definitions - WordPress.com
advertisement
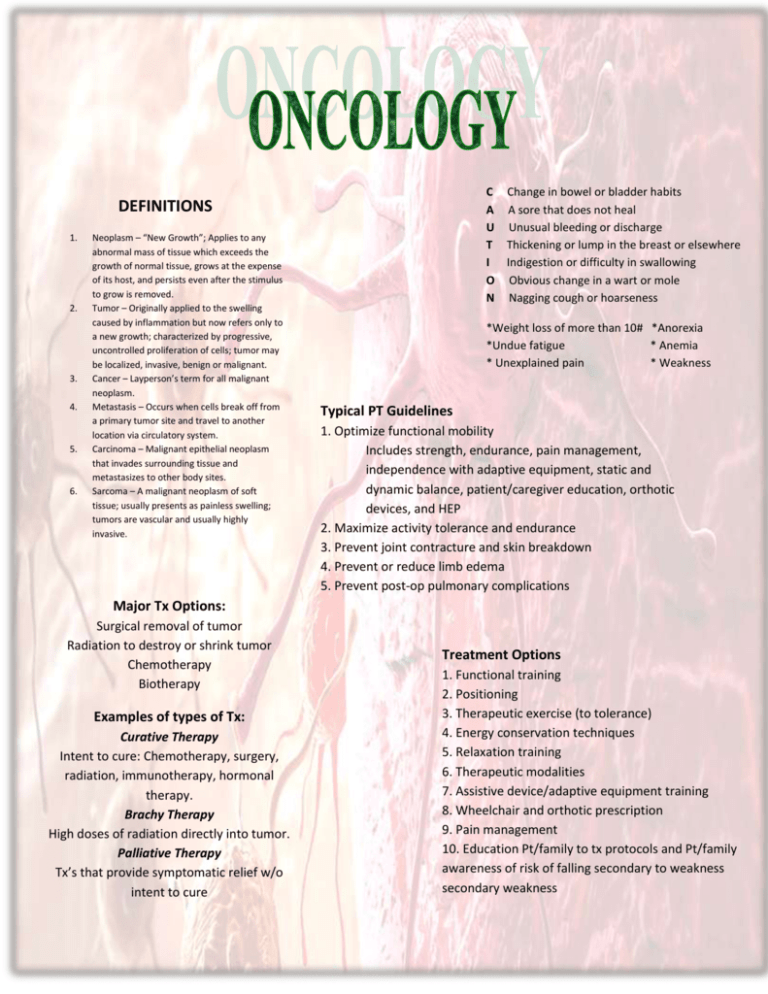
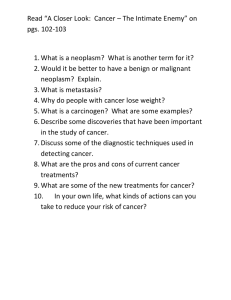
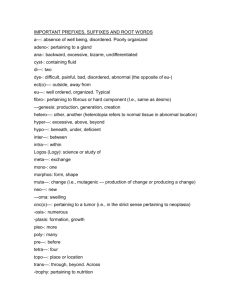
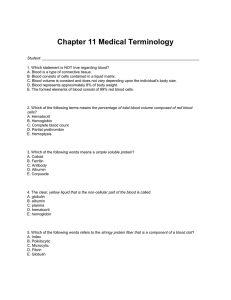
C Change in bowel or bladder habits A A sore that does not heal U Unusual bleeding or discharge T Thickening or lump in the breast or elsewhere I Indigestion or difficulty in swallowing O Obvious change in a wart or mole N Nagging cough or hoarseness DEFINITIONS 1. 2. 3. 4. 5. 6. Neoplasm – “New Growth”; Applies to any abnormal mass of tissue which exceeds the growth of normal tissue, grows at the expense of its host, and persists even after the stimulus to grow is removed. Tumor – Originally applied to the swelling caused by inflammation but now refers only to a new growth; characterized by progressive, uncontrolled proliferation of cells; tumor may be localized, invasive, benign or malignant. Cancer – Layperson’s term for all malignant neoplasm. Metastasis – Occurs when cells break off from a primary tumor site and travel to another location via circulatory system. Carcinoma – Malignant epithelial neoplasm that invades surrounding tissue and metastasizes to other body sites. Sarcoma – A malignant neoplasm of soft tissue; usually presents as painless swelling; tumors are vascular and usually highly invasive. *Weight loss of more than 10# *Anorexia *Undue fatigue * Anemia * Unexplained pain * Weakness Typical PT Guidelines 1. Optimize functional mobility Includes strength, endurance, pain management, independence with adaptive equipment, static and dynamic balance, patient/caregiver education, orthotic devices, and HEP 2. Maximize activity tolerance and endurance 3. Prevent joint contracture and skin breakdown 4. Prevent or reduce limb edema 5. Prevent post-op pulmonary complications Major Tx Options: Surgical removal of tumor Radiation to destroy or shrink tumor Chemotherapy Biotherapy Examples of types of Tx: Curative Therapy Intent to cure: Chemotherapy, surgery, radiation, immunotherapy, hormonal therapy. Brachy Therapy High doses of radiation directly into tumor. Palliative Therapy Tx’s that provide symptomatic relief w/o intent to cure Treatment Options 1. Functional training 2. Positioning 3. Therapeutic exercise (to tolerance) 4. Energy conservation techniques 5. Relaxation training 6. Therapeutic modalities 7. Assistive device/adaptive equipment training 8. Wheelchair and orthotic prescription 9. Pain management 10. Education Pt/family to tx protocols and Pt/family awareness of risk of falling secondary to weakness secondary weakness General Guidelines for PT 5. If patient is on isolation precautions make 1. Know stage and grade of cancer sure to sterilize all diagnostic and exercise 2. Patients may be on bed rest: Deep equipment. breathing exercises, position changes and bed 6. Watch placement of equipment on exercise program. patient’s sensitive skin. 3. Metastatic processes, especially to the bone 7. Emotional support for pt and family is are at high risk for pathologic fracture. Take helpful and appreciated. care with manual chest PT techniques and 8. Timely communication with entire health resistive exercises. care team is essential for safe and effective 4. Pt/family education: safety management, care. energy conservation, postural awareness, and 9. Monitor lab values daily. body mechanics. 5. If patient is on isolation precautions make sure to sterilize all diagnostic and exercise equipment. 6. Watch placement of equipment on patient’s CONTRAINDICATIONS to PT sensitive skin. count < 50,000/uL 7. Emotional support for pt and family Platelet is Hemoglobin < 10g/dl helpful and appreciated. blood cell count < 300/uL 8. Timely communication with entireWhite health Absolute care team is essential for safe and effective granulocytes < 2500/uL care 9. Monitor lab values daily PEARLS *Schedule Tx when pt has peak energy; find their best time of day * Modify Tx as needed to accommodate for side effects of Tx *Conduct exercise at 40-65 of peak HR *Chemobrain: The Fog Confusion Fatigue Limited attention span Short term memory An unusual degree of difficulty w/concentration Difficulty w/word finding *Multi tasking and organization problems * Monitor cardiac/respiratory systems and watch for signs of dyspnea, sweating and pallor Post Radiation 1. No PT while person has implanted radioactive seeds 2. Massage and heating modalities should be withheld for 1 year in an irradiated area 3. Caution should be taken with skin and underlying tissues in areas irradiated by beam as they will be fragile (blue markings in area)