27 Chest Injuries
advertisement

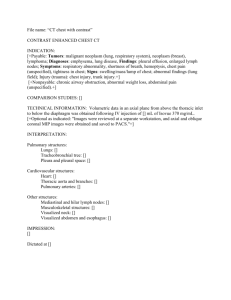
Chest Injuries Chapter 27 Review anatomy of the chest: Mechanics of Ventilation: • Inspiration – • Intercostal muscles contract and diaphragm flattens. Expiration – Intercostal muscles and diaphragm relax; tissues move back to normal position. • Phrenic nerves exit the spinal cord at C3, C4, and C5. • Spinal cord injury below C5 • – Loss of ability to move intercostal muscles – Diaphragm can still contract; patient can still breathe. Spinal cord injury at C3 or higher – No ability to breathe *note that a spinal cord injury below c-5 results in paralysis below the shoulders Injuries to the Chest: • Closed chest injuries – • Caused by blunt trauma Open chest injuries – Caused by penetrating trauma Signs and Symptoms: • Pain at site of injury • Pain aggravated by increased breathing • Bruising to chest wall • Crepitus with palpation of chest • Penetrating injury to chest • Dyspnea • Hemoptysis • Failure of chest to expand normally • Rapid, weak pulse and low blood pressure • Cyanosis around lips or fingernails Scene Size Up: • Observe for hazards • Do not disturb potential evidence • Put several pairs of gloves in your pocket. • Consider spinal immobilization • Ensure that police are on scene if incident involved violence Initial Assessment: • General impression • – Quickly evaluate ABCs – Difficulty speaking may indicate several problems – Patients with significant chest injuries will look sick Airway and breathing – Ensure that patient has a clear, patent airway – Protect the spine – Inspect for DCAP-BTLS Inspection (AB): • Decreased breath sounds usually indicate significant damage to a lung • If both sides of chest do not have equal rise and fall, chest muscles have lost ability to work properly • If one section of chest moves in opposite direction from the rest of the chest (paradoxical motion), this is a life threat Immediate Interventions: • Apply an occlusive dressing to any penetrating chest injury • Stabilize paradoxical motion with a large bulky dressing and 2'' tape • Apply oxygen via nonrebreathing mask at 15 L/min • Provide positive pressure ventilations if breathing is inadequate Circulation (C): • Assess patient’s pulse • Consider aggressive treatment for shock • Internal bleeding can quickly cause death Transport Decision: • Rapidly transport if patient has problems with ABCs. • Pay attention to subtle clues. – Skin signs – Level of consciousness – Sense of impending doom Focused History and Physical Exam: • Focused physical exam – • For a patient with isolated chest injury and limited MOI Rapid physical exam – For a patient with a significant MOI – Use DCAP-BTLS – Do not focus just on the chest wound • Obtain baseline vital signs • Obtain SAMPLE history quickly Interventions: • Provide complete spinal immobilization • Maintain open airway; be prepared to suction • Provide assisted ventilations if needed • Control bleeding • Place occlusive dressing over penetrating chest wound • Stabilize flail segment with a bulky dressing • Treat aggressively for shock • Do not delay transport Detailed Physical Exam: • Perform enroute to the Hospital if time allows Ongoing Assessment: • Assess effectiveness of interventions • Reassess vital signs • Communication and documentation – Communicate with hospital early if patient has significant MOI – Describe injuries and treatment given Complications of Chest Injuries: • A pneumothorax occurs when air leaks into the space between the pleural surfaces. • Air accumulates in the pleural space • Air enters through a hole in the chest wall • The lung may collapse in a few seconds or a few minutes • An open or penetrating wound to the chest is called a sucking chest wound • Treat with a flutter valve dressing • • • Spontaneous Pneumothorax • Some people are born with or develop weak areas on the surface of the lungs • Occasionally, the area will rupture spontaneously, allowing air into the pleural space • Patient experiences sudden chest pain and trouble breathing • Consider a spontaneous pneumothorax for a patient with chest pain without cause Tension Pneumothorax • Can occur from sealing all four sides of the dressing on a sucking chest wound • Can also occur from a fractured rib puncturing the lung or bronchus • Can also result from a spontaneous pneumothorax Signs and Symptoms • Respiratory distress • Distended neck veins • Tracheal deviation • Tachycardia • Low blood pressure • Cyanosis • Decreased lung sounds • Treatment • If a tension pneumothorax develops from sealing an open chest wound, partly remove the dressing to let the air escape. • • If there is no open wound, follow local protocol Hemothorax- Collection of blood in the pleural space • Suspect if the following are seen: • Signs and symptoms of shock • Decreased breath sounds on affected side • If both air and blood are present in the pleural space, it is a hemopneumothorax Rib Fractures: • They are very common in the older people. • A fractured rib may lacerate the surface of the lung • Patients will avoid taking deep breaths and breathing will be rapid and shallow • The patient often holds the affected side to minimize discomfort • Administer oxygen Flail Chest:- Segment of chest wall detached from rest of thoracic cage • Occurs when: – Three or more ribs are fractured in two or more places. – Sternum is fractured along with several ribs. • Creates paradoxical motion • Treatment: – Maintain airway – Provide respiratory support with BVM if needed – Perform ongoing assessments for pneumothorax and other respiratory complications – Immobilize flail segment Pulmonary Contusions: • Bruising of the lung • Develops over hours • Alveoli fill with blood, and edema accumulates in the lung, causing hypoxia • Provide oxygen and ventilatory support Traumatic Asphyxia:- Sudden, severe compression of chest • Produces rapid increase in pressure within chest • Results in neck vein distention, cyanosis, and bleeding into the eyes • Provide supplemental oxygen and monitor vital signs • Transport immediately Blunt Myocardial Injury: • Bruising of heart muscle • Pulse is often irregular • There is no prehospital treatment for this condition • Check patient’s pulse and note irregularities • Provide supplemental oxygen and transport immediately Pericardial Tamponade- Blood or other fluids collect in the pericardium • Signs and symptoms: – Very soft and faint heart tones – Weak pulse – Low blood pressure – Decrease in difference between systolic and diastolic blood pressure – Jugular vein distention (JVD) – Provide oxygen and transport quickly Laceration of the Great Vessels: • The superior vena cava, inferior vena cava, pulmonary arteries and veins, and aorta are contained in the chest • Injury to these vessels can cause fatal hemorrhage • Treatment includes: – CPR – Ventilatory support – Supplemental oxygen – Transport immediately