Immunosuppression in Bone Marrow Transplant
advertisement

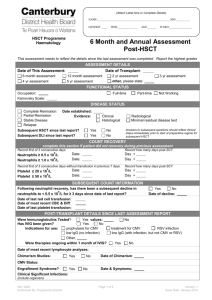
Objectives Summarize the principles for use of immunosuppression in allogeneic stem cell transplant (SCT) Compare and contrast commonly used medications used for immunosuppression Describe monitoring parameters and common adverse effects associated with immunosuppression Immunosuppression in Bone Marrow Transplant Ashley Newland, PharmD Hematology/Oncology Pharmacist Specialist VCU Medical Center November 8, 2011 Cells of the Immune System http://www.rikenresearch.riken.jp/eng/frontline/5028 Use of Immunosuppression Allogeneic stem cell transplant Prevention of rejection Prevention of graft versus host disease (GVHD) Component of conditioning regimen Eradicates host T-cells to allow acceptance of donor cells Pre- & post-transplant medications Suppresses donor T-cells to minimize recognition of host cells as foreign Treatment of GVHD Pathophysiology of GVHD Ferrara, et al. Lancet 2009;373:1550-61. Medications used for immunosuppression Class Drug Immune globulin Antithymocyte globulin (ATG) - Equine ATG: Atgam - Rabbit ATG: Thymoglobulin Monoclonal antibody Alemtuzumab - Campath Calcineurin Inhibitors Tacrolimus - Prograf Cyclosporine - Non-modified: SandIMMUNE - Modified: Gengraf or Neoral Antifolate antimetabolite Methotrexate Immunosuppressant Mycophenolate mofetil - CellCept Corticosteroids Methylprednisolone Prednisone mTOR inhibitor Sirolimus - Rapamune Alemtuzumab Anti CD52 monoclonal antibody CD52 expressed on: B and T lymphocytes Monocytes Macrophages NK cells Dendritic cells www.nature.com/reviews/drugdisc Alemtuzumab Adverse Effects Infusion related reactions Chills, dyspnea, fevers, hypotension, rigors May be fatal Premedicate with acetaminophen, diphenhydramine, ± corticosteroid Hypersensitivity reactions Cytokine release syndrome Opportunistic infections Requires anti-infective prophylaxis Antithymocyte Globulin (ATG) Mohty. Leukemia.2007, 21:1387-94. Antithymocyte Globulin Polyclonal antibodies active against T cells Administration Infuse over at least 6 hours Premedicate with acetaminophen, corticosteroids, and an antihistamine Rabbit ATG (Thymoglobulin®) and equine ATG (Atgam ®) are NOT interchangeable Antithymocyte Globulin Adverse effects Infusion-related reactions Fever, chills, headache Hypersensitivity reactions Cytokine release syndrome Increased risk of infections Serum sickness Calcineurin inhibitors http://www.nature.com/nrneph/journal/v2/n12/fig_tab/ncpneph0343_F2.html Calcineurin Inhibitors Inhibit T cell activation by suppressing production of IL-2 IV Administration Non-PVC tubing Continuous infusion over 24 hours IV:PO conversion = ~1:3 Therapeutic Drug Monitoring (TDM) PO: trough levels (30 min prior to dose) IV: be sure to waste sufficient amount to avoid falsely elevated levels Calcineurin Inhibitors: Adverse Effects Nephrotoxicity Hypertension Hyperglycemia Hypercholesterolemia Hypomagnesemia Hyperkalemia HUS/TTP CNS toxicity Tremor Posterior reversible encephalopathy syndrome (PRES) Calcineurin Inhibitors: Drug Interactions Antifungals Antibiotics GI Agents Fluconazole Metronidazole Metoclopramide Phenytoin Protease inhibitors Voriconazole Erythromycin Cimetidine Phenobarbital Sirolimus Posaconazole Clarithromycin Lansoprazole Carbamazepine St. John’s wort Ketoconazole Rifampin Anticonvulsants Many others CYP3A4 inducers and inhibitors Others Grapefruit juice Calcineurin Inhibitors: Cyclosporine Dosing TDM 3 mg/kg CIVI over 24 hours (initial) 5-6 mg/kg PO every 12 hours (initial) Modified ≠ non-modified May mix oral solution with orange juice 150-350 ng/ml Adverse effects Hirsutism/hypertrichosis Gingival hyperplasia Calcineurin Inhibitors: Tacrolimus Dosing 0.03 mcg/kg CIVI over 24 hours (initial) 90 mcg/kg PO every 12 hours (initial) TDM 5-15 ng/ml Methotrexate Mechanism of action Dosing Induces apoptosis of activated lymphocytes Blocks dihydrofolate reductase to inhibit purine synthesis 5-15 mg/m2 IVP on D+1, 3, 6, 11 +/- leucovorin rescue Adverse effects Mucositis Myelosuppression Hepatotoxicity Mycophenolate mofetil Mechanism of action Dosing 1000 mg PO/IV every 12 hours Drug interactions Inhibits lymphocyte proliferation by blocking purine synthesis Calcium & magnesium Adverse effects Nausea, vomiting, diarrhea Myelosuppression Corticosteroids Mechanism of action Affect number & function of B-cells & T-cells Dosing Systemic Methylprednisolone or prednisone 0.5-2 mg/kg IV/PO daily Taper when applicable Topical Budesonide-SR 3 mg PO every 8-12 hours (gut GVHD) Triamcinolone cream 0.1% to body +/hydrocortisone 1% to face (skin GVHD) Corticosteroid Adverse Effects Short term Hyperglycemia Mood disturbance, psychosis Insomnia Hypertension Fluid retention Skin atrophy Gastric ulcers Long term Adrenal suppression Moon facies Weight gain Osteoporosis Buffalo hump Cataracts Myopathy Infections Sirolimus Mechanism of action Dosing Inhibits proliferation of lymphocytes by blocking m-TOR 12 mg PO x 1 then 4 mg PO once daily Therapeutic Drug Monitoring (TDM) 3-12 ng/ml Trough levels (30 min prior to dose) http://www.nature.com/nrneph/journal/v2/n12/fig_tab/ncpneph0343_F2.html Sirolimus Drug interactions Similar to calcineurin inhibitors (CYP 3A4) Adverse effects Hyperlipidemia Myelosuppression Pneumonitis Thrombotic microangiopathy Additional Immunosuppressants: Treatment for GVHD TNFα blockers Etanercept, infliximab Pentostatin Alefacept Many drugs under investigation for treatment of acute and chronic GVHD Infection Prevention Use appropriate anti-infective prophylaxis throughout immunosuppressive therapy Pneumocystis carinii pneumonia Fungal infections Viral infections Summary Immunosuppression is utilized in allogeneic SCT to prevent rejection and GVHD, and for the treatment of GVHD Calcineurin inhibitors and sirolimus require TDM and close monitoring for side effects and drug interactions Infectious complications are common, making appropriate anti-infective prophylaxis important Thank You! Ashley Newland, PharmD anewland@mcvh-vcu.edu