysfunction in liver, brain, and elsewhere o accumulation of fat in hepatocytes (microvesicular steatosis) o aspirin in febrile illness - exposure to a toxin or therapeutic agent should always be included in the ddx of liver dz Alcoholic liver disease - 3 forms of alcoholic liver dz: o hepatic steatosis (fatty liver dz) reversible if abstention from EtOH results from: shunting away from catabolism to lipid biosynthesis impaired assembly and secretion of lipoproteins increased peripheral catabolism of fat microvesicular lipid droplets macrovesicular globules soft yellow greasy organ o alcoholic hepatitis hepatocyte swelling & necrosis mallory bodies neutrophilic rxn fibrosis acetaldehyde (metabolite of EtOH) induces lipid peroxidation & acetaldehyde-protein adduct formation disrupt cytoskeletal & membrane fxn cyt P450 produce ROS malnutrition & vitamin (thiamine) def. release of bacterial endotoxin from gut inflammatory response release of endothelins from sinusoidal endothelial cells decrease in sinusoidal perfusion o cirrhosis final & irreversible form of alcoholic liver dz yellow-tan, fatty, enlarged brown, shrunk, nonfatty scattered larger nodules = hobnail appearance on surface - pathogenesis: o exposure to EtOH causes steatosis, dysfunction of mitochondrial & cellular membranes, hypoxia, and oxidative stress - clinical: o hepatic steatosis – hepatomegaly, mild hyperbilirubinemia & alkaline phosphatase o alcoholic hepatitis – acute symptoms after bout of heavy drinking; malaise, anorexia, weight loss, upper abdominal pain, tender hepatomegaly, hyperbilirubinemia, elevated alkaline phosphatase, neutrophilic leukocytosis; repeated bouts cirrhosis o alcoholic cirrhosis –elevated aminotransferase, hyperbilirubinemia, elevated serum AP, hypoproteinemia, anemia - risk factors: o women more susceptible to hepatic injury but majority of are men o rates higher for African Americans o strong family association o iron overload & infections w/ HCV & HBV increase severity Metabolic liver disease Non-alcoholic fatty liver disease (NAFLD) - MC acquired metabolic disorder - hepatic steatosis in those who don’t drink - MC cause of chronic liver dz in US - NAFLD includes: hepatic steatosis, steatosis accompanied by minor non-specific inflammation, and non-alcoholic steatohepatitis (NASH) - NASH o hepatocyte ballooning o lobular inflammation o steatosis o progressive dz fibrosis o strongly assoc. w/ obesity & metabolic syndrome (dyslipidemia, hyperinsulinemia, insulin resistance) - pathogenesis (two hit model): o (1) hepatic fat accumulation o (2) hepatic oxidative stress - clinical: o serum AST and ALT elevated o AST/ALT ratio <1 o symptoms related to obesity & metabolic syndrome - morphology: o steatosis involves >5% of hepatocytes; droplets of fat (TGs) accumulate in hepatocytes o NASH characterized by steatosis & multifocal parenchymal inflammation (Mallory bodies, ballooning degeneration, apoptosis), fibrosis Hemachromatosis - excessive accumulation of iron deposition in parenchymal organs - abnormal regulation of intestinal absorption of dietary iron - characteristic features: o micronodular cirrhosis (all pts) o DM (75-80%) o skin pigmentation (75-80%) o injury is slow & progressive (5th-6th decade) o males >females - hepcidin – main regulator of iron absorption o encoded by HAMP gene o txn of hepcidin is increased by inflammatory cytokines & iron o txn decreased by iron deficiency, hypoxia, and ineffective erythropoiesis o binds to cellular iron efflux channel ferroportin internalization & proteolysis of the channel prevents iron from intestinal cells & macrophages o hepcidin lowers plasma iron; deficiency causes iron overload o mutations causing lack of hepcidin expression cause hemochromatosis o HFE mutation = MC form of hereditary adult hemochromatosis o HJV mutation = severe juvenile hereditary hemochromatosis - morphology: o deposition of hemosiderin in liver, pancreas, myocardium, pituitary, adrenal, thyroid, parathyroid, joints, skin o cirrhosis o pancreatic fibrosis o liver slightly larger than normal, dense, chocolate brown o biochemical determination of hepatic tissue iron conc. is standard for quantitating hepatic iron content o pancreas – intensely pigmented, diffuse fibrosis, parenchymal atrophy o heart – enlarged, hemosiderin granules, striking brown color o skin – pigmentation due to deposition & increased epidermal melanin production; slate-gray color o joint – hemosiderin deposition in synovial linings; synovitis may develop; may develop pseudo-gout o testes – small and atrophic - clinical: o principally dz of males o classic triad = pigment cirrhosis with hepatomegaly, skin pigmentation, DM o abdominal pain, cardiac dysfunction, atypical arthritis o 200-fold increase in risk of HCC; Tx doesn’t remove risk o removal of excess iron can reverse the toxic changes if cells are not fatally injured Neonatal hemochromatosis - unknown origin - severe liver dz + extrahepatic hemosiderin deposition - not inherited - liver injury begins in utero - no treatment - major function of their protein is inhibition of proteases released from neutrophils - w/o it, emphysema and liver dz develop - cutaneous panniculitis, arterial aneurysm, bronchiectasis, Wegener’s granulomatosis can occur as well - morphology: o presence of round-to-oval cytoplasmic globular inclusions in hepatocytes; acidophilic o PAS positive and diastase resistant - clinical: o neonatal hepatitis w/ cholestatic jaundice in 10-20% of newborns w/ deficiency o HCC develops in 2-3% o in pts with pulmonary dz, smoking avoidance is crucial because it will markedly accelerate emphysema Hemosiderosis - secondary hemochromatosis; parenteral iron overload - ineffective erythropoiesis (severe thalassemia & myeodysplastic syndromes) - excess iron from transfusions + increased absorption - Bantu siderosis – iron overload from ingesting large quantities of alcohol fermented in iron utensils - congenital atransferrinemia - chronic liver dz Neonatal cholestasis - primary conjugated hyperbilirubinemia - 1/2500 live births - major conditions causing it: o cholangiopathies (primary biliary atresia) o neonatal hepatitis - major causes: o bile duct obstruction o neonatal inf. o toxic o metabolic dz o miscellaneous o idiopathic - important to differentiate biliary atresia (needing surgery) - affected infants have jaundice, dark urine, light stools, hepatomegaly - multinucleated giant hepatocytes Wilson disease - AR mutation of ATP7B gene (majority are compound heterozygotes) - impaired copper excretion into bile - failure to incorporate copper into ceruloplasmin - toxic lvls of copper in brain, liver, eye - morphology: o liver – steatosis; acute/chronic hepatitis o brain – basal ganglia (putamen) shows atrophy & cavitation o eyes – Kayser Fleischer rings (green/brown deposits of Cu in Descemet’s membrane in limbus) - clinical: o average age onset = 11.4 years o MC presentation = acute or chronic liver dz o neuropsychiatric symptoms (behavioral changes, frank psychosis, Parkinson-like syndrome – tremor) - in serum ceruloplasmin - in hepatic Cu content (most sensitive & accurate test) - urinary excretion of copper - chelation therapy or zinc-based therapy very successful if recognized early α1-antitrypsin deficiency - AR - very low lvls of α1-antitrypsin Intrahepatic biliary tract disease Secondary biliary cirrhosis - prolonged obstruction of the extrahepatic biliary tree - MC cause = extrahepatic cholelithiasis - other causes = malignancy, strictures - in children = biliary atresia, CF, choledochal cysts, paucity of bile ducts - subtotal obstruction can cause ascending cholangitis (gram neg. enteric organisms) - morphology o end-stage obstructed liver = yellow-green o coarse fibrous septa that subdivide liver in jigsaw-like pattern o proliferation of smaller bile ductules o feathery degeneration o bile lakes Primary biliary cirrhosis - nonsuppurative, inflammatory destruction of medium-sized intrahepatic bile ducts - females > males 6:1 - antimitochondrial antibodies - morphology: o small-duct biliary fibrosis and cirrhosis o dense accumulation of lymphocytes, macrophages, plasma cells, & occasional eosinophils o liver weight is increased becomes decreased - clinical: o fatigue o pruritus o hepatomegaly o hyperpigmentation o eyelid xanthelasmas o arthropathy o increased risk of HCC - extrahepatic manifestations: Sjögren syndrome, systemic sclerosis, thyroiditis, RA, Raynaud’s, membranous GN, celiac - Tx: ursodeoxycholic acid; mechanism unknown, remission and prolonged survival in 25-30% Primary sclerosing cholangitis - inflammation & obliterative fibrosis of intrahepatic & extrahepatic bile ducts, w/ dilation of preserved segments - “beading” of contrast in radiographs of biliary tree - commonly associated with IBD (ulcerative colitis) - atypical p-ANCA found in 80% - onion-skin fibrosis of affected ducts solid cordlike fibrous scars - 7% develop cholangiocarcinoma Anomalies of the biliary trees - Von meyenburg complexes o bile duct hamartomas o common; no clinical significance - Polycystic liver dz o multiple diffuse cystic lesions in liver - Congenital hepatic fibrosis o portal tracts enlarged by irregular, broad bands of collagenous tissue o due to persistence of embryonic form of biliary tree o may develop portal HTN o risk for cholangiocarcinoma - Caroli dz o larger ducts of intrahepatic biliary tree are segmentally dilated o risk for cholangiocarcinoma - all above can be assoc. w/ polycystic kidney dz - Alagille syndrome (paucity of bile ducts) o AD; mutation or deletion of Jagged1 o 5 major clinical features: chronic cholestasis peripheral stenosis of pulmonary a. butterfly-like vertebral arch defects posterior embryotoxon (eye defect) peculiar hypertelic facies Circulatory disorders Impaired blood flow - hepatic a. compromise localized infarct - portal v. obstruction & thrombosis o extrahepatic portal v. obstruction can be caused by: umbilical catheter intra-abdominal sepsis hypercoagulable disorders trauma pancreatitis/pancreatic CA HCC cirrhosis o intrahepatic portal v. radicles may be obstructed by acute thrombosis infarct of Zahn o noncirrhotic portal fibrosis is common in India; presents w/ upper GI bleeding o idiopathic portal HTN has female predominance; presents w/ splenomegaly Impaired intrahepatic blood flow - MC is cirrhosis - sinusoid occlusion can occur in sickle cell, DIC, eclampsia, metastases - R-sided cardiac decompensation = passive congestion of liver enlarged, tense, cyanotic w/ round edges - L-sided cardiac failure/shock = hepatic hypoperfusion centrilobular necrosis - centrilobular hemorrhagic necrosis o hypoperfusion + retrograde congestion o nutmeg liver - peliosis hepatis o primary sinusoid dilation o Bartonella species involved in AIDS assoc. o assoc. w/ CA, TB, AIDS, post-transplant Hepatic vein outflow obstruction - Budd-Chiari syndrome o obstruction of 2+ major hepatic veins o liver swollen & red-purple w/ tense capsule o centrilobular congestion & necrosis - hepatic vein thrombosis is assoc. w/ o 1 myeloproliferative disorders (polycythemia vera) o inherited coagulopathies o antiphosphlipid syndrome o paroxysmal nocturnal hemoglobinuria o intra-abdominal CA (HCC) - obliterative hepatocavopathy o inferior vena cava obstruction at hepatic portion o caused by inferior vena cava thrombosis o endemic in Nepal (assoc. w/ infections) - sinusoidal obstruction syndrome (veno-occlusive disease) o Jamaican bush tea drinkers o occurs primarily following allogenic bone marrow transplant o can occur in CA pts receiving chemo o obliteration of hepatic vein radicles o arises from toxic injury to sinusoidal endothelium slough off wall & embolize downstream, obstructing bloodflow Hepatic complications of organ or bone marrow transplantation Acute graft-vs-host disease - 10-50 days after bone marrow transplantation - donor lymphocytes attack epithelial cells of liver hepatitis Chronic hepatic graft-vs-host disease - >100 days after transplantation - portal tract inflammation, selective bile duct destruction, fibrosis - endothelitis present (subendothelial lymphocytic infiltrate lifts endothelium from BM) Acute rejection of transplanted livers - infiltration of mixed population of inflammatory cells - endothelitis - BANFF scheme – grading scale for severity of rejection Chronic rejection - obliterative arteritis of small & larger arterial vessels (arteriopathy) ischemic changes in liver parenchyma - bile ducts progressively destroyed Hepatic disease associated with pregnancy - viral hepatitis is MC cause of jaundice in pregnancy - HEV inf. runs severe course (10-20% mortality) Preeclampsia/eclampsia - maternal HTN, proteinuria, peripheral edema, coagulation abnormalities, DIC - HELLP syndrome – hemolysis, elevated liver enzymes, low platelets - periportal sinusoids contain fibrin deposits w/ hemorrhage into space of Disse - hepatic hematoma - dissection of blood under Glisson’s capsule may lead to rupture - eclampsia = preeclampsia + hyper-reflexia and convulsions; life-threatening Acute fatty liver of pregnancy (AFLP) - spectrum of mild hepatic dysfunction to hepatic failure, coma, death - present in latter half of pregnancy - primary Tx = termination of pregnancy - fetuses are deficient in mitochondrial long-chain 3hydroxyacyl CoA dehydrogenase metabolites produced by fetus cause hepatic toxicity in mother Intrahepatic cholestasis of pregnancy - onset of pruritus in 3rd trimester, darkening of urine, light stools, jaundice - pruritus extremely distressing for pregnant mother Benign neoplasms Cavernous hemangiomas - MC benign liver tumor - BV tumor - discrete red-blue soft nodules directly beneath capsule Hepatic adenoma - MC occur in women on OC (regress if OC stopped) - may be mistaken for HCC - subcapsular adenomas have tendency to rupture (esp in pregnancy) - may transform into carcinomas (esp. in glycogen storage dz) - mutation in txn factor HNF1α and β-catenin - morphology: o pale, yellow-tan bile-stained nodules o often beneath capsule o well demarcated o steatosis commonly present o no portal tracts Malignant tumors Angiosarcoma of the liver - assoc. w/ vinyl chloride, arsenic, or Thorotras - metastasize widely and kill w/in a year Hepatoblastoma - MC liver tumor of childhood - fatal w/in few years if not treated - epithelial type o made of small polygonal fetal cells or smaller embryonal cells o form acini, tubules, or papillary structures - mixed epithelial & mesenchymal type o contains foci of mesenchymal differentiation - frequent activation of WNT/β-catenin signaling pathway - assoc. w/ FAP and Beckwith-Wiedmann syndrome Hepatocellular carcinoma (HCC) - 3rd most frequent cause of CA deaths - males > females - 4 major etiologic factors: o chronic viral infection (HBV, HCV, 200-fold increased risk for vertical transmission of HBV) o chronic alcoholism o NASH o food contaminants (aflatoxins from A. flavus in peanuts/grains) - tyrosinemia – 40% develop HCC - cirrhosis is prerequisite to emergence of HCC in Western countries - repeated cycles of cell death & regeneration - morphology: o unifocal, multifocal, or diffusely infiltrative o strong propensity for invasion of vascular structures (may be long snakelike mass of tumor invading portal vein or IVC extending into R-side of heart) o satellite nodules - fibrolamellar carcinoma o 5% of HCCs o young male & female adults o no underlying hepatic dz o single large, hard “scirrhous” tumor w/ fibrous bands - clinical: o elevated serum AFP in 50% o death due to cachexia, GI bleed, liver failure w/ coma, rupture of tumor w/ hemorrhage Cholangiocarcinoma (CCA) - 2nd MC hepatic malignant tumor - malignancy of biliary tree outside liver - highest in Hispanics in US - risk factors: o primary sclerosing cholangitis o congenital fibropolycystic dz of biliary system o HCV infection o exposure to Thorotrast o liver fluke (Opisthorchis sinensis) - Extrahepatic form (90% of CCAs) o Klatskin tumors – perihilar; junction of R & L hepatic ducts o periampullary carcinomas are grouped w/ adenocarcinomas of duodenum & pancreatic carcinomas - Intrahepatic form o not usually detected until late in course - morphology: o extrahepatic CCAs small firm gray nodules w/in bile duct wall most are adenocarcinomas Klatskin tumors have slower growth w/ prominent fibrosis o intrahepatic CCAs occur in noncirrhotic liver track along intrahepatic portal tract = treelike tumorous mass extensive intrahepatic metastasis extremely firm & gritty lymph node & hematogenous metastases to lungs, bone (vertebrae), adrenals, brain Metastatic tumors - more common than primary liver cancers - MC = colon, breast, lung, pancreas - multiple nodular metastases w/ striking hepatomegaly - amazing amt of involvement before lab evidence of hepatic dysfunction Biliary tract - 95% of biliary dz attributable to cholelithiasis - 1 liter of bile secreted by liver each day - GB has capacity of 50 ml - not essential for biliary function Biliary tract congenital anomalies - GB absent, duplicated, bilobed or aberrantly located - folded fundus is MC anomaly; creates Phrygian cap - agenesis of all/portion of hepatic or common bile ducts - hypoplastic narrowing of biliary channels (true biliary atresia) Disorders of the gallbladder Cholelithiasis - vast majority silent - 2 main types: cholesterol (90%) & pigment (bilirubin calcium salts) - risk factors: o cholesterol stones northern europeans, N & S Americans, Native Americans advancing age female sex hormones obesity & metabolic syndrome rapid weight reduction gallbladder stasis inborn errors of bile acid metabolism hyperlipidemia syndromes o pigment stones Asians, rural chronic hemolytic syndromes bacterial infection of biliary tree parasitic infestations GI disorders - cholesterol gallstone formation involves 4 simultaneous conditions: o supersaturation of bile o GB hypomotility o cholesterol nucleation (crystallization) o hypersecretion of mucus in gallbladder trap crystals aggregation into stones - morphology: o cholesterol stones pure cholesterol stones = pale yellow, round to ovoid, finely granular hard external surface mostly radiolucent 10-20% cholesterol stones radiopaque o pigment stones black stones in sterile GB bile; 50-75% are radioopaque brown stones in infected intra or extrahepatic ducts; radiolucent - clinical: o biliary pain – excruciating & constant or “colicky” o GB inflammation – painful o complications – empyema, perforation, fistulas, obstructive cholestasis or pancreatitis, gallstone ileus (Bouveret’s syndrome), risk for carcinoma Acute cholecystitis Calculous - precipitated 90% of time by obstruction of neck or cystic duct - results from chemical irritation & inflammation of obstructed GB - protective mucus layer disrupted expose epithelium to bile salts - GB dysmotility develops compromised blood flow to mucosa bacterial contamination may later develop - frequently develops in diabetic pts w/ symptomatic gallstones - clinical: o RUQ or epigastric pain o fever, anorexia, tachycardia, sweating, nausea, vomiting o jaundice = obstruction of common bile duct o leukocytosis, increased serum alkaline phosphatase o symptoms appear w/ remarkable suddenness Acalculous - results from ischemia - cystic artery has no collateral circulation - contributing factors: o inflammation & edema of wall, compromising blood flow o GB stasis o accumulation of microcrystals of cholesterol (biliary sludge), viscous bile, and GB mucus cystic duct obstruction - risk factors: o sepsis w/ hypotension & multisystem organ failure o immunosuppression o major trauma & burns o DM o infections - clinical: o more inisidous than calculous cholecystitis o incidence of gangrene & perforation much higher than calculous Chronic cholecystitis - associated with cholelithiasis in >90% - supersaturation of bile predisposes to inflammation as well as stone formation - microorganisms (E. coli and enterococci) can be cultured from bile in 1/3 of cases - obstruction of GB outflow is not requisite - morphology: o fibrous adhesions o variable degrees of inflammation o Rokitansky-Aschoff sinuses (outpouchings of mucosal epithelium through wall) o porcelain GB (extensive calcification) o xanthogranulomatous cholecystitis (thickened wall) o hydrops of GB (obstructed atrophic GB w/ clear secretions) - clinical: o recurrent attacks of steady or colicky epigastric or RUQ pain o n/v o intolerance for fatty foods - complications: o bacterial superinfection w/ cholangitis or sepsis o GB perforation & local abscess formation o GB rupture w/ diffuse peritonitis o biliary enteric fistula o aggravation of preexisting medical illness o porcelain GB (increased risk of CA) Disorders of extrahepatic bile ducts Choledocholithiasis - presence of stones w/in bile ducts of biliary tree - higher incidence in Asia - may be asymptomatic or cause symptoms: o obstruction o pancreatitis o cholangitis o hepatic abscess o secondary biliary cirrhosis o acute calculous cholecystitis Cholangitis - bacterial infection of bile ducts - MC from choledocholithiasis and biliary strictures - Sphincter of Oddi is MC entry point - ascending cholangitis – infection of intrahepatic biliary radicles; usually enteric gram neg. aerobes (E. coli, Klebsiella, Interococcus, Enterobacter) - presents with fever, chills, abdominal pain, jaundice Biliary atresia - complete or partial obstruction of lumen of extrahepatic biliary tree w/in 3 months of life - 1/3 of infants with neonatal cholestasis - 1:12,000 live births - MC cause of death from liver dz in children - progressive inflammation and fibrosis of intra or extrahepatic bile ducts - 2 forms: o fetal (20%) – commonly assoc. w/ other anomalies (malrotation of viscera, interrupted IVC, polysplenia, congenital heart dz) o perinatal form (MC) – presumed normal tract is destroyed following birth; viral (reovirus, rotavirus, CMV) or autoimmune - Kasai procedure – for type I (common duct) or type II (hepatic bile ducts) - 90% of pts have type III biliary atresia (obstruction at or above porta hepatis) Choledochal cysts - congenital dilations of common bile duct - present most often in children <10 years old - present with jaundice and/or recurrent abdominal pain - predispose to stone formation, stenosis and stricture, pancreatitis, and obstructive biliary complications within liver - risk of bile duct carcinoma in older pts Tumors - derive from epithelium lining of biliary tree - adenomas o benign epithelial tumors o tubular, papillary, or tubulopapillary - inflammatory polyps o sessile mucosal projections with surface stroma infiltrated w/ chronic inflammatory cells and lipid-laden macrophages - adenomyosis of GB o hyperplasia of muscle layer, containing intramural hyperplastic glands Carcinoma of the gallbladder - MC malignancy of extrahepatic biliary tract - women>men; occurs mostly in 7th decade of life - gallstones = most important risk factor - carcinogenic derivatives of bile acids may play role - morphology o infiltrating pattern is MC; poorly defined area of diffuse thickening and induration of GB wall o exophytic pattern growns into lumen as irregular, cauliflower mass while invading underlying wall o MC sites of involvement are fundus and neck; 20% involve lateral walls o most are adenocarcinomas o most invade liver centrifugally at time of discovery; many have extended to cystic duct and adjacent bile ducts and portal-hepatic lymph nodes