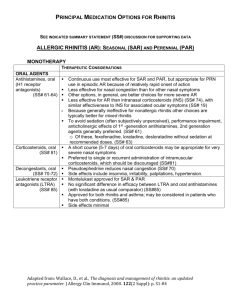
Perennial Allergic Rhinitis
advertisement

Allergic Rhinitis/Conjunctivitis (perennial/non-seasonal) Key Messages Scope Diagnosis and management of perennial (non-seasonal) allergic rhinitis/conjunctivitis. For seasonal allergic rhinitis see separate guidelines. Assessment Signs and Symptoms Bilateral nasal itching, congestion and rhinorrhoea, sneezing, or bilateral conjunctivitis. Ask about triggers (eg pets) if symptoms intermittent all year round (perennial). Differential diagnosis - Seasonal rhinitis (symptoms only in pollen season spring/summer) - Infective rhinosinusitis - Non-allergic (eg hormonal, drug-induced, vasomotor) rhinitis For diagnostic algorithm see http://www.bsaci.org/Guidelines/Algorithm-RhinitisPCGL.pdf Red Flags Unilateral symptoms, polyps, persistent blood stained discharge or persistent purulent discharge – consider referral to ENT. Investigations Send blood for specific IgE to suspect aero-allergen (most commonly house dust mite and pets if exposed). Management 1. Allergen avoidance where possible (eg house dust mite reduction measures or pet avoidance). 2. Mild symptoms should be treated with oral non-sedating antihistamines at doses up to twice BNF maximum dosing (cetirizine 10mg, loratadine 10mg, or fexofenadine 180mg up to twice daily). 3. Moderate-severe symptoms should be treated with intranasal corticosteroid (eg Beconase, two sprays into each nostril twice daily; consider alternative, eg Nasonex or Avamys) in addition to non-sedating antihistamines. Consistent daily use of intranasal use is vital, given maximal effect may not be apparent for at least two weeks. Version: 3 Date last edited: 10/06/15 Locality: Devon wide Amendments by: Kevin Bishop a. Training in appropriate nasal spray technique essential. Guidance is given at http://www.nationalasthma.org.au/uploads/publication/intranasalcorticosteroid-spray-technique.pdf 4. Systemic corticosteroids (in addition to intranasal corticosteroid) at doses of 15-20mg for a maximum of 5 days as a one-off course can be used for severe symptoms uncontrolled on conventional therapy, to control symptoms during important periods (eg exams or other major events). 5. Topical cromoglicate and nedocromil eyedrops are useful to manage allergic conjunctivitis. Consider a concomitant diagnosis of asthma and manage according to guidelines Avoid sedating antihistamines, depot corticosteroids, and chronic use of decongestants. Treatment failure should prompt a review of the diagnosis, compliance with therapy (regular therapy is more effective than “as required” treatment), and intranasal corticosteroid technique. For more information see http://www.guidelines.co.uk/eye_ear_nose_throat_bsaci_rhinitis http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2222.2007.02888.x/pdf Referral Referral Criteria i) Perennial symptoms that are severe and resistant to treatment (when combination treatment at maximum doses has been attempted for at least 3 months). Referral Instructions Red Flags – refer to ENT Refer via DRSS for NEW Devon CCG patients Choose and Book Selection Specialty: ENT Clinic type: Not otherwise specified Service: DRSS- Western – ENT -NEW Devon CCG - 99p Refer to Peninsula Immunology and Allergy Service Refer via DRSS for NEW Devon CCG patients Choose and Book Selection Specialty: Allergy Clinic type: Allergy Service: DRSS- Western –Allergy & Immunology - CCG - 99p Version: 3 Date last edited: 10/06/15 Locality: Devon wide Amendments by: Kevin Bishop Referral forms DRSS Referral form Supporting Information http://www.guidelines.co.uk/eye_ear_nose_throat_bsaci_rhinitis http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2222.2007.02888.x/pdf Evidence Pathway Group This guideline has been signed off by the Western Locality on behalf of NEW Devon CCG. Publication date: June 2015 Review date: May 2017 Version: 3 Date last edited: 10/06/15 Locality: Devon wide Amendments by: Kevin Bishop