6 Month and Annual Assessment Post-HSCT
advertisement

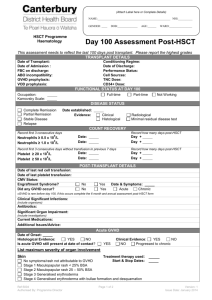
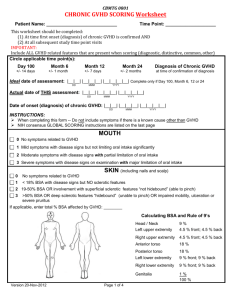
(Attach Label here or Complete Details) NAME:___________________________________________________NHI:__________ GENDER: ____ HSCT Programme Haematology DOB:______________ AGE:______ WARD:________________ 6 Month and Annual Assessment Post-HSCT This assessment needs to reflect the details since the last assessment was completed. Report the highest grades ASSESSMENT DETAILS Date of Transplant: Date of This Assessment: 6 month assessment 4 yr assessment 12 month assessment 5 yr assessment 2 yr assessment other, please state: 3 yr assessment FUNCTIONAL STATUS Occupation: Karnovsky Scale: Full-time Part-time Not Working DISEASE STATUS Complete Remission Partial Remission Stable Disease Relapse Date established: Evidence: Subsequent HSCT since last report? Subsequent DLI since last report? Yes Yes Clinical Histological Radiological Minimal residual disease test Answers to subsequent questions should reflect clinical status immediately prior to start of preparative regime for subsequent HSCT No No COUNT RECOVERY complete this section if patient did not recovery during previous assessment Record first of 3 consecutive days Record how many days post-SCT 9 Date: Date: Neutrophils ≥ 0.5 x 10 /L 9 Neutrophils ≥ 1.0 x 10 /L Day + Day + Record first of 3 consecutive days without transfusion in previous 7 days 9 Date: Date: Platelet ≥ 20 x 10 /L 9 Platelet ≥ 50 x 10 /L Record how many days post-SCT Day + Day + SUBSEQUENT COUNT INFORMATION Following neutrophil recovery, has there been a subsequent decline in 9 neutrophils to < 0.5 x 10 /L for ≥ 3 days since date of last report? Yes No Date of decline: Date of last red cell transfusion: Date of most recent CBC & Diff: Date of last platelet transfusion: POST-TRANSPLANT DETAILS SINCE LAST ASSESSMENT REPORT Were Immunoglobulins Tested? Yes values: Has IVIG been given? Yes No Indications for use: prophylaxis for CMV low IgG (no infection) Other, Were therapies ongoing within 1 month of IVIG? No treatment for CMV RSV infection low IgG (with infection, but not CMV or RSV) Yes No Date of most recent lymphocyte analyses: Chimerism Studies: Yes No Date of Chimerism: CMV Status: Engraftment Syndrome? Yes No Date & Symptoms: Clinical Significant Infections: (include organism) Ref: 5005 Authorised By: Programme Director Page 1 of 5 Version: 1 Issue Date: January 2014 (Attach Label here or Complete Details) Assessment Post-HSCT NAME:___________________________________________________ NHI:__________ GENDER: ____ DOB:______________ AGE:______ WARD:________________ Antibiotics: Significant Organ Impairment: (include investigations) Current Medications: Additional Issues/Advice: GVHD ASSESSMENT Did any GVHD develop or persist since last report? Yes (complete applicable sections below) No Acute GVHD Date of Onset: Histological Evidence: Yes No Clinical Evidence: Is acute GVHD still present at date of contact? Yes No Yes No Progressed to chronic LIST MAXIMUM SEVERITY OF ORGAN INVOLVEMENT Treatment therapy used: Skin Start & Stop Dates: No symptoms/rash not attributable to GVHD Stage 1 Maculopapular rash < 25% BSA Stage 2 Maculopapular rash 25 – 50% BSA Stage 3 Generalised erythroderma Stage 4 Generalised erythroderma with bullae formation and desquamation Gut (lower intestinal tract) Treatment therapy used: Start & Stop Dates: Symptoms not attributable to GVHD Stage 0 No diarrhoea Stage 1 Abdominal pain without significant weight loss (<5%). Diarrhoea ≥ 500ml/day but ≤ 1000ml/ day Stage 2 Mild to moderate weight loss (5-15%) Diarrhoea > 1000ml.day but ≤ 1500ml/day Stage 3 Significant weight loss > 15% Diarrhoea > 1500ml/day Stage 4 Severe abdominal pain with or without ileus Upper Intestinal Tract Treatment therapy used: Start & Stop Dates: Stage 0 No persistent nausea or vomiting Stage 1 Persistent nausea or vomiting Liver Treatment therapy used: No liver acute GVHD / bilirubin level not attributable to acute GVHD Stage 0 Bilirubin < 2.0 mg/dL (< 34 µmol/L) Stage 1 Bilirubin 2.0 – 3.0 mg/dL (34 – 52 µmol/L) Stage 2 Bilirubin 3.1 – 6.0 mg/dL (53 – 103 µmol/L) Stage 3 Bilirubin 6.1 – 15.0 mg/dL (104 – 256 µmol/L) Stage 4 Bilirubin > 15.0 mg/dL (> 256 µmol/L) Other Organ Involvement: Yes No Start & Stop Dates: Organ Involved: Date of Onset: Maximum overall grade (Glucksberg): Grade I (mild) Skin stage 1 or 2 only (no liver or gut aGVHD) Grade II (moderate) Up to stage 1 liver or gut, up to stage 3 skin Grade III (severe) Up to stage 4 liver, up to stage 3 in any other organ Grade IV (life threatening) Stage 4 skin or gut, ECOG/WHO performance status 4 or Karnofsky performance score < 30% Ref: 5005 Authorised By: Programme Director Page 2 of 5 Version:1 Issue Date: January 2014 (Attach Label here or Complete Details) Assessment Post-HSCT NAME:___________________________________________________ NHI:__________ GENDER: ____ DOB:______________ AGE:______ WARD:________________ Chronic GVHD Did chronic GVHD occur? Date of onset: GVHD Grade: Complete section A Organ Involvement: Yes No Progressed from acute GVHD Histological Evidence OR Clinical Evidence Yes No If yes, complete Organ Scoring of GVHD, section B Was specific therapy used to treat chronic GVHD? If so, what was it & when did it start & stop: New Malignancy? Specify Organ: YES Yes No No Date of onset: PHYSICIAN PERFORMING ASSESSEMENT Name: Grade Signed: Date: SECTION A: Overall chronic GVHD grade (NIH) Organ Involvement Mild 1 or 2 organs or sites (except the lung: see below), with no clinically significant functional impairment (maximum of score 1 in all affected organs or sites) Moderate At least 1 organ or site with clinically significant but no major disability (maximum score of 2 in any affected organ or site) 3 or more organs or sites with no clinically significant functional impairment (maximum score of 1 in all affected organs or sites). A lung score of 1 will also be considered moderate chronic GVHD. Severe Score of 3 in any organ or site. A lung score of 2 or greater will also be considered severe chronic GVHD SECTION B: Organ scoring of chronic GVHD Performance Score: KPS ECOG LPS SKIN SCORE 0 SCORE 1 SCORE 2 SCORE 3 Asymptomatic and fully active (ECOG 0; KPS or LPS 100%) Symptomatic, fully ambulatory, restricted only in physically strenuous activity (ECOG 1, KPS or LPS 80–90%) <18% BSA with disease signs but NO sclerotic features Symptomatic, ambulatory, capable of self-care, >50% of waking hours out of bed (ECOG 2, KPS or LPS 60-70%) 19-50% BSA OR involvement with superficial sclerotic features “not hidebound” (able to pinch) Symptomatic, limited self-care, >50% of waking hours in bed (ECOG 3-4, KPS or LPS <60%) No symptoms Clinical features: Maculopapular rash Lichen planus-like features Papulosquamous lesions or ichthyosis Hyperpigmentation Hypopigmentation Keratosis pilaris Erythema Erythroderma Poikiloderma Sclerotic features Pruritus Hair involvement Nail involvement >50% BSA OR deep sclerotic features “hidebound” (unable to pinch) OR impaired mobility, ulceration or sever pruritus %BSA involved: Ref: 5005 Authorised By: Programme Director Page 3 of 5 Version:1 Issue Date: January 2014 (Attach Label here or Complete Details) Assessment Post-HSCT NAME:___________________________________________________ NHI:__________ GENDER: ____ DOB:______________ AGE:______ SCORE 0 WARD:________________ SCORE 1 SCORE 2 SCORE 3 MOUTH No symptoms Mild symptoms with disease signs but not limiting oral intake significantly Severe symptoms with disease signs on examination with major limitation of oral intake EYES No symptoms Mild dry eye symptoms not affecting ADL (requiring eyedrops ≤ 3x per day) OR asymptomatic signs of keratoconjunctivitis sicca Moderate symptoms with disease signs with partial limitation of oral intake Moderate dry eye symptoms partially affecting ADL (requiring drops >3 x per day or punctal plugs), WITHOUT vision impairment GI TRACT No symptoms Symptoms such as dysphagia, anorexia, nausea, vomiting, abdominal pain or diarrhoea without significant weight loss (<5%) Symptoms associated with mild to moderate weight loss (5 - 15%) LIVER Normal LFT LUNGS† No symptoms Elevated Bilirubin, AP*, AST or ALT <2 x ULN Mild symptoms (shortness of breath after climbing one flight of steps) Bilirubin >3 mg/dl or Bilirubin, enzymes 2-5 x ULN Moderate symptoms (shortness of breath after walking on flat ground) FEV1 60-79% OR LFS 3-5 Mild tightness of arms or legs, normal or mild decreased range of motion (ROM) AND not affecting ADL FEV1 40-59% OR LFS 6-9 Tightness of arms or legs OR joint contractures, erythema thought due to fasciitis, moderate decrease ROM AND mild to moderate limitation of ADL Symptomatic with moderate signs on exam AND with mild dyspareunia or discomfort with gynaecologic exam Mean tear test (mm): >10 6 - 10 ≤5 Not done FEV1: DLCO: JOINTS AND FASCIA GENITAL TRACT FEV1 > 80% OR LFS = 2 No symptoms No symptoms Symptomatic with mild signs on exam AND no effect on coitus and minimal discomfort with gynaecologic exam Severe dry eye symptoms significantly affecting ADL (special eyeware to relieve pain) OR unable to work because of ocular symptoms OR loss of vision caused by keratoconjunctivitis sicca Symptoms associated with significant weight loss >15%, requires nutritional supplement for most calorie needs OR oesophageal dilation Bilirubin or enzymes >5 x ULN Severe symptoms (shortness of breath at rest; requiring O2) FEV1 ≤39% OR LFS 10-12 Contractures WITH significant decrease of ROM AND significant limitation of ADL (unable to tie shoes, button shirts, dress self etc) Symptomatic WITH advanced signs (stricture, labial agglutination or severe ulceration) AND severe pain with coitus or inability to insert vaginal speculum OTHER INDICATORS, clinical manifestations or complications related to chronic GVHD check all that apply and assign a score to its severity (0 – 3) based on its functional impact where applicable (none – 0, mild 1, moderate – 2, severe – 3) Oesophageal stricture or web: Pericardial Effusion: Pleural Effusion(s): Ascites (serositis): Nephrotic syndrome: Peripheral Neuropathy: M yasthenia Gravis: Cardiomyopathy: Eosinophilia > 500µl: Polymyositis: Cardiac conduction defects: Coronary artery involvement: Platelets <100,000/µl: Progressive onset: OTHERS: Specify: Ref: 5005 Authorised By: Programme Director Page 4 of 5 Version:1 Issue Date: January 2014 (Attach Label here or Complete Details) NAME:___________________________________________________ NHI:__________ GENDER: ____ DOB:______________ AGE:______ WARD:________________ Assessment Post-HSCT Organ Scoring of chronic GVHD: *AP may be elevated in growing children, and not reflective of liver dysfunction. † Pulmonary scoring should be performed using both the symptom and pulmonary function testing (PFT) scale whenever possible. When discrepancy exists between pulmonary symptom or PFT scores the higher value should be used for final scoring. Scoring using the Lung Function Score (LFS) is preferred, but if DLCO is not available, grading using FEV1 should be used. The LFS is a global assessment of lung function after the diagnosis of bronchiolitis obliterans has already been established. The percent predicated FEV1 and DLCO (adjusted for haematocrit but not alveolar volume) should be converted to a numeric score as follows: >80% = 1; 70-79% = 2; 60-69% = 3; 50-59% = 4; 40-49% = 5; <40% = 6. The LFS = FELV1 score + DLCO score, with a possible range of 2-12. GVHD indicates graft versus host disease; ECOG, Eastern Cooperative Oncology Group; KPS, Karnofsky Performance Status; LPS, Lansky Performance Status; BSA, body surface area; ADL, activities of daily living; LFTs, liver function tests; AP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspirate aminotransferase; ULN, upper limit of normal. Chronic GVHD Risk Score Arora, M., et al. (2011). "Chronic GVHD risk score: a Center for International Blood and Marrow Transplant Research analysis." Blood 117(24): 6714-6720. Risk Factor 0 1 2 Age (years) <29 30-59 >60 Prior acute GVHD None Present Time from transplantation to cGVHD >5 months <5 months <2 mg/dl >2 mg/dl </=34 >34 KPS at cGVHD onset >/=80 <80 Platelet count at cGVHD onset </=100 HLA-identical sibling 7/8 or 8/8 MUD >100 Other related/mismatched MUD Disease status at transplant** Early Intermediate Sex mismatch (donor/recipient) M/M, M/F, F/F F/M Serum bilirubin at cGVHD onset Type of donor Advanced GVHD prophylaxis CSA+MTX+other Tacrolimus+MTX +other or TCD **Early disease = allograft in CR1 (acute leukemia) or first chronic phase (CML) or MDS categories RA or RARS; Intermediate disease = CR2 or later (ALL) or second chronic phase/accelerated phase or later (CML); Advanced disease = patients in relapse or with refractory disease (acute leukemia) or blast crisis (CML) or MDS categories RAEB or RAEB in transformation. Score Risk Group OS (%) NRM (%) 0–2 1 91 4.6 3-6 2 67 20 7-8 3 51 33 9 - 10 4 40 43 11 5 21 63 >12 >11 6 5+6 4 14.5 72 67 This prognostic scoring system for chronic graft versus host disease (cGVHD) was published by the Center for International Blood and Marrow Transplant Research (CIBMTR) in 2011.1 It derives from a multivariate analysis of survival of 5343 patients who underwent allogeneic stem cell transplantation from a related or unrelated donor (including umbilical cord blood) for AML, ALL, CML, or MDS between 1995 and 2004, and who were diagnosed with cGVHD within 1 year of transplantation. References: www.bloodref.com Ref: 5005 Authorised By: Programme Director Page 5 of 5 Version:1 Issue Date: January 2014