Treatment of severe acute Graft-versus-Host Disease with
advertisement

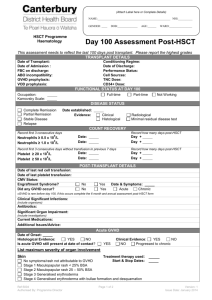
Supplemental Information History of the patient A 22-year old female patient received a first allogeneic stem cell transplantation (AlloSCT) at the age of 13 due to a myelodysplastic syndrome with peripheral blood stem cells (PBSC) from a HLA-identical female donor. After the first AlloSCT she developed moderate mucosal GvHD but recovered hematologically with full donor chimerism. When she was 20, a secondary acute myeloid leukemia was diagnosed. Therefore, a second AlloSCT with PBSC from a HLAidentical male donor following conditioning with hyper-fractionated total body irradiation with 12 Gy and cyclophosphamide was performed. GvHD prophylaxis was standard cyclosporine (CSP) and a short course of methotrexate. The patient suffered a hyperacute GvHD of the skin with general erythema and bullae, grade IV, which initially responded sufficiently to high-dose steroid-therapy. Thus, the patient was discharged with a dual immunosuppression of CSP and steroids. Unfortunately, the GvHD worsened after discharge and the patient had to be admitted to hospital again 2 months after AlloSCT with exacerbated skin GvHD and severe intestinal involvement. She had therapy-refractory nausea and vomiting, abdominal cramping and diarrhea volumes reached up to five liters/day. The intestinal GvHD was repeatedly documented by endoscopy and histological examination. There was no hepatic GvHD involvement. The severe GvHD did not respond to a number of immunosuppressive lines. Immediately upon re-admission the patient received high-dose steroids (5 mg/kg body weight [BW]) with no improvement. Therefore, a course of anti-thymocyte globuline (10 mg/kg BW) was applied over five days, which also did not lead to a response. Then, mycophenolate mofetil (MMF) and subsequently tacrolimus were added. Since in some colon biopsies HHV-6, adenovirus and EBV DNA were detectable, a therapy course with cidofovir was initiated. Unfortunately, all these 1 measures did not lead to a relief in GvHD symptoms. Therefore, a course of infliximab (10 mg/kg BW once per week over a four week period) was administered and 19 sessions of extracorporeal photopheresis were performed over four months. Throughout this time the basic immunosuppression with steroids, mostly in combination with either tacrolimus or MMF, was continued. A therapy attempt with sirolimus had to be discontinued due to increasing renal insufficiency (a synopsis of immunosuppressive therapy is depicted in Figure S1). Given the history of this therapy-refractory GvHD, we discussed in depth with the patient the possibility of an experimental approach to control the GvHD. A concept for an individual treatment attempt with MSC exosomes was developed and approved by the Legal Department of the University Hospital Essen, Germany. The patient agreed to the proposed treatment and gave her written consent. Isolation and expansion of primary human mesenchymal stem cells Human bone marrow (BM) was obtained from unrelated donors after informed consent according to the Declaration of Helsinki. Primary human MSCs were raised from mononuclear cells obtained by Ficoll (Biocoll Separating Solution, Biochrom AG, Berlin, Germany) density gradient centrifugation of bone marrow. The mononuclear cells were cultured in tissue culture 6well plates at a density of 2 x 106 cells per well in MSC basal media (Pan Biotech, Aidenbach, Germany) supplemented with 5% human thrombocyte lysate, 1% glutamine, and 1% penicillinstreptomycin (Invitrogen, Darmstadt, Germany) for 24 hours. After 24 hours non-adherent cells were removed by medium exchanges. After confluence had been reached, usually within 14 days, cells were continuously passaged after treatment with 0.25% Trypsin. Obtained MSCs were characterized flow cytometrically, their osteogenic and adipogenic differentiation potential was confirmed in vitro. 2 Collection of MSC conditioned media Starting at passage 3, MSC conditioned media (CM) were harvested every 48 hours and passed through a 0.22 µm filter membrane (TPP, Trasadingen, Switzerland) to remove cell debris and larger vesicles. CM were collected and stored at -20°C. After thawing CM were unified. 3 units/mL of heparin (Ratiopharm, Ulm, Germany) and 3 µg/mL Actilyse (Boehringer Ingelheim, Ingelheim, Germany) were added. Supernatants were incubated for 3 hours at 37°C and then filtered through 0.22 µm bottle top filters (TPP). PEG-precipitation of exosomes from conditioned media of BM-MSCs Exosomes were concentrated applying a polyethylene-glycol (PEG)-based purification strategy. PEG 6000 (Sigma-Aldrich) and NaCl were added to filtered MSC supernatants to a final concentration of 10% PEG 6000 (v/v) and 75 mM NaCl, respectively. Following incubation for 8-12 hours at 4°C, exosomes were precipitated and collected by centrifugation for 30 min at 1,500 g. The obtained pellets were resolved in 1 mL 0.9% NaCl (B. Braun Melsungen, Melsungen, Germany), washed in a total volume of 45 mL 0.9% NaCl for 12 h at 4°C and precipitated by ultracentrifugation for 2 hours at 100,000 g. The pellets were once again resolved in 1 mL 0.9% NaCl and diluted with 0.9% NaCl to the applied working solutions. Working solutions were stored as 1 mL aliquots at -80°C until usage. Microbiological, virological and toxicological analyses of the applied exosome preparation A 1:5 diluted sample of the exosome preparation was tested for bacterial contamination at the Institute of Medical Microbiology (University Hospital Essen) and analyzed for infectivity via PCR and infectious serology. The endotoxin concentration of the preparation was tested by the Acila AG (Mörfelden-Walldorf, Germany). 3 Nano particle tracking analysis (NTA) NTA was performed by using the NanoSight® (NanoSight, Minton Park, GB) and the ZetaView® (Particle Metrix, Meerbusch, Germany). Both these instruments track the Brownian motion of laser beam illuminated particles over time and subsequently calculate particle sizes and concentrations. As described previously, 1:500 or 1:1000 H2O diluted probes were measured in triplicates (NanoSight®) and duplicates (ZetaView®) 1. Western Blot analyses Protein concentrations of obtained aliquots were determined by the micro BCA assay (Thermo Fisher Scientific, Schwerte, Germany). To perform Western Blots 5 µg of the concentrated exosomes were treated with sample buffer (DTT, 0.1% SDS, 0.1 M Tris HCl, pH 7.0) and boiled for 5 min at 95°C. Samples were separated on 12% SDS-PAGE gels and transferred to PVDF membranes (Merck Millipore, Darmstadt, Germany). Membranes were blocked for 1 hour in 5% skimmed milk (Sigma-Aldrich) and phosphate buffered saline (PBS) and incubated with antibodies either recognizing the exosomal marker proteins Tsg101 (Sigma-Aldrich) or CD81 (BD). For the detection of bound antibodies corresponding HRP-conjugated secondary antibodies (Dianova, Hamburg, Germany) were used. HRP activities were visualized by enhanced chemiluminescence (Thermo Fisher Scientific). Peripheral blood samples Peripheral blood mononuclear cells (PBMCs) and Heparin plasma samples were procured from the GvHD patient before, during and after the MSC-exosome therapy. PBMCs were isolated from the samples by Ficoll density gradient centrifugation (Invitrogen, Darmstadt, Germany) and cryopreserved at -80°C until usage. 4 Determination of Cytokines and HLA-G ELISA technology was used to estimate the amount of soluble HLA-G (sHLA-G), cytokines and apoptosis-inducing molecules in the exosome preparations and in patient’s Heparin plasma samples obtained before, during and after the exosome therapy. Before the various ELISA formats were performed, enriched exosomes (100 µg/mL) were solubilized in 1 mL PBS-Tween (1%) and sonicated for 60 sec; plasma samples were analyzed undiluted. sHLA-G concentrations were determined as described previously 2 with minor modifications: The monoclonal antibody (mAb) G233 (Exbio, Praha, Czech Republic) was used as the capture reagent, and bound sHLAG was detected by the biotinylated mAb w6/32 (Leinco Technologies, St. Louis, Missouri, USA) followed by AMDEX™ Streptavidin HRP (Amersham, Freiburg, Germany). The detection limit of sHLA-G ELISA was 0.1 ng/mL. Concentrations of pro-inflammatory (IFN-γ, TNF-α, IL-1b, IL-2, IL-6, IL-8, IL-17a, IL-21), anti-inflammatory (IL-1RA, IL-4, IL-10, IL-13, TGF-1) and apoptosis-inducing molecules (soluble FasL) were determined according to the manufacturers’ protocols (eBioscience, Frankfurt, Germany or BD Biosciences, San Jose, CA, USA). The assay sensitivities ranged between 2.0 and 20 pg per mL. Determination of the IL-1β, TNF-α and IFN-γ cytokine reactivity profile by ELISpot After thawing PBMCs, NK cells were isolated by negative selection (Invitrogen). PBMCs and NK cells were adjusted to concentrations of 1 x 106 cells per mL and used as effector cells. To analyze impacts of MSC-exosomes on cytokine responses, 1 x 106 effector cells were mixed with 100 µg MSC-exosome preparations. Effector cell suspensions with and without exosomes were used in cytokine stimulation experiments. HLA-E*01:03 or HLA-B27 stably transfected K562 cells and cells of the parental HLA class I negative K562 leukemic cell line were used as allogeneic stimulator cells at densities of 1 x 105 cells per mL. ELISpot assays were performed in 5 an effector to stimulator range of 6:1. For IL-1β and TNF-α ELISpot assays 1.25 x 105 effector cells and 2,500 stimulator cells were used, for IFN- ELISpot assays 7.5 x 105 effector cells and 1.5 x 104 stimulator cells. Cells were seeded in 200 µL culture medium supplemented with 200 U/mL IL-2 and 10% fetal calf serum onto MultiScreen-HA ELISpot plates (MAIPS4510, Merck Millipore) pre-coated with corresponding capture antibodies of the ELISpot kit (eBioscience, Frankfurt, Germany). Effector cells without stimulator cells and stimulator cells without effector cells served as controls. Each stimulation condition was performed in duplicate. After 24 hours incubation at 37°C in 5% CO2 atmosphere, the numbers of cytokine producing effector cells were estimated according to the manufacturer’s protocol. Spots were enumerated by the ELISpot reader AID ELISpot Reader Systems (Autoimmun Diagnostika, Strassberg, Germany) using AID ELISpot Software Version 6. Statistics The D’Agostino-Pearson omnibus normality test was applied to assess the Gaussian distribution of individual data sets. In relation to that, the results of mixed lymphocyte reaction assays were analyzed by the Mann-Whitney U test. The comparison of the cytokine response of the patient derived PBMCs harvested before, during and after the exosome therapy was performed with the Kruskal Wallis test. Statistical analyses were performed with GraphPad Prism version VI. Overall, a 5% or lower p-value was considered to be statistically significant; only such p-values are indicated within the text. 6 Supplemental Figure Legends Figure S1 Treatment regime of the 22-year old female GvHD patient following allogeneic stem cell transplantation. ATG: anti-thymocyte globuline, MMF: mycophenolate mofetil, ECP: extra corporal photophoresis. 7 Figure S2 Analyses of the MSC exosome preparations. (A) Western Blot analyses of the MSC exosome preparations for the exosomal marker proteins TSG101 and CD81 (5 µg protein lane). (B) Size distribution of nanoparticles within the MSC exosome preparations (MSC1 Exo and MSC3 Exo were used as representatives and measured on the NanoSight® platform). (C) Electron microscopic analyses of exosome preparations (MSC1 Exo and MSC3 Exo were used as representatives; scalbare 100 nm). 8 1. Sokolova V, Ludwig AK, Hornung S, Rotan O, Horn PA, Epple M, et al. Characterisation of exosomes derived from human cells by nanoparticle tracking analysis and scanning electron microscopy. Colloids Surf B Biointerfaces 2011 Oct 1; 87(1): 146-150. 2. Schutt P, Schutt B, Switala M, Bauer S, Stamatis G, Opalka B, et al. Prognostic relevance of soluble human leukocyte antigen-G and total human leukocyte antigen class I molecules in lung cancer patients. Hum Immunol 2010 May; 71(5): 489-495. 9