Objectives
advertisement
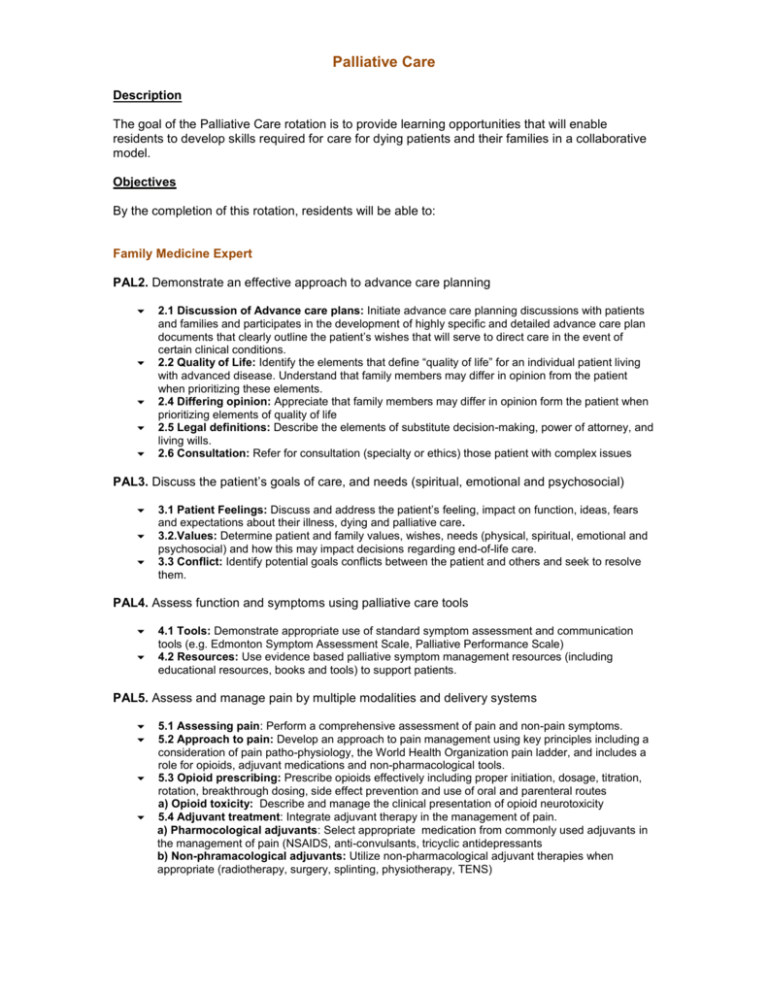
Palliative Care Description The goal of the Palliative Care rotation is to provide learning opportunities that will enable residents to develop skills required for care for dying patients and their families in a collaborative model. Objectives By the completion of this rotation, residents will be able to: Family Medicine Expert PAL2. Demonstrate an effective approach to advance care planning 2.1 Discussion of Advance care plans: Initiate advance care planning discussions with patients and families and participates in the development of highly specific and detailed advance care plan documents that clearly outline the patient’s wishes that will serve to direct care in the event of certain clinical conditions. 2.2 Quality of Life: Identify the elements that define “quality of life” for an individual patient living with advanced disease. Understand that family members may differ in opinion from the patient when prioritizing these elements. 2.4 Differing opinion: Appreciate that family members may differ in opinion form the patient when prioritizing elements of quality of life 2.5 Legal definitions: Describe the elements of substitute decision-making, power of attorney, and living wills. 2.6 Consultation: Refer for consultation (specialty or ethics) those patient with complex issues PAL3. Discuss the patient’s goals of care, and needs (spiritual, emotional and psychosocial) 3.1 Patient Feelings: Discuss and address the patient’s feeling, impact on function, ideas, fears and expectations about their illness, dying and palliative care. 3.2.Values: Determine patient and family values, wishes, needs (physical, spiritual, emotional and psychosocial) and how this may impact decisions regarding end-of-life care. 3.3 Conflict: Identify potential goals conflicts between the patient and others and seek to resolve them. PAL4. Assess function and symptoms using palliative care tools 4.1 Tools: Demonstrate appropriate use of standard symptom assessment and communication tools (e.g. Edmonton Symptom Assessment Scale, Palliative Performance Scale) 4.2 Resources: Use evidence based palliative symptom management resources (including educational resources, books and tools) to support patients. PAL5. Assess and manage pain by multiple modalities and delivery systems 5.1 Assessing pain: Perform a comprehensive assessment of pain and non-pain symptoms. 5.2 Approach to pain: Develop an approach to pain management using key principles including a consideration of pain patho-physiology, the World Health Organization pain ladder, and includes a role for opioids, adjuvant medications and non-pharmacological tools. 5.3 Opioid prescribing: Prescribe opioids effectively including proper initiation, dosage, titration, rotation, breakthrough dosing, side effect prevention and use of oral and parenteral routes a) Opioid toxicity: Describe and manage the clinical presentation of opioid neurotoxicity 5.4 Adjuvant treatment: Integrate adjuvant therapy in the management of pain. a) Pharmocological adjuvants: Select appropriate medication from commonly used adjuvants in the management of pain (NSAIDS, anti-convulsants, tricyclic antidepressants b) Non-phramacological adjuvants: Utilize non-pharmacological adjuvant therapies when appropriate (radiotherapy, surgery, splinting, physiotherapy, TENS) PAL6. Assess and manage common non-pain symptoms in the last year of life 6.1 Common EOL symptoms: Prevent, identify and manage common EOL symptoms including: nausea vomiting constipation bowel obstruction urinary retention urinary incontinence dyspnea cough delirium anxiety fatigue anorexia cachexia oral problems wounds ascites edema PAL7. Recognize and appropriately address palliative emergencies. 7.1 Palliative care emergencies: Recognize and address the following palliative care emergencies: spinal cord compression malignant bowel obstruction SVC syndrome cardiac tamponade seizures urinary obstruction hemorrhage 7.2 Refer: Refer appropriately for specialty consultation. FAM 5. Perform family medicine specialty-appropriate procedures to meet the needs of individual patients and demonstrate an understanding of procedures performed by other specialists to guide their patients’ care 5.1 Selection: Determine the most appropriate procedures or therapies. 5.2 Consent: Obtain and document informed consent, explaining the risks and benefits of, and the rationale for, a proposed procedure or therapy. 5.3 Prioritize: Prioritize a procedure or therapy, taking into account clinical urgency and available resources. 5.4 Performance: Perform the following procedures in a skillful and safe manner, adapting to unanticipated findings of changing clinical circumstances: nasogastic tube insertion parecentesis thoracocentesis 5.5 Aftercare: Develop a plan with the patient for the aftercare and follow-up after completion of a procedure. 5.6 Complications: Describe the normal post-operative healing course and recognize and manage post-operative complications. PAL8. Provide end-of-life care in multiple environments: hospital, hospice, care facility, home 8.1 Last hours: Plan and manage for the care of the dying patient during the last hours of life. a) Impending death: Recognize signs and symptoms of impending death 8.2 Setting: Recognize and access the differing resources in different palliative care setting: patients' homes, hospice, nursing / retirement/ long-term care home, specialized palliative care environment or in the hospital. a) Home care: Access home care resources appropriately, identifying unique aspects of caring for dying patient in the home. 8.3 Death certification: Pronounce death and conduct death certification. Identify situations in which the coroner must be contacted. a) Anticipation of death at home: Complete required documentation for patients planning to die at home Communicator PAL9. Demonstrate an effective approach to conveying bad news and discussing prognosis 9.1 Breaking bad news: Demonstrate sensitivity, compassion, empathy and respect when conveying difficult news to patients. 9.2 Prognosis: Inform patients of the diagnosis of life-threatening or life-limiting illness or change in trajectory of chronic illness. Inform patients of progression of disease and complications. PAL10. Communicate with patient, families and care team about palliative and end-of-life care 10.1Communicating with families: Identify situations that may benefit from a family meeting and facilitate these meetings 10.2. Supporting families: Support patients and families coping with loss and bereavement, grief (including anticipatory grief), risk factors for atypical grief and develop an awareness of local resources to assist families through this process Collaborator FAM13. Work effectively with physicians and other colleagues in the health care professions 13.1 Relationship: Establish and maintain positive relationships with physicians and other colleagues in the health care professions to support relationship-centered collaborative care 13.2 Team communication: Demonstrate clear and effective communication (both written and verbal) with physicians and other colleagues in the healthcare professions. 13.3 Shared decision-making: Negotiate overlapping and shared responsibilities with physicians and other colleagues in the health care professions. 13.4 Positive work environment: Implement strategies to promote understanding, manage differences, and resolve conflicts in a manner that supports a collaborative culture Leader/Manager FAM17. Engage in the stewardship of health care resources 17.1 Resource allocation: Allocate health care resources for optimal patient care, including referral to other health care professionals and community resources 17.2 Cost-appropriate: Apply evidence and management processes to achieve cost-appropriate care Scholar FAM24. Integrate best available evidence, contextualized to specific situations, into real-time decision-making 24.1 Identifying knowledge gap: Recognize practice uncertainty and knowledge gaps in clinical encounters and generate focused questions that can address them. 24.4 Integrating evidence: Integrate evidence into decision-making in their practice by reviewing and appropriately applying guidelines from organizations such as Health Canada, the College of Family Physicians of Canada, and relevant specialty societies such as the Canadian Pain Society. Professional FAM27. Demonstrate a commitment to patients by applying best practices and adhering to high ethical standards 27.1 Professional behavior: Exhibit appropriate professional behaviors and relationships in all aspects of practice, reflecting honesty, integrity, commitment, compassion, respect, altruism, respect for diversity, and maintenance of confidentiality. 27.2 Commitment to excellence: Demonstrate a commitment to excellence in all aspects of practice. PAL11. Recognize ethical challenges in providing palliative care and demonstrate the use of an ethical framework for decision-making. 11.1 Ethical framework: Employ ethical frameworks or tools for decision making in common EOL situations as they arise in any environment 11.2 Decision-makers: Describe a sound ethical and legal approach to: obtaining informed consent, assessment of capacity and substitute decision making 11.3 Physician assisted suicide: Distinguish between physician assisted suicide, euthanasia, palliative sedation and withholding and withdrawing therapy using an ethical framework. PAL12.1 Personal impact: Demonstrate skills in self-reflection on the personal impact of patient’s illness, dying and death 12.1 Discomfort: Recognize personal comfort or discomfort in responding to patient and family spiritual issues 12.2 Personal experience: Recognize how personal life experiences may affect their interactions with patients and their families. 12.3 Sharing: Identify a colleague or resource with whom to share discomforts or challenges Entrustable Professional Activities Perform common family medicine procedures. • Provide palliative end-of-life care. Evaluation Field Notes In-training Assessment Report (ITAR)