Valgus knee injury
advertisement

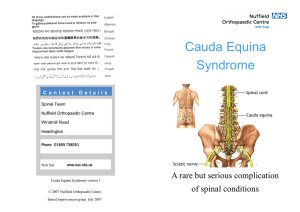
Case Report A 31 years old female presented in 2008 with the chief complaints of lower back pain and right buttock pain, along with difficulty in falling asleep because of the severe pain in the leg with a left sided sciatica. For the past history, she had discectomy in 1998 at L5/S1 with prolonged rehabilitation but returned to work within 12 months. Onset On the physical examination, it was determined that the motor and sensory nerve functions along L5 nerve root was marginally involved with weakness of EHL and a straight leg raising was positive at 30 degrees. MRI confirmed L5/S1 disc protrusion causing L5 nerve root irritation. There was some improvements of the symptom until four days after the surgery, but then the patient complained of a progressive tingling sensation in both legs and difficulties in micturition and defecation with a saddle sensory decrease and a decrease of the anal sphincter tone. She showed some significant weakness in the ankle, and knee weakness with numbness in the left leg. There was decreased anal tone. Repeat MRI mild change in his symptoms several days after the surgery, but he suffered from constant neurogenic pain along with the difficulty in micturition and defecation and he was unable to walk normally because of the weakness and tingling sensation in both legs. Thus, we performed electromyography of the lower extremities and the results showed diffuse bilateral lumbosacral radiculopathies. The 3-phase bone scan showed non- specific findings. However, there was no evidence of focal disc herniation and compression of the thecal sac or nerve root, and the fixation device was in good position according to the contrast enhancement lumbar MRI findings (Fig. 1). We carried out various treatments with taking adhesive arachnoiditis, a battered nerve root or scar adhesion and the psychological compensation from the labor injury into account as the cause of the post-operative syndrome in the lumbar spine. We administered oral corticosteroid (Dexamethasone®; Pacific Pharmaceuticals, Seoul, Korea) due to the neurogenic symptoms for a fixed period, and the patient continued his exercise and physical therapy, and he received medication (anti- inflammatory drugs, analgesics, and gabapentin [Neurontin®; Pfizer, New York, USA]) at the same time. We also administered medication for the difficulty of micturition along with conducting uro-dynamic and bladder examinations at the urology center and we provided psychological consultation and antidepressants at the neuropsychology center. Furthermore, the patient received local injection therapy that included epidural block at the pain clinic, but he did not show any satisfying improvement of the symptoms. DIAGNOSIS; Cauda Equina Syndrome [CES] following post discectomy Pathophysiology of CES In adults, the spinal cord terminates between the T12 and L2 vertebrae, most commonly at the level of the L1 vertebral body. The conus medullaris and is attached to the coccyx by the filum terminale. The conus contains the cell bodies and dendrites of the exiting L5 to S3 nerve roots. The cauda equina is a collection of peripheral nerves (L1 to S5) in a common dural sac within the lumbar spinal canal. Bladder innervation Neurogenic bladder dysfunction is an essential element of CES. Parasympathetic: S2,3,4 [contraction of detrusor and relaxes internal sphincter Sympathetic: hypogastric plexus (T11-L3). Reverse of Parasympathetic Somatic nerves [the pudendal nerve S2,3,4. The external sphincter of the bladder is a striated muscle Pathogenesis The nerve damage in CES may be the result not only of direct mechanical compression but also a secondary, so-called closed compartment syndrome. Rydevik demonstrated that mechanical compression of the nerve roots causes an intraneural edema, which directly causes nerve damage and secondarily results in an increase in intraneural pressure. Clinical 1. Sensation Urinary retention (S2-S4 nerve roots). Measurement of a patient’s post void residual volume provides an accurate assessment of urinary retention. [Kostuik ] Reflexes: Anal wink, Anal tone, look for voluntary anal contraction, bulbocavernous reflex [S1-3] Look for Pinprick sensation Usually they preserve light touch Discussion Bilateral radiculopathy or sciatica are early stages of CES and indicate a high risk of development of advanced CES. Electrophysiological abnormalities and reduced saddle sensation [to prick pin sensation] are indices of early diagnosis. Early CES Patients at the preclinical and early stages have better functional recovery than patients in later stages after surgical decompression.[ Acta Orthopaedica 2010; 81 (3): 391–395] Fully blown CES: CES refers to impairment of the cauda equina and clinically it may manifest as low back pain, saddle anesthesia, bilateral sciatica, motor weakness of the lower extremities, paraplegia, and bowel, bladder, or sexual dysfunction (Byrne 1993). Conversely, patients with extensive nerve damage from severe and prolonged compression (group 4) were not helped by surgical intervention Shia classification [Acta Orthopaedica 2010; 81 (3): 391] Group 1 Low back pain with only BCR (bulbo-cavernosus reflex) and ICR (ischio-cavernosus reflex) abnormalities and no typical symptoms of CES. Group 2 He had slight saddle sensory disturbances and bilateral sciatica. Group 3 Patients had severe saddle sensory disturbances, bowel and/or bladder dysfunction, motor weakness of the lower extremities and reduced sexual function. Group 4 Patients had no saddle sensation, no sexual function, and uncontrolled bowel function. Cauda Equina after Disketomy Incidenc 0.5% Kardaun [J Spinal Disord 1990;3:30–8] have shown a 3.7% over all complication rate after surgical treatment for lumbar disc herniation. Postoperative cauda equina syndrome (CES) ac- counted for 0.5%[J Bone Joint Surg [Am] 1986;68:386 –91]. When to suspect 1, A high index of suspicion is necessary in the postoperative spine patient with back and/or leg pain refractory to analgesia, especially in the setting of urinary retention [J Am Acad Orthop Surg 2008;16:471- 479 ] 2. Bilateral sciatica: early post op period. Look for any changes in the saddle area Causation In lumbar diskectomy, injury to the cauda equina can occur during surgery from direct damage to the nerves, especially from excessive retraction of the dural sac, or postoper- atively as a result of the development of a hematoma or related to dural tear. Common features Henriques [Spine 2001; 26:293-297] reported on five cases of postoperative CES following surgery for lumbar disk herniation. All five patients had a relative spinal stenosis at the involved level. Usual presentation is within 24 hours [1/5 may be seen at 4th day] Neurology is due to ischaemia contributed by venous congestion 4. Postoperative magnetic resonance imaging did not show the cause of the cauda equina syndrome, nor could this be established at the reoperation. Intensity of symptoms: significant bilateral sciatic refractory to analgesics Treatment Most authors seem to agree that the treatment of CES is a wide decompression within 24 hours. References McLaren [Clin Orthop Relat Res 1986;204:143-149] 2. Jensen[Neurosurg Focus 2004;16:E7] Henriques [Spine 2001; 26:293-297] J Bone Joint Surg [Am] 1986;68:386 –91