Renal Physiology Equations
advertisement

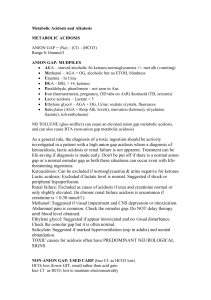
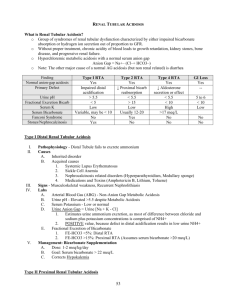
©2010 Mark Tuttle Renal Physiology Equations Name Equation 𝐶𝑋 = Clearance 𝐶𝑋 Units [𝑈]𝑋 ∙ 𝑉 excretion rate = [𝑃]𝑋 serum concentration x is any substance not metabolized by the kidney Comments X is any substance not metabolized by the kidney 𝐶𝐼𝑛𝑢𝑙𝑖𝑛 = 𝐶𝐶𝑟𝑒𝑎𝑡𝑖𝑛𝑖𝑛𝑒 = 𝐺𝐹𝑅 ml/min Cx = Clearance of substance x [U]X = Urine concentration of x V = Urine flow [P]X = Plasma concentration of x Creatinine is filtered (20%), but not reabsorbed or secreted. Actually is secreted in small amounts by PT → overestimates GFR by 10-20% Inulin is filtered, but not reabsorbed/secreted. Filtered Load 𝐹𝐿𝑋 𝐹𝐿𝑋 = 𝐺𝐹𝑅 ⋅ [𝑋]𝑠𝑒𝑟𝑢𝑚 mg Amount of substance X that is filtered through the glomerulus Amount excreted EX EX = amt. filtered + amt. secreted – amt. reabsorbed mg Amount of substance X that is found in the urine Of the filtered amount of X, what ratio is found in the urine. Fractional Excretion 𝐹𝐸𝑋 𝐸𝑋 amount excreted 𝐶𝑋 𝐹𝐸𝑋 = = = 𝐹𝐿𝑋 amount filtered 𝐶𝐼𝑛𝑢𝑙𝑖𝑛 % Determines net reabsorbtion/secretion: 𝐹𝐸𝑋 < 100% → net reabsorption of X 𝐹𝐸𝑋 < 100% → net secretion of X In renal failure (oliguria): 𝐹𝐸𝑁𝑎+ < 1% → Prerenal disease - 𝐹𝐸𝑁𝑎+ > 2% → Acute tubular necrosis Net reabsorption or secretion 𝐹𝐿𝑋 − 𝐸𝑋 mg Excretion Rate 𝐸𝑅𝑋 𝐸𝑅𝑋 = [𝑈]𝑋 ∙ 𝑉 mg/min Rate at which X accumulates in the urine % Normal is 0.2 Filtration Fraction 𝐹𝐹 Renal Plasma Flow 𝑅𝑃𝐹 Renal Blood Flow 𝑅𝐵𝐹 Free-Water Clearance 𝐶𝐻2 𝑂 CockroftGault 𝐺𝐹𝑅 𝑅𝑃𝐹 𝐹𝐹 = 𝑅𝑃𝐹 ≈ 𝐶𝑃𝐴𝐻 𝑅𝐵𝐹 = [𝑈]𝑃𝐴𝐻 ∙ 𝑉 = [𝑃]𝑃𝐴𝐻 𝑅𝑃𝐹 1 − 𝐻𝑒𝑚𝑎𝑡𝑜𝑐𝑟𝑖𝑡 𝐶𝐻2 𝑂 = 𝑉 ∙ 𝐶𝑂𝑠𝑚 𝐶𝐶𝑟 = 𝑈𝑂𝑠𝑚 =𝑉−𝑉 𝑃𝑂𝑠𝑚 𝐴 ⋅ (140 − age)(kg) 72 ⋅ [𝑃]𝐶𝑟𝑒𝑎𝑡𝑖𝑛𝑖𝑛𝑒 PAH is 100%* excreted ml/min ml/min ml/min 𝑝𝐻 = 𝑝𝑘 + 𝑙𝑜𝑔 [𝐴− ] [𝐻𝐶𝑂3− ] = 𝑝𝑘 + 𝑙𝑜𝑔 [𝐻𝐴] 0.03 ⋅ 𝑝𝐶𝑂2 *Underestimates RPF by 10% (because it’s really only 90% excreted) 1 -Hct is fraction of blood volume that is plasma If positive, free water is excreted If negative, free water is reabsorbed Determines if the kidney is concentrating or diluting urine ml/min A=1 for males, 0.85 for females HendersonHasselbalch If positive, there is net reabsorption of X. If negative, there s net secretion of X. - ©2010 Mark Tuttle Fluid Compartment Markers Compartment Substance - D2O - Titrated H2O % Total body weight TBW: Total Body Water ICF: Intracellular Fluid TBW - ECF 40% ECF: Extracellular Fluid - 20% Sulfate Inulin Mannitol 60% ISF: Interstitial Fluid ECF - Plasma - Plasma - - Risa Evans blue Radioactive albumin Normal Serum Levels Substance Normal Range Significance [BUN] 4-8 mmol/L ↑ indicates azotemia BUN:Creatinine 10 > 20:1 → Prerenal azotemia 1:1 → Acute renal failure Blood pH 7.38 – 7.42 Indicates acidosis/alkalosis pCO2 40 mmHg [HCO3-] 24 mEq/L Serum Anion Gap [Na+]-([HCO3-]+[Cl-]) Unmeasured ions include phosphate, citrate, sulfate, and protein. ↑ to replace [HCO3-] ↓in metabolic acidosis 12 mEq/L (8-16 mEq/L) If anion gap is normal in metabolic acidosis, Cl- has likely taken the place of HCO3-, called hyperchloremic metabolic acidosis. Urinary Anion Gap [Na+]+[K+]-[Cl-] Unmeasured ions include ammonium. If anion gap is increased, there is an increase in an unmeasured ion, usually (phosphate, lactate, β-hydroxybutyrate) Near zero or positive In metabolic acidosis, the excretion of the NH4+ (which is excreted with Cl- ) should increase markedly if renal acidification is intact. Because of the rise in urinary Cl- , the urine anion gap which is also called the urinary net charge, becomes negative, ranging from -20 to more than -50 meq/L. The negative value occurs because the Cl- concentration now exceeds the sum total of Na+ and K+. In contrast, if there is an impairment in kidney function resulting in an inability to increase ammonium excretion (i.e. Renal Tubular Acidosis), then Cl- ions will not be increased in the urine and the urine anion gap will not be affected and will be positive or zero.