PALLIATIVE CARE - Heart of England Faculty of Education
advertisement
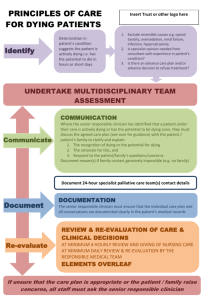
PALLIATIVE CARE Palliative Care Team Heart of England NHS Foundation Trust AIMS:• • • • To define what we mean by palliative care To define what we mean by end of life care To identify the needs of patients that are dying To highlight what the needs of the family are when a patient is dying • To identify the role of the HCA in caring for patients at end of life and their families • To identify factors that lead to a ‘good’ or ‘bad’ death OBJECTIVES At the end of the session HCA’s should be able to:• Define what we mean by palliative care • Define what we mean by dying • To enable HCA’s to recognise signs that a patient may be dying • Identify the most important aspects of care for a patient at end of life • Appreciate the needs of the family and their main concerns at end of life >4,000 Patient Deaths at HoEFT per Year! Aim of palliative Care The goal of palliative care is the achievement of the best possible quality of life for the patients and their families. (WHO 1990) DEFINITION OF PALLIATIVE CARE ………to achieve the best quality of life for individuals with any advanced, progressive illness, and their families, by the management of their physical symptoms and the provision of psychological, social and spiritual support. World Health Organisation 2002 End of Life Care Strategy 50% of complaints are related to end of life care in some way. Of 50 cases looked at relating to end of life care the complaints were around poor communication, lack of basic comfort, privacy and psychological care, and late or no referral to palliative care Relatives are often the 1st to notice a patient is dying! DoH 2008 DEFINITION OF DYING ‘If the patient has a progressive incurable disease, if reversible causes of deterioration have been excluded (eg infection, hypercalcaemia) and if they are very weak and drowsy and getting weaker every day, then they are dying.’ (Kaye 1999) Recognising a Dying Patient Drowsy/ unresponsive Poor urine output Cold peripheries Patient Laboured breathing Pale in colour Abnormal Observations Shallow breathing End of Life Carea daunting prospect ! ! REMEMBER “all the care she received before meant nothing, because she died the way she died” Husband of 43yr old lady who died in hospital “There is little time and only one chance to get it right” Common End of Life Symptoms • • • • Pain Agitation / terminal restlessness Nausea / Vomiting Moist Chest How does focus of care change? • • • • Investigations become irrelevant. Aiming to prolong life becomes irrelevant. Patient comfort takes priority. Increased support for the family is needed. (Kaye 1999) Other considerations • • • • • • Maintaining patient privacy and dignity Ensuring patients wishes are respected Support of family. Place of death. Spiritual requirements of patient. Staff support Cultural and Social Issues • • • • • • Social taboos Social denial of death Materialism Role of religion Experience of loss in the family Expectations of health and life HCA ROLE • • • • • • • • Maintaining privacy and dignity Provision of good essential nursing care Respecting wishes of patients and families Listening to patients and families Spending time with patients and their families Communicating with patients and families Communicate with other team members Recognising your own limitations and areas of concern What do we mean by Essential Nursing Care • Meeting patients hygiene needs • Providing good oral care • Monitoring of micturition • Maintaining regular bowel pattern • Regular visual observation • Appropriate pressure relief/skin care NB:- Think of caring for that person as you would wish a loved one to be cared for! Communication With dying patients and their relatives Barriers perceived by patients • Perceive Doctors/nurses as too busy • Don’t want to burden them with their worries • Believe Doctors/nurses primarily concerned about physical care • Think their perspectives may depend on treatments so don’t want to complain Continued . . . • Think their worries are silly or trivial or that professionals will think that. • Fear of admitting being unable to cope, breaking down, losing control. • Not being able to find the words to explain how they feel. • Anxiety about having their worse fears confirmed. Barriers to communication by Staff Being frightened of – - upsetting the patient – - causing more harm than good – - being asked difficult/unanswerable questions – - saying the wrong thing Continued. . . Feeling that – - there is not enough time – - cannot handle the emotions of patient or themselves – - not knowing enough – - not being part of their job – - not being able to do anything about the situation/helplessness Skills Required for Good Communication • Listening • Body language • Clinical skills/knowledge base • Awareness of family dynamics • Self awareness • Managing time, boundaries, endings • Empathy • Advocacy • Touch • Responding appropriately Non-verbal • • • • • • Eye contact Nodding Sit down Close door/pull curtain across Switch off mobiles Plan time for talk Verbal • • • • Checking Respond to emotional distress Use open questions Ask directly how they are ‘feeling’, (psychological state) • Make supportive comments Words to try When you think you want to say: • You are going to be just fine. Try this instead: • Are there some things that worry you? • Don't talk like that! You can beat this! • This must be hard to come to terms with • I can't see how anyone can help. • We will work with you. • What do the doctors know? You might live forever. • Don't be glum. You will get well. • Do you think the doctors are right? How does it seem to you? • It must be hard. Can I just sit with you for a while. Key Points • Ensure patients privacy and dignity are maintained at all times. • High quality essential nursing care is a priority • Good communication with both patients and relatives is essential • Recognising spiritual needs of patients is important