File - What you Need to Know
advertisement

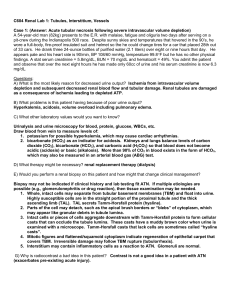
Daryl Apostol Pathophysiology Case Study & Integration Concept Map Assignment Case Study #1 J.H. is a 12-year-old boy diagnosed several months ago with nephrosis following postinfectious glomerulonephritis secondary to an episode of pneumococcal pneumonia. He has been coming to the clinic to have his condition monitored and therapies adjusted as needed. At his latest clinic visit, a decrease in urine output, increasing lethargy, hyperventilation, and generalized edema are noted. Trace amounts of protein are detected in J.H.’s urine by dipstick. Blood is drawn for laboratory analysis, and the results are as follows: pH = 7.36 PaCO2 = 33 mm Hg PaO2 = 100 mm Hg HCO3 – = 18 mEq/L Hct = 30% Na+ = 130 mEq/L K+ = 5.4 mEq/L BUN = 58 mg/dl creatinine = 3.9 mg/dl albumin = 2.0 g/dl Discussion Questions 1. How would a pneumococcal infection lead to glomerulonephritis? How can glomerulonephritis result in nephrosis? (4 points) a) The pneumococcal infection initiates an inflammation process that inflames the glomerulus. b) Glomerulonephritis leads to deposits of mesangial cells that take the place of normal glomerulus cells that become similar in structure to proliferative lesions. Changes in the glomerular wall permeability resulting in larger solvents to pass through into the urine (e.g. protein). 2. Use JH’s laboratory values to determine if he is still experiencing nephrosis or is his condition progressing to renal failure. (4 points) Based on the abnormal lab values: PaCO2, HCO3-, Hct 30%, Na+ 130 mEq/L, K+ 5.4 mEq/L, BUN 58 mg.dl, creatinine 3.9 mg/dl, albumin 2.0 g/dl & traces of protein in urine suggests that pt is experiencing renal failure. 3. What additional physical or laboratory findings would be helpful in determining JH’s degree of renal impairment? (4 points) Lab findings: BUN 58 mg/dl & creatinine 3.9 mg/dl. Physical assessment of decreased urine output leads to patient experiencing edema, increased lethargy due to decreased Hct percentage and hyperventilation (respiratory compensation) from low HCO3- (metabolic acidosis). 4. Draw a concept map depicting how glomerulonephritis can result in nephrotic syndrome. (25 points) Case Study # 2 D.K., a 42-year-old female, is being seen in the clinic for complaints of urinary frequency, urgency, and burning. She reports that her urine appears cloudy and smells abnormal. A urine dipstick reveals leukocyte esterase and is positive for nitrites. D.K. is given a prescription for antibiotics. Discussion Questions 1. What is the most likely cause of D.K.’s signs and symptoms? (4 points) Signs & symptoms of polyuria, urgency & burning, cloudy, + leukocyte esterase & nitrate is + for bacterial infection. 2. What organism is the most common cause of this disorder? (4 points) E. coli is the most common cause of bacterial cystitis. 3. What factors may have predisposed D.K. to the development of this disorder? (4 points) The factors that predisposed patient to cystitis may have been from being female, age, possible poor hygiene, & possible family Hx of UTIs. Case Study #3 P.W. is 23 years old. He was involved in an MVA and has had quite a bit of blood loss due to his injuries. He is brought to the emergency department by ambulance. It is estimated that P.W. has had a blood loss of about 2500 ml. A urinary catheter is inserted to monitor urine output, and fluid resuscitation is initiated while his wounds are cleaned and sutured. The urine output is averaging 15 ml/hr, with a high urine osmolality and low urine sodium. Discussion Questions 1. What type of renal failure is P.W. likely developing? What data support this conclusion? (4 points) a) Patient is experiencing prerenal kidney failure. b) Supporting data is a decrease in circulating volume in the body due to blood loss (hemorrhage) of half his blood volume that decreases renal perfusion urine output of 15 mL. 2. Without adequate therapy, what may develop? Why? What is the best therapy for preventing this from occurring? (4 points) a) Without adequate therapy, hypoxic renal cells will turn into acute tubular necrosis (ATN). b) ATN may develop due to hemorrhaging. In hemorrhage, there is a large amount of blood loss, in this case about half of total body blood volume is lost, therefore causing hypovolemia which causes hypotensio. There is less perfusion within the kidney causing oliguria and ischemia that result in tubular cell death in the kidneys. c) The best therapy for preventing ATN from occurring is address etiology. In this case, stop site of hemorrhage, start blood transfusion and IV fluids to increase perfusion. If pt 2 is taking NSAIDS, ACE inhibitors, or AII blockers, discontinue them. Provide nutrition and monitor for the development of infection. 3. In addition to urine output, what laboratory data should be monitored to assess changes in P.W.’s renal function? (4 points) In addition to urine output, GFR, BUN, creatinine, CBCs (for infection and RBC count), F & E, and urinalysis should be monitored for changes in renal function. 4. If P.W.’s renal function does not return to normal, but continues to be diminished, what are the subsequent stages of his renal disorder and what clinical problems do they present? (4 points) If P.W.’s renal function does not improve it could turn into acute tubular necrosis (ATN). In ATN the pt will encounter 3 phases. The first phase, Prodromal phase, the pt will experience normal or declining urine output and BUN & creatinine levels. The next phase is the oliguric phase; pt will develop oliguria or be nonoliguric. Depending on the severity of the injury, pt may become anuric. Urine output continues to drop, F&E imbalance occurs that result in hypertension & edema & other hypervolemia S&Sx. Protein, casts, WBCs, & RBCs are found in the urine, and eventually uremia. Pt can develop hyperkalemia (fatal) & metabolic acidosis (at the same time). What also may be seen in this phase are anorexia, N/V, weakness, seizures, acidosis, confusion, & coma. The last phase, the postoliguric phase, begins when oliguria has stopped. In this phase of AKI 5% of pts do not recover & is irreversible. Pt will experience polyuria & sodium wasting, & lost of electrolytes in the urine. If no renal function recovery is made after more than 3 months, renal disorder will become chronic and can result in ESRD, the last stage of CKD. Case Study #4 Terry is a 54 y.o. male who was in the other vehicle involved in the MVA with JH. He has also lost a large volume of blood. Upon admission he is lethargic and these are his parameters. B/P 90/50 MAP 63 HR 124 UOP a0-a5 cc/hr BUN 40 Cr. 0.8 1. Based on the information presented what is accounting for Terry’s low UOP? (2 points) a. Urinary obstruction b. Acute glomerulonephritis c. Decreased renal perfusion secondary to hypovolemia d. Acute tubular necrosis (ATN) 2. What does his BUN and Creatinine tell you about his renal function? (2 points) 3 a. b. c. d. He has chronic renal failure He has prerenal acute renal failure He has intrarenal acute renal failure He has postrenal acute renal failure Terry is given a fluid challenge of 500cc NS and 2 units of PRBC’s over the next 3 hours. His B/P is now 118/80; HR 96; and UOP 100cc/hr. 3. What does this response indicate about his renal function? (2 points) a. Intravascular volume was decreased b. Kidney function is normal and able to respond to increased perfusion by increasing UOP c. Post obstructive diuresis d. This is an excessive response because UOP should be 40cc/hr 24 hours later Terry is taken to surgery for internal bleeding. It was determined that he suffered an intraoperative anterior MI. These are his postoperative parameters: Auscultation revealed crackles Irregular and labored respirations B/P 76/48 HR 102 BUN 64 Cr. 6.2 4. What type of renal failure is this? ______________________________ (2 points) 5. The most likely cause of the above type of renal failure in this patient is? (2 points) a. Nephrotoxicity from furosemide b. Renal constriction from norepinephrine c. Diminished cardiac output (remember the most common cause of acute intrarenal failure is untreated acute prerenal failure) d. Toxins from death of myocardial cells 6. Draw a concept map depicting the development of acute prerenal failure in this case. (25 points) See next page Prerenal Kidney Injury Risk Factors/Etiology: Hemorrhage 4 Absolute in circulating volume Hemorrhage Dehydration Burns Relative in circulating volume Distributive shock Hypovolemia Third-spacing & edema cardiac output Cardiogenic shock Dysrhythmias Cardiac temponade Heart failure Myocardial infarction Primary renal hemodynamic abnormalities Occlusion/stenosis of renal artery Drug-induced impairment of renal autoregulation in susceptible persons Diagnostic tests: GFR BUN Creatinine Urinalysis CBCs Chemistry panel, comprehensive Creatinine clearance Na+ reabsorption Low urine Na+ renal perfusion Aldosterone secretion GFR renal hypoxia Renal ischemia (more than few hours) oliguria Acute tubular necrosis (ATN) Treatment: Identify etiology and treat it (e.g. blood transfusion) IV diuretics to address oliguria Diet restrictions (e.g. Na+ intake) Dialysis (if waste products start to build up in body fluid) ria ria 5