Reflection Paper NU 608
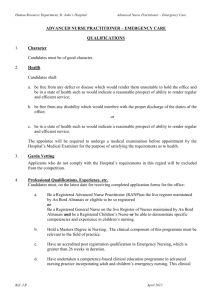
advertisement

Running head: REFLECTION PAPER NU 608 Reflection Paper NU 608 Jennifer Dixon Washburn University NU 608 September 16, 2013 1 REFLECTION PAPER NU 608 2 Reflection Paper NU 608 Incorporating principles of ethical and legal practice in the primary care settings is essential for a nurse practitioner and is also course outcome number seven in NU 608. Ethics are the rules, values, guidelines, or standards governing the conduct of a person or the conduct of the members of a profession and incorporating those guidelines into personal practice as a nurse practitioner. These standards of conduct direct an individual to proper professional conduct concerning the rights and duties of health care professionals and their conduct toward patients, patient’s family members and fellow health care professionals. The American Nurses’ Association has set forth ‘The Code of Ethics for Nurses’ that describes standards of conduct that are to be demonstrated by all nursing professionals and direct their conduct within the profession. Legal practice in the primary care setting is following the legal scope of nurse practitioner practice, or what a nurse practitioner can and can not do. For example, in Kansas nurse practitioners are able to sign workers comp claims, sign handicap parking permits and order physical therapy, but cannot sign a death certificate. Each individual state has a scope of practice that nurse practitioners must follow that identifies what a nurse practitioner can and cannot do in their practice. Incorporating principles of ethical and legal practice in the primary care setting means following these ethical standards and practicing within the legal scope of practice set forth by each state for a nurse practitioner. This course outcome relates to program outcome number one, provide organizational leadership demonstrating knowledge of health policy and health care systems. In order to provide organizational leadership, you have to be incorporating legal and ethical principles into your nurse practitioner practice as well as demonstrating knowledge of health policy and health care systems. True leadership is more than the ability to lead others through authority and power, great leaders lead by inspiring others, REFLECTION PAPER NU 608 3 leading by example and through personal connections. By incorporating principles of ethical and legal practice in the primary care setting you are providing leadership within the organization and demonstrating knowledge of health policy and health care systems. This topic was demonstrated in my specialty practicum by a patient that was being seen for dizziness. This patient was a female in her 30’s that came into the clinic with a history of two days of unexplained dizziness. The patient also reported her lower legs were hurting and her right arm and lower legs were tingling at times with the rest of the review of systems being negative. The patient was very concerned that she may have a blood clot in her arms and legs. We discussed her risk factors for blood clots and she did not have any risk factors so I explained to the patient that is would be highly unlikely that she would have blood clots especially in multiple limbs at the same time. On physical exam, Homan’s sign was negative on both legs and her legs did not appear to be swollen, red, or painful to the touch. The patient had a perfectly normal physical exam and a reason for the dizziness was not discovered in the office. The patient was given meclizine to help control her dizziness and was to follow up in the office in a few days and to call the office immediately if her symptoms got worse. My preceptor and I talked to the patient about possible causes of dizziness and explained to her that we wanted to wait and see how things progressed before ordering something like an MRI of the head since dizziness can gradually subside on its own after such things as an upper respiratory or flulike illness and because her physical exam was completely normal. The next day the patient called the office and was concerned because her legs were still hurting and the patient was still not convinced that she did not have a blood clot. Even though my preceptor was not concerned about a blood clot she ordered a Doppler study to be done anyway because she knew the patient would not feel assured until she had a test done to prove she did not have a blood clot. The REFLECTION PAPER NU 608 4 patient had the Doppler study done and it showed no blood clots just as my preceptor and myself had suspected. Two days later my preceptor saw there was a request for the patient’s medical records from an Internal Medicine Group in town, which meant the patient was seeing someone else about her concerns. There is a fine line between practicing what is though to be good medicine and ordering multiple unnecessary tests for a patient and using your best judgment and conserving resources to keep health care costs low. Some patients may think that a doctor or nurse practitioner is not practicing good medicine because they do not order a panel of unnecessary tests. In this case, is it ethical to go ahead and order a Doppler study at the patient’s request even though the provider does not suspect the condition? It is a hard decision to make especially with medical care being a consumer-based practice where patient’s can shop around until they find a provider to do what they are asking for. What the patient perceives as good medical care and what the provider considers good medical care when using their best judgment and trying to conserve medical resources to keep health care cost low can be two very different things and you have to use your best ethical and medical judgment when making decisions. Another patient, female in the twenties, came into the clinic with a history of depression, anxiety, and ADHD and was requesting a medical note for work stating that she cannot work a certain shift at her current job. The patient was currently working 5:30am-2pm and her employer was wanting to switch her shift to 2:30pm-10pm and she did not want to work this shift because she has a family and would not get to see her family in the evening and she would not be able to find childcare until 10pm every evening. She was requesting that my preceptor sign her work note stating that for medical reasons she has to be off of work by 2:15pm due to her needing to take her medications. In reality she could have worked that shift, but it would have been inconvenient for her to do so. As my preceptor was filling out the form the patient also asked REFLECTION PAPER NU 608 5 that Monday through Friday also be added to the times that she is available to work so that she is not required to work on weekends. In this instance I would have a very hard time signing a medical work release form knowing that the patient is physically able to work the shift even though she does have diagnosed chronic conditions. I feel like the patient was abusing her relationship with her provider and also the medical system to get out of a shift she didn’t want to work. As a soon-to-be nurse practitioner, I would not have felt like I was ethically or legally doing the right things by signing the medical work release form and I do not feel like I would have signed the forms for the patient. I would empathize with the patient’s unfortunate situation but I would not put my own profession on the line or compromise my own ethical beliefs by signing the form for the patient. In the future as a nurse practitioner, I plan to incorporate principles of ethical and legal practice in the primary care setting by practicing in a manner that incorporates ethical, legal and professional standards for advanced nursing practice by serving as an advocate to my patients and by being obligated to demonstrate nonjudgmental and nondiscriminatory attitudes and behaviors towards patients and their families. I plan to promote an ethical practice and base decisions and actions on behalf of patients consistent with the American Nurses’ Association Code of Ethics for Nurses and by acknowledging the dignity, autonomy, cultural beliefs and privacy of all patients. I also plan to provide organizational leadership by promoting an ethical, healthy work environment and demonstrating knowledge of health policy and health care systems.