Malignant Peripheral Nerve Sheath Tumor of Scalp: A case
advertisement

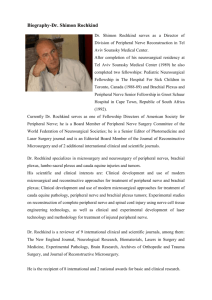
Malignant Peripheral Nerve Sheath Tumor of Scalp: A case report with review of literature. Abstract Malignant Peripheral nerve sheath tumors(MPNST) account for approximately 5-10% of soft tissue sarcomas and occur most often in limbs and paraspinal region. This entity is an extremely rare occurrence in the scalp with sporadic case reports appearing in English literature since 2003.Here we describe a case of 38 year old male with MPNST of the scalp over the right temporo-mastoid region, its course of management and the difficulties encountered. The case represents not only a rare tumor occurring in a rarer location but also the difficulties in obtaining clear margins of resection for sarcoma in scalp with bone erosion as dura does not seem to present any significant barrier for local invasion. Introduction Malignant peripheral nerve sheath tumor ( MPNST) are defined as malignant tumors either arising from a peripheral nerve sheath ( except epineurium and vasa nervorum ) or showing a nerve sheath differentiation (1). MPNST usually arise from large peripheral nerves and are more common in limbs. Head and neck region in general and scalp in particular are extremely uncommon locations for their occurrence . One of the largest single institution series of MPNST had only nine cases in head and neck region of a total of 200 cases (2). Here we describe the presentation and management of a rare case of a MPNST of scalp with calvarial erosion. Case Report A 38 year old male presented with a large slowly growing swelling over right temporomastoid region of head over a period of 2 years. The patient had noticed an increased rate of growth over the previous 8 months and it had become painful since about 3 weeks before admission. The swelling was uniformly firm in consistency, with well defined margins, globular in shape, non- transilluminant , and was immobile over the underlying structures. The skin over the lesion was not pinchable and showed an area of ulceration over its posterior extent . He had been employed as a driver in a middle eastern country and had undergone an incisional biopsy from the lesion there and the incision site had not apparently healed and had persisted as an ulcer. The margins of this ulceration were everted and the floor was covered with slough. A thin serous discharge was also observed from the ulcer.( Fig 2) There was no lymphadenopathy. There were no stigmata of NF1. CT scan had revealed a soft tissue mass with evidence of strong enhancement with bone window revealing erosion of skull( Fig 1). The patient was taken up for wide excision of the mass by neurosurgery service . Intraoperatively , the lesion seemed to have vague capsule around it but had areas where it was infiltrating the temporalis muscle . There was no clear plane of the lesion from the scalp . The lesion was pinkish in coloured and was relatively avascular. An area of erosion of skull was seen. Wide excision of the of the lesion was done . The final histopathology report was suggestive of MPNST .(Fig 3)Immunohistochemistry for S-100 antigen was done revealing 60% positivity. A diagnosis of malignant peripheral nerve sheath tumor was made. The patient was planned for re-excision as only 1cm margin had been obtained in the first instance. This needed excision of the ipsilateral pinna for which the patient was not ready. He was started on chemotherapy with Adriamycin( 100mg) every 3 weeks for six cycles. After about 2 months of completion of chemotherapy, a recurrence was observed at the posterior margin of the resection( occipital region). This time, he underwent radiotherapy( 50 Gy in 25 fractions).This was unable to control the growth and he underwent chemotherapy with Gemcitabine(900 mg/sq m on day 1 and 8) and Docetaxel(35 mg/sq m on day 1 and 8) every 3 weeks for six cycles. The external growth was controlled with chemotherapy. However, he had an episode of seizure and the imaging revealed massive dural invasion and involvement of transverse and sigmoid sinuses with involvement of underlying brain. The extent of involvement precluded a safe resection. After discussion about the available options, the patient decided to take up therapy with Pasopanib( 800mg daily for two months). At the time of reporting, the patient has been under treatment for almost two years since his first surgery. Presently, the patient is symptomatically relieved while off Pasopanib for one month. Discussion: MPNSTs are uncommon malignancies accounting for 5 to 10% of all soft tissue sarcomas with an incidence of 0.1/100,000 per year in the general population (2). These lesions are commonly located in thighs, buttocks, and brachial plexus. Scalp in particular and head and neck in general are extremely uncommon locations for their occurrence and very few case reports have been appearing in English literature since 2003 (3,4,5,6,7,8,9).However, the diagnosis should be strongly considered in any patient with rapidly enlarging swelling of the scalp. The only prognostic indicators for recurrence and metastasis have been negative tumor margins after excision and radiotherapy. Tumor location has not been found to directly affect the same. However, the inability to provide tumor free margins in certain locations like headneck, retro peritoneum and thoracic cavity may render these locations unfavourable. Approximately two- thirds of MPNSTs arise by malignant degeneration of pre-existing neurofibromas with or without neurofibromatosis 1. Others arise de-novo. A higher incidence of MPNST has also been noted after radiation exposure(1). Our case seems to have been a malignant lesion from the beginning. Imaging features of MPNST in other locations like pelvis have been well summarised by some authors (10) and include diffuse or ring enhancement of MPNST as against central enhancement of their benign counterparts. Microscopically, MPNST is a densely cellular tumor that shows fascicular areas with alternate myxoid areas in a swirling pattern classically called merbellisation (1). Cells may be spindle shaped with irregular contours. Malignancy as in other tissues is suggested by invasion of surrounding tissues, Invasion of vascular structures, nuclear pleomorphism, necrosis and mitotic activity. S-100 immunoreactivity has been widely used in diagnosing PNSTs. Though it shows focal positivity in almost 70 to 90% MPNSTs, a more diffuse positivity suggests BPNSTs including degenerating schwannomas (11). Ki-67 immunoreactivity of more than 5% has been suggested as an additional supporting criterion. The present consensus about management of MPNSTs is carry out a wide surgical excision and follow it up with adjuvant radiotherapy. Chemotherapy has a role in case of advanced local disease and metastatic disease. The local recurrence rate for MPNSTs has historically been reported to range from 40-65% and the distant recurrence rate has similarly been reported to range from 40-68% (12). In conclusion, MPNSTs though extremely rare in head and neck region, should be strongly considered in differential diagnosis of rapidly enlarging solid lesion of scalp. These are aggressive lesions and demand an early diagnosis and multimodality treatment. References: 1.Enzinger FM, Weiss SW. Malignant tumours of peripheral nerves. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumors. Vol. 31. St. Louis: CV Mosby Company; 2001:1209–1263. 2. Matteo Anghileri, Rosalba Miceli,Marco Fiore, Luigi Mariani, Andrea Ferrari,Chiara Mussi, Laura Lozza et al: Malignant Peripheral Nerve Sheath Tumors Prognostic Factors and Survival in a Series of Patients Treated at a Single Institution. Cancer 107:1065-1074, 2006. 3. Demir Y, Tokyol C. Superficial malignant schwannoma of the scalp. Dermatol Surg 29:879-81,2003 4. Garg A, Gupta V, Gaikwad S B, Mishra N K, Ojha B K, Chugh M, Sharma M.C. Scalp malignant nerve sheath tumor (MPNST) with bony involvement and new bone formation:case report. Clinical Neurology and Neurosurgery 106 :340-344, 2004. 5. Fukushima S, Kageshita T, Wakasugi S, Matshushita S, Kaguchi A,Ishihara A, Ono T. Giant malignant peripheral nerve sheath tumor of scalp. J Dermatol 33:865-868, 2006 6.Kumar P, Jaiswal S, Agarwal T, Verma A, Datta N R. Malignant peripheral nerve sheath tumor of the occipital region:case report. Neurosurgery 61:1334-1335 ,2007 7.Telera S, Carapella C, Covello R, Cristalli R, Carosi M A, Pichi B, Spriano G. Malignant peripheral nerve sheath tumors of laterall skull base. J Craniofac Surg 19:805-812, 2008 8.Voth H, Nakai N, Wardelmann E, Wenzel J, Bieber T, Wendetner C M, Reinhard G, SchmidtWendtner M H. Dermatol Surg 37:1684-88,2011 9.Jhawar S S, Mahore A, Goel N, Goel A. Malignant peripheral nerve sheath tumor of scalp with extradural extension: case report. Turkish Neurosurgery 22:254-256, 2012 10. Akira Ogose, Tetsuo Hotta, Tetsuro Morita, Takeshi Higuchi3, Hajime Umezu, Satoshi Imaizumi, Hiroshi Hatano, Hiroyuki Kawashima, Wenguang Gu and Naoto Endo. Diagnosis of Peripheral Nerve Sheath Tumors around the Pelvis. Jpn J Clin Oncol :34(7)405–413,2004 11. Enzinger FM, Weiss SW. Soft tissue tumors, 3rd edn. St. Louis: Mosby:821–928.1995 12. Hruban RH, S. M., Senie RT, Woodruff JM: Malignant peripheral nerve sheath tumors of the buttock and lower extremity. A study of 43 cases. Cancer, 66 : 1253-65, 1990.