PAIN IN THE BUTT - Bragg Creek Physiotherapy
advertisement
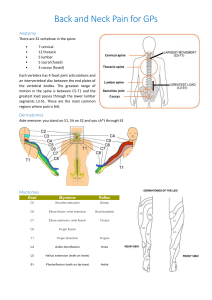
PAIN IN THE BUTT? And down the leg into the foot? Pins and needles, tingling, or numbness? Sciatic pain may be the cause, it typically occurs in the buttock, back or side of the leg and calf and into the foot. Sciatica results from a structure impinging on a lumbar nerve root, resulting in compression and/or inflammation to cause neurological changes in the skin, reflexes and muscles served by the affected nerve. This results in altered sensations, i.e. pain, tingling, numbness. Reflexes can be diminished or absent and the muscles supplied by the specific nerve root become weak. It is not a common syndrome, only that 3-5% of the population suffer from sciatica, however, suffer they will! It can be extremely painful and have a profound impact on function. Aggravating factors are sneezing, coughing, sitting, driving and bending over. Putting on socks and shoes can become a monumental task. Lying down or standing up usually ease the symptoms. It affects men and women equally, with men most susceptible in their forties and women in their fifties. Up to a quarter have symptoms which last more than six weeks and referral to physiotherapists for acute management is routine. The onset of lumbosacral radiculopathy is often sudden with low back pain; any back pain may disappear at the start of the leg pain. Disc prolapse is typically the cause of proper sciatica, however the size of the prolapse is not related to the amount of pain the person suffers. Disc prolapse can result in the internal nuclear material being extruded past the outer disc wall, physically compressing the nerve root which runs nearby. This substance is also chemically irritating to the nerve structure, making the nerve and nearby structures swell, partly blocking the local circulation and the nerve's message transmission. The lumbar discs are more likely to have prolapses due to the high levels of force they have to endure. When we lift things away from the body, bend over at the waist or perform standing activities the back has to cope with the leverage involved. When stresses are loaded onto the discs the hydraulic mechanism magnifies the forces on the outer walls by three to five times that which the skeleton has to cope with. With time these stresses cause failure of the outer disc material and allow prolapses to occur. If the disc prolapse is higher up the pain may be in the front of the thigh and travel no further down the leg than the knee. A patient may have an isolated area of pain and still have a prolapse. “Red flags” are potential warning signs that a person’s back pain could be caused by a medical illness and they need referral to a medical advisor for further investigation. The physiotherapist will ask about weight loss, difficulty passing urine or stools, feeling unwell or having a fever, night pain, poor appetite, a serious past medical history and note whether the patient is younger or older than typical back pain onset age. The physiotherapist will also record the areas of pain, the types of pain reported and the response of pain to postures and activities. A person with lumbar radiculopathy may exhibit abnormal posture, sometimes bent forward and unable to bend backwards, with a one-sided trunk shift. Physiotherapists check the ability to perform spinal movements, any pattern of limitation or tendency for the pain to centralize on repeated movements. Physios will test the reflexes, sensation and muscle power to perform the neurological examination. The McKenzie technique works on pain centralization, the tendency for pain to move towards the back from the legs, suggesting a disc problem, and many physios use this technique. Pain in the front of the thigh and over the knee can be referred from the hip joint, so the physiotherapist will assess the lower limb joints to check the diagnosis. A thorough examination allows the physiotherapist to diagnose the cause of the pain and how to best treat the syndrome, or determine that the individual needs to be referred to a medical practitioner for a consultation and investigation. Physiotherapists use a variety of therapies to treat sciatica, with McKenzie technique being a mainstream technique for discogenic pains. Mobilization and manipulation techniques, core stability work, active release techniques, specific exercises, manual techniques, acupuncture and IMS, soft tissue work and massage are all used in treatment. Patient education on rest and the best position to relieve extreme sciatica pain and advice are instrumental in the healing process. Most individuals recover fully without surgery, and a long term exercise program is useful once the problem has settled. If you have a pain in the butt you would like to get rid of, we can help! Bragg Creek Physiotherapy 403 949 4008 www.braggcreekphysio.com