Joe`s Rheumatic and Autoimmune Disorders Outline
advertisement

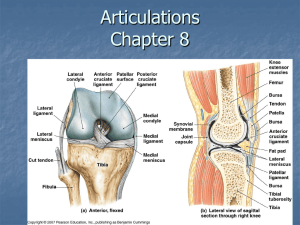
Rheumatic and Autoimmune Disorders • Rheumatic Diseases • Dictionary: Disorders of connective tissue, especially the joints and related structures, characterized by inflammation, degeneration, or metabolic derangement. • Affect: – Skeletal muscles – Bones – Cartilage – Ligaments – Tendons – Joints • Rheumatic Diseases • Inflammatory v. non-inflammatory • Monoarticular v. polyarticular-these disorder affect mutiple joints • Pathophysiology Synovial Joint • Function = movement • Articular cartilage = friction free movement • Synovial fluid = shock absorber • Synovitis = Primary or Secondary • Inflammation 1) Antigen stimulus a) Activation of monocytes “leukocyte that functions in the ingestion of bacteria” and… b) Activation of T cells “specific kind of white blood cell, active in controlling the immune response and attacking infections” c) Antibodies form immune complexes with antigens “substance that induces an immune response” 2) Phagocytosis “Ingestion and digestion of bacteria” 3) Inflammatory reaction- joint effusion, pain, edema, swelling Inflammation • Phagocytosis Leukotrienes & Prostaglandins ↓ Collagenase ↓ Breaks down collagen ↓ Synovial membrane damage, Pannus formation, destruction of cartilage, & erosion of bone. Pannus- forms in the joint affected by the disease, causing loss of bone and cartilage Pannus Formation A growth composed of thickened synovium. Forms due leak of fluid. • Pannus = “Granulation tissue” • Composed of inflammatory cells • Erodes articular cartilage • Leads to bone destruction – Overgrowth of bearing surface – Breakdown of joint surfaces Steps of Pannus formation: 1) RA begins with synovitis of the affected joint 2) Inflammatory chemicals are inappropriately released 3) Inflammatory blood cells migrate to the joint, causing swelling 4) Inflamed synovial membrane thickens into a pannus 5) Pannus erodes cartilage, scar tissue forms, articulating bone ends connect 6) The end result, ankylosis, produces bent, deformed fingers Systemic Inflammation • Diffuse Connective Tissue Diseases: – Systemic Lupus Erythrematosus- a chronic inflammatory disease affecting many systems of the body. – Rheumatoid Arthritis- a chronic, inflammatory, destructive, and deforming collagen disease that has an autoimmune component. It is characterized by inflammation and increased synovial exudate, leading to thickening of the membranes and swelling of the joints. – Scleroderma- chronic hardening and thickening of the skin caused by new collagen formation. – Polymyalgia rheumatica- a chronic, episodic, inflammatory disease of the large arteries. Joint Degradation • Several theories – Genetic or hormonal- strongly link to estrogen – Mechanical factors- obesity – Prior joint damage- trauma to joints are more prone to have problems later – Bone stiffeningJoint Effusions • Friction at bone ends damage tiny blood and lymphatic vessels. Blood particles, lymph, and chemical mediators accumulate in the synovial fluid. • AKA Synovitis Clinical Manifestations of Rheumatic Disorders • PAIN • Swelling • Limited movement • Stiffness • Weakness/ Fatigue Assessment Assessment 5-6Qs & Allergy 9-10Qs & HIV 10Qs • Health history o Onset & evolution of sx o Family o Past hx o Contributing factors o How does it affect lifestyle o Treatments attempted… Successful? • Physical Exam o Functional assessment (Limp, balance support) Other Systemic Assessments See chart pg 1609 “systemic assessments w/ RA • Skin- buising, inflamm of skin, thinning of skin (prednisone), warmth/infected, photo-sensitivity • Hair- allopecia • Eye- grittiness or dryness (lacrimal gland decr) • Ear- ringing of the ears, tinnitus, hearing loss, poos from bone stiffening or due to meds • Mouth- ulcerations, jaw stiffness due to inflam process diff eating/chewing • Chest- pleuralitis, inflam of tissue • Cardiovascular system- pericarditis, Reynauld’s disease • Neurological- HAs, depression, psycosies Diagnostic Studies • Arthrocentesis- joint aspiration, goal is to sample fluid for analysis. This will also decr pain. W/ inflam diseases it’ll look milky, pus-like, bloody. • X-rays • Arthrography- move joint around in diff positions to take a look at it. Giving a functional picture of joint. • Bone & Joint scans- bone density and overgrowth • Tissue Biopsy Blood Studies o ESR- Erythrocyte Sedimentation Rate: the rate at which red blood cells settle out in a tube of blood under standardized conditions o Creatinine- incr (due to wide spread inflam indicative of nephritis) because of systemic complications o RBC, H/H, WBC- blood due to meds (some meds can cause ulcerations) o Uric acid o ANA (Antinuclear Antibody)- very specific to Rheumatic diseases. added:Present in 30% of patients with RA. o Rheumatoid factor- An antibody that reacts with Ig (an immunoglobulin) found particularly in patients with rheumatoid arthritis. o C-reactive protein- byproduct of inflammation o Immunoglobulin electrophoresis Difficult Diagnosis….. • Not a clear-cut diagnosis, because s/s are vague • Don’t make diagnostic assumptions • Rheumatology Consult, a specialist to help make a better dx Gerontological considerations • “Older person’s disease” • Secondary concern- arthritis may not be the number one concern • Diagnosis difficulties • Increased risk osteoporosis- due to lack of support for joints • Quality of life – lifestyle changes- laying awake at night worrying, sleeplessness Medical Management Pharmacologic: • Salicylates- aspirin, not as common • NSAIDs- big help (give w/ food & monitor GI function) • DMARDs (Disease Modifying AntiRheumatic Drugs) – Will inhibit breakdown of cells. • Antimalarials (Plaquenil)- antiarthritic, and lupus erythematosus suppressant agent. Monitor visual changes and skin rash • Sulfasalazine (Azulfidine)- antibacterial to treat ulcerative colitis and rheumatoid arthritis Antidepressants – Management • Non-pharmacological – Pain • Hot, cold (compresses) • Devices to protect & support joints (Cane, walker) • Exercise, Activity – Passive exercises will be needed – Need to keep moving, even when pain is a factor Goals of Management • Suppress inflammation • Suppress Autoimmune response • Control Pain • Maintain/improve joint mobility (splints, compresses) • Maintain/improve functional status (devices: walker, canes) • Increase knowledge • Promote self-management (see what works best for them) Nursing Diagnosis • Acute & chronic pain • Fatigue • Disturbed sleep pattern • Impaired physical mobility • Disturbed body image • Self – care deficits • Ineffective coping Nursing Interventions • Relieving Pain & discomfort • Promoting restorative sleep • Increasing mobility • Improving body image & coping • Monitoring & managing potential complications- watch out for injury, neuro problems Discharge Planning • Maintain independence • Pt teaching • Medications (Monitor reaction to meds) • Required monitoring for meds • Safety/mobility • Teaching self–injection meds Diffuse Connective Tissue Diseases • Group of Chronic disorders • Exacerbation “incr in seriousness of disease” ↔ Remission “partial/complete disappearance” • Etiology Unknown Diseases: • • • • • Rheumatoid Arthritis- chronic inflammation of joints & surrounding tissue Lupus (SLE)- chronic inflammatory disease Scleroderma- chronic hardening and thickening of the skin Polymyositis- inflammation of muscles, accompanied by deformity, edema, insomnia, pain, sweating, and tension Polymyalgia- Many muscle pain Rheumatoid Arthritis (RA) Clinical Manifestations • More common in women • Joint Pain- usually bil & begins in smaller joints • Swelling • Warmth & erythema • Loss of function • Spongy or boggy joint tissue • Begins with Small Joints!! • Acute onset • Deformity hands, feet Extra-articular features • Fatigue • Fever • Weight loss • Anemia • Lymph node enlargement • Raynaud’s phenomenon- strong link to immune problems • • Rheumatic nodules Associated Disorders • Arthritis- inflam of arteries (can lead to HAs) • Neuropathy- ex: decr sensation in toes • Pericarditis- tissue surrounding the heart (pericardium) becomes inflamed • Splenomegaly- abn enlargement of the spleen • Sjögren’s syndrome- autoimmune disorder in which immune cells attack and destroy the exocrine glands that produce tears and saliva Physical Assessment of RA • Bilateral & symmetric stiffness • Joint Tenderness • Joint Swelling • Temperature changes in joints • Assess for extra-articular symptoms Diagnostic Findings with RA • Elevated Rheumatiod factor- happens in 80% of patients • RBC & C4 complement- goes w/ inflammation • C-reactive protein- Produced by the liver - present during episodes of acute inflammation. • ANA • Synovial fluid changes- cloudy, dark • X-ray changes- joint space will narrow Stages of Rheumatoid Arthritis • Early- catch early & treat (2yr window for symptom control) • Methotrexate- Main med, anti-inflammatory drug w/ immune suppressing effect. Will see alopecia, N/V, wt loss, fatigue. • Moderate- erosive • Educate. • Persistent- erosive • Provide support, corticoid steroids to prevent inflam. Reconstructive Surgery for repair may be required. • Advanced- unremitting • Immunosuppressive meds. Pts at this stage may be wheelchair bound. Nursing Management • Dietary assessment- high vitamin/protein/iron • Manage… • Wt • Pain • Sleep disturbance • Fatigue • Altered mood • Limited mobility • Educate – disease, meds, coping • Support groups may be needed Systemic Lupus Erythematosus (SLE) Immune Regulation Problem: production of autoantibodies. – 10 times more in women – 3 times more common in African-Americans Patho of Lupus Abnormal Suppressor T-cell Function ↓ Immune Complex Deposition & Tissue Damage ↓ Inflammation ↓ Antigen Stimulation ↓ Antibody Synthesis & Cyclical Pattern Systemic Lupus Erythematosus Cause?? Thought to be due to a combination of ... – Genetic – Hormonal – Environmental factors • Sun exposure can trigger lupus! – Certain Meds • Pronestyl, hydralazine, isoniazid, Thorazine, some anti-seizure meds. • Systemic Lupus Erythematosus http://www.lupus.ab.ca/viewpage.asp?p=resources-flash Clinical Manifestations Lupus • Musculoskeletal – Arthralgias, arthritis (synovitis)- joint pain – Joint swelling, tenderness, pain with movement- morning stiffness… big prob w/ these pts. – Morning stiffness Clinical Manifestations Lupus • Skin lesions – Annular polycyclic- reddish spots… <image> – Discoid lupus lesions- tuff on black women <image> – Butterfly rash – Oral ulcers– Alopecia- hair loss Systemic Manifestations Lupus • Pericarditis- the most common disorder in Lupus • Renal- Creatine level • Hypertension • CNS Diseases • Neuro-psychiatric- signs of dementia or mood alterations Diagnostic Tests for SLE Systemic Lupus Erythematosus • No one test confirms Diagnosis – Moderate to severe anemia – Thrombocytopenia – Leukocytosis – Positive ANA Medical Management Lupus – NSAIDs – Corticosteroids- most important med for lupus – Antimalarial Meds – Immunosuppressive agents Nursing Management • Fatigue • Impaired skin integrity • Body image concerns • Lack of knowledge • Self management Scleroderma No known cure • “Hard skin”- excess collagen production under skin • Edema (Hard, tight, causing diff of movement) • Rare Connective Tissue Disease • More common in women Scleroderma • Starts with Raynaud’s & swelling of hands • Hard, taut, shiny skin • Dry skin • Moves slowly abd can be isolated to one area for years • Limited mobility • Term- calcinosis- calcium deposits in the tussues, charateristic sign of Scleroderma Assessment of Scleroderma • General physical assessment – Skin changes – Body systems assessments • Big problems Hardening of the esophagus • May see scarring of lungs and stuff intestinal mucosa (causing persistant diarrhea) – No conclusive diagnostic tests • CREST – Calcinosis, Reynauld’s, Esophageal hardening, Screla of digits, Telangiectasis Treatment of Scleroderma Main goal: decr pain and limit disability • Continual assessment of progression • Treat symptoms • Moderate exercise- to decr stiffness • Avoid temperature extremes- mainly cause of Reynauld’s • Use lotion for skin dryness- moist and movable Medications for Scleroderma • NONE to delay its progression • Ca++ Blockers for Raynaud’s • Anti-inflammatories Nursing Diagnoses: Scleroderma • Impaired Swallow/Airway is a main focus! • Impaired skin integrity- excellent skin care is must! Creams, ointments to keep skin soft, protect from temp extremes • Self-care deficits • Imbalanced nutrition- Due to swallowing impairment • Disturbed body image Polymyalgia Rheumatica • Severe muscle stiffness • Most common in shoulders, upper arms, neck, hips, & thighs • Auto-immune process • Giant cell arteritis Spondyloarthropathies • Inflammation at sites of bone attachment – Tendons – Joint capsules – Ligaments • Occurs more commonly in males • Arthritis of the sacroiliac joints is common Spondyloarthropathies • Ankylosing spondylitis- spine fixates – Ankylosis = fixation • Most common feature: Back pain • Breathing problems!!! – Reactive arthritis- other probs • Psoriatic arthritis- other probs Gout • • • Hyperuricemia- over secretion of ***uric acid in blood Incidence: (picture overwt elderly man) – ↑ Age – ↑ BMI – More common in males Suspected Cause? – Primary hyperuricemia • Severe dieting/starvation (***high protein intake) • High purine intake (shellfish, red meat) • Hereditary – Secondary hyperuricemia • Leukemia • Multiple myeloma • • Anemia Psoriasis Patho of Gout Increases in uric acid levels ↓ Urate crystals gather in joints ↓ Tophi “lrg gouty nodules due to uric acid accumulation” and kidney stones develop (***Tophi most commonly found in toes) What does this have to do with immune function???? • Urate crystals obtained during synovial fluid analysis are often covered with IgG antibodies! • There is an immunologic link to gout formation. Manifestations of Gout • Pain and inflammation of joints • Tophi • Renal impairment • Uric acid urinary calculi Treatment of Gout • ***Decr protein and ETOH consumption • Colchicine • NSAIDs • Allopurinol- ***common med • Low purine diet • Decrease alcohol consumption Fibromyalgia • Chronic fatigue • Generalized muscle aches • Stiffness Management of Fibromyalgia • NSAIDs • Tricyclic antidepressants- for pain and to promote sleep • Individualized exercise plans • Support/encouragement Infectious Arthritis ***Infection in the joint space- joint can “shed” and get into blood system Med emergency. Stabilize joint. • Common cause: • Neisseria gonorrhoeae • Staph Aureus • Streptococci • Acute onset • Warm, swollen, painful joint • C&S of Synovial fluid • IV antibiotics • Joint drainage