Pegfilgrastim for stem cell mobilisation
advertisement

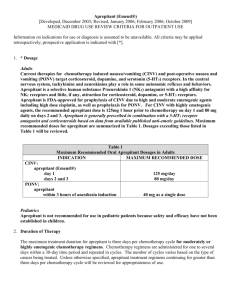
Developments in supportive care of the haematology patient Nick Duncan Haematology pharmacist QE Hospital, Birmingham Outline of session Stem cell stimulation Anti-infectives Plerixafor Pegfilgrastim Maribavir Symptom control Aprepitant Palifermin New agents for GVHD Stem cell stimulation Current Mobilization Strategies for Autologous Haematopoietic Stem Cell Transplantation Growth factor alone - Filgrastim, Lenograstim Growth factor + Chemotherapy No agreed front-line choice – current failure rate 15-20% Consequences of Sub-optimal Mobilisation Failure to mobilise a sufficient number of CD34+ cells may result in: Increased number of days of apheresis Need for bone marrow harvest Ineligibility for transplantation Additional burden on patients Use of sub-optimal apheresis product may lead to: Delayed, partial, or failed stem cell engraftment Potential for increased risk of opportunistic infections and/or bleeding Limitations of Salvage Mobilisation Strategies Strategy Complications Repeat Mobilization High product volume when combined with previous collection Higher cost & morbidity Associated with high failure rate Alternative Cytokines Higher dose of G-CSF Combine G-CSF with GM-CSF Associated with added toxicity or lack of efficacy Addition of Chemotherapy Toxicity, neutropenic fever, admission costs Traditional Bone Marrow Harvest Slower engraftment Increased cost, risk (due to anesthesia) and pain for patient Plerixafor Recently approved by EMEA In combination with G-CSF to enhance mobilisation of haematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation in patients with lymphoma and multiple myeloma whose cells mobilise poorly. Novel mechanism of action A CXCR4 receptor antagonist Mechanism of Action of Plerixafor stem cell CXCR4 SDF-1a bone marrow SDF-1a and CXCR4 play key regulatory roles in stem cell trafficking to, and retention by the bone marrow. Plerixafor blocks the CXCR4SDF-1a interaction, releasing stem cells from the bone marrow into the circulating blood Lapidot T and Petit I. Exp Hematol. 2002;30:973 Kaplan-Meier estimate of proportion of patients reaching ≥ 5 × 106 CD34+ cells/kg NHL Patients (%) achieving ≥ 5 million CD34+ cells/kg by apheresis day HR = 3.64, 95%CI (2.39, 5.45), P < 0.0001 65.6% 70 57.7% 60 50 40 Plerixafor + G-CSF 49.1% 27.9% 30 21.6% 20 14.2% 10 24.2% Placebo + G-CSF 4.2% 0 1 2 3 4 Apheresis Day DiPersio JF et al JCO 2009; Epub ahead of print Myeloma patients (%) achieving ≥ 6 x 106 CD34+ Cells/kg by apheresis day Kaplan-Meier Estimate of Proportion of Patients Reaching ≥ 6 x 106 CD34+ cells/kg HR = 2.54, P < .0001 100 86.8 90 Plerixafor + G-CSF 77.9 80 70 86.8 54.2 56.0 60 49.0 50 Placebo + G-CSF 35.3 40 17.3 30 20 10 0 1 2 3 4 Apheresis Day DiPersio JF et al Blood 2009; 113: 5720-5726 Transplant Outcomes: Number of Days to Neutrophil & Platelet Engraftment PLERIXAFOR PLACEBO Median time to neutrophil engraftment (days) NHL: 10 Myeloma: 11 NHL: 10 Myeloma: 11 Median time to platelet engraftment (days) NHL: 20 Myeloma: 18 NHL: 20 Myeloma: 18 DiPersio JF et al JCO 2009; Epub ahead of print DiPersio JF et al Blood 2009; 113: 5720-5726 Safety of Plerixafor – myeloma study DiPersio JF et al Blood 2009; 113: 5720-5726 Plerixafor – practical issues Which patients to target? Needs to be given 6-11 hours pre-apheresis Admission required? Recommended to be given at a dose of 0.24mg/kg/day for 2-4 days Costs £4,900 + VAT for a 24mg vial Pegfilgrastim Currently licensed for FNE prophylaxis post conventional chemotherapy. Interest in using it for: PBSC mobilisation Post SCT Pegfilgrastim for stem cell mobilisation Has been used alone (usually 12mg) or postchemo (usually 6mg) for autologous stem cell mobilisation in myeloma and lymphoma patients Appears comparable to conventional G-CSF but studies all small Pegfilgrastim mobilised stem cells may result in faster count recovery – Tricot G et al. Haematologica 2008; 93: 1739-42 Pegfilgrastim post SCT Number of small studies in autologous SCT comparing pegfilgrastim (6mg on d+1 or d+5) with conventional G-CSF. Equivalence demonstrated wrt count recovery Some studies demonstrated superiority wrt incidence and duration of FN - (e.g. Martino M et al. Eur J Haematol 2006; 77: 410-5) One fully published study in allograft recipients – Ocheni S et al. Leuk Lymphoma 2009; 50: 612-8 Neutrophil recovery slightly faster (15 vs 16 days) with pegfilgrastim vs lenograstim No difference wrt incidence and duration of FN. In conclusion, drug cost likely to impact on choice of agent Anti-infectives CMV infection CMV reactivation a major issue post allogeneic SCT Pre-emptive ganciclovir mainstay of management but toxicity concerns Lack of gold-standard prophylaxis – aciclovir, valaciclovir, ganciclovir? Interest in new agents Maribavir (1) Maribavir is an oral agent with anti-CMV activity Inhibits viral DNA assembly and egress of viral particles from infected cells Favourable toxicity profile – no renal or BM effects Interest in using for CMV prophylaxis Promising data published 2008 Maribavir (2) Winston et al. Blood 2008; 111:5403 111 allograft recipients randomised to maribavir (200-800mg/day) or placebo At 100 days incidence of CMV infection was 15-19% vs. 39% Significant reduction in need for pre-emptive ganciclovir Toxicity – N+V, taste disturbances Maribavir (3) Large phase III trial (681 patients) not yet published but results released earlier this year Maribavir prophylaxis (100mg bd) failed to meet 1ry and 2ry endpoints vs. placebo: Rate of CMV disease: 4.4% vs. 4.8% Need for anti-CMV therapies: 38% vs. 40.5% GVHD incidence and mortality comparable Not sure what the future holds for this drug……. Symptom control Aprepitant An oral neurokinin-1 antagonist Licensed for prevention of N+V associated with moderately and highly emetogenic chemo (+5HT3 antagonist and corticosteroid) Increasingly used in oncology High-dose chemotherapy is highly emetogenic so should we be using aprepitant in haematology? What do the guidelines say? ESMO guidelines 2008 Highly emetogenic chemo 5-HT3 antagonist + steroid + aprepitant to prevent acute N+V. Steroid + aprepitant to prevent delayed N+V NCCN guidelines 2008 As per ESMO for highly emetogenic chemo. An option for some patients receiving moderately emetogenic chemo. TBI - 5-HT3 antagonist + steroid For multiple-day chemotherapy advises that can give aprepitant 125mg day 1 then 80mg days 2-5. What do the guidelines say? ASCO guidelines 2006 As per ESMO for highly emetogenic chemo Consider aprepitant with high-dose chemo although lack of evidence in this group Any data in haematology patients? Bubalo JS et al. ASCO 2007, abstract 9112 30 patients receiving Cyclo/TBI or Bu/Cy allograft Randomised to aprepitant or placebo (plus ondansetron +/- dex) Received aprepitant from d-7 to d+4 Complete or major response rate: 14/15 vs 7/15 (p=0.014) No emesis seen in 10/15 vs. 5/15 (p = ns) No difference wrt cyclophosphamide kinetics or toxicity Any data in haematology patients? Aprepitant (3/7) + ondansetron in 5 patients receiving Bu/Cy. No vomiting and 2 patients had 1 episode of nausea. Mittaine et al. EBMT 2007, Abstract 1026 Domingues et al. EBMT 2008, Abstract 1235 Domingues et al. EBMT 2009, Abstract 1202 Aprepitant (days -5, -2, +1) + ondansetron in 8 patients receiving BEAM. Concluded that highly effective. Current issues with aprepitant Lack of data in BMT population but may be worth considering How to deal with multiple-day chemotherapy Little use of cisplatin in haematology Can it replace dexamethasone? Cost issues…… Cost issues 18 16 14 12 10 8 6 4 2 0 rid o ne e pe om D lo p ra m id ne so oc M et ex a m an D et ha se tro O nd ni se G ra ita pr ep A tro n n Cost/day (£) nt Cost (£) Comparative costs of antiemetics (BNF 2008) Data misleading due to NHS contract prices for 5-HT3 antagonists – large differential between aprepitant and other agents Mucositis as a complication of SCT Incidence of mucositis with SCT conditioning regimens 70-80% Consequences include pain, infection risk, inadequate nutrition, prolonged hospitalisation Management mainly supportive Now have option of palifermin (recombinant human keratinocyte growth factor) Benefits of palifermin Pivotal trial – Spielberger R et al. NEngl J Med 2004; 351: 2590-8 212 autograft patients receiving high dose chemo + TBI randomised to palifermin (60mcg/kg) or placebo Incidence of mucositis (grade 4) – 20% vs 62% (p<0.001) Duration of mucositis (grade 3/4) – 3 vs 9 days (p<0.001) Significant reduction in opioid and TPN requirements Recent allograft study reported similar findings Langer et al. BMT 2008; 42: 275-9 Can palifermin influence GVHD Prevention of GI injury important in minimising aGVHD Animal models demonstrated benefits of palifermin in incidence and severity of GVHD Blazer B et al. Blood 2006; 108: 3216-22 Palifermin vs. placebo in 100 allograft recipients No difference wrt GVHD, relapse or survival Longer follow up failed to demonstrate any differences between arms (Levine et al. Biol Blood Marrow Transplant 2008; 14: 1017-21) Is there a role for palifermin? Trial data is reasonably strong but……….. The drug is very expensive - >£700/dose Practice at QEH has been to give it to private patients undergoing SCT. About 25 patients treated to date Collected data on first 13 patients and demonstrated no clear benefits compared to matched control-group (Khan, Duncan BOPA 2007). Lower-risk population? Majority of patients developed a rash Conclusion - may have a role with TBI-based schedules but too expensive for routine use Management of GVHD GVHD is the most frequent complication after allogeneic SCT. Steroids the mainstay of treatment but steroid refractory GVHD has a mortality of 70% so need for effective 2nd line/alternative therapies Lots of treatment options……. ATG, alemtuzumab, daclizumab,etanercept, infliximab, pentostatin, MMF, budesonide, ECP, thalidomide, imatinib, rituximab Recent trials in GVHDbudesonide Andree H et al. BMT 2008; 42: 541-6 13 patients with cGVHD affecting the gut Some had received systemic steroid previously Received budesonide 3mg tds for median 5/12 7 patients achieved CR and 1 PR. Consider as alternative to systemic steroid in mildmoderate cGVHD but caution re recurrence when treatment stopped. Also shown efficacy in combination with systemic steroids in aGVHD of the gut – Bertz H et al. BMT 1999; 24: 1185-9 Recent trials in GVHD imatinib Magro L et al. BMT 2008; 42: 757-60 Sclerodermatous cGVHD historically difficult to treat – incidence of about 11% Imatinib’s inihibition of PDGF and TGF pathways may be of benefit – inhibits fibroblasts growth and collagen production 2 patients with refractory sclerodermatous GVHD treated with imatinib 400mg/day Both had very good response with no tolerability issues AT QEH, one patient with severe ocular cGVHD received imatinib for relapsed CML. GVHD improved dramatically. Recent trials in GVHD – antiTNF agents (1) Infliximab drug of choice at QEH for steroidrefractory gut aGVHD – Italian study showed 59% RR in 32 patients (mainly gut +/liverGVHD) – Patriarca F et al. Haematologica 2004; 89: 1352 Potential issues: 72% developed infection and 2 responding patients died of fungal infection 10mg/kg/week for 4 weeks - £13,500 for 70kg patient Recent trials in GVHD – antiTNF agents (2) Etanercept has also shown promise against GVHD. Busca A et al. Am J Haematol 2007; 82: 45-52 21 patients with steroid-refractory GVHD 52% RR (64% in gut GVHD) High-rate of CMV reactivation and bacterial and fungal infection Also been used 1st line (+ steroids) - 69% CR rate vs 33% with steroid alone – Levine J et al. Blood 2008; 111: 2470-2475 25mg SC bw for 4/52, then weekly for 4/52 cost = £1200. Conclusions A number of interesting and novel recent developments in supportive care Concerns: Affordability Quality of the trial data especially in setting of GVHD