The respiratory tract in the most common route of entry - PBL-J-2015
advertisement

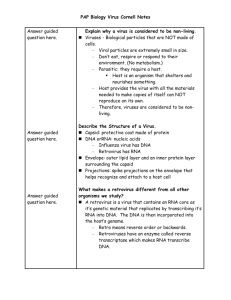
Week 5 Magic Bullets 5.3 RESPIRATORY VIRUSES 1. Outline the major groups of viruses infecting the respiratory system, including influenza, paramyxoviruses, rhinoviruses, coronaviruses and adenoviruses. Viruses are obligate intracellular parasites. The most fundamental characteristic of a virus is that it is absolutely dependent on a living host (cell) for its reproduction. Virus Family Orthomyxovirus Paramyxoviridae VIRUS Influenza A, B, C (RNA virus) Respiratory syncytial virus (RNA virus) VACCINES LOCATION AFFECTED CLINICAL SIGNS Adenoviridae Coronaviruses Adenoviruses (cause 15% (DNA virus) common colds) (RNA virus) Adults, children, elderly, immunecompromised, elderly with cardiac and respiratory problems at risk Ubiquitous: global pandemics, local epidemics. More common in winter Infants, children (most common cause of RT infection in children), adults All ages All ages coming into contact with animal carriers Ubiquitous Incidence seasonal Disease more common in early autumn, late spring Disease more common in winter, early spring Ubiquitous, no seasonal incidence Influenza A + B vaccine (annually) Antiviral drugs (eg amantadine) URT, LRT (others outside RT) No vaccines. Antiviral drugs No vaccines. Antiviral drugs for infants No vaccines Live, attenuated vaccine. Respiratory tract, most commonly LRT URT URT, LRT (also affect eye, GIT) Sore throat, cough, nasal congestion. Systemic: muscle aches, fever, chills, malaise, Most commonly in children: Bronchiolitis, pneumonia Adults: generally common cold symptoms. Mostly limited to URT, replicate in the nasopharynx Common cold, major factor in asthma exacerbations. Common cold (afebrile), SARS. Infants: associated with gastroenteritis Febrile. Bronchitis, common cold, sore throat, conjunctivitis, diarrhoea, pneumonia particles (small) eg sneezing. Widely spread by school children DISTRIBUTION OF VIRUS Coronaviridae Rhinovirus (most common cause of the common cold) (RNA virus) Inhalation of large Inhalation of aerosol droplets droplets, contact with contaminated hands TRANSMISSION Airborne RISK FACTORS Picornaviruses Inhalation of droplets, contact with contaminated hands Transmission by aerosol, close contact, faecal-oral route, or fingers and ophthalmologic instruments (eye infections) Children, day care centres, military camps, swimming clubs. Week 5 Magic Bullets 2. Identify the steps in the viral infection cycle with particular reference to infection of the respiratory epithelium. Respiratory Tract as site of entry The respiratory tract in the most common route of entry for viruses. Other common sites of entry include mucosal linings of the alimentary, and urogenital tract, the outer surface of the eye and the skin. The cell imposes multiple barriers to virus entry. Viruses must overcome the mechanical barrier of the mucosal lining. This mucosal lining traps microorganisms where they may be carrier to the back of the throat via cilia and either coughed or swallowed (digested and degraded). However, viruses exploit fundamental cellular processes to gain entry to cells and deliver their genetic cargo. Virus entry pathways are largely defined by the interactions between virus particles and their receptors at the cell surface. These interactions determine the mechanisms of virus attachment, uptake, intracellular trafficking, and, ultimately, penetration to the cytosol. Micro-organisms can avoid this by: Adhesions: specialised molecules, which enable binding to the receptor cell. The Inhibiting the action of cilia. Human Respiratory Tract Mucus layer Brush border Most transmission via the respiratory tract occurs through sneezing and coughing which allows movement of mucosal secretions. Increased nasal secretions that accompany many respiratory infections assist by increasing the number of virus carrying droplets available to transmit the micro-organism. 1. Attatchment: The virus binds to the surface of the cell through adhesions. 2. Penetration: Fusion of the viral and host membranes, or uptake via a phagosome, results in the virus carried across the plasma membrane and into the cytoplasm. 3. Uncoating: The viral envelope and/or capsid are shed and the viral nucleic acids released. At this point the virus is no longer infective. Not until the virus has replicated and exits cell. 5. Transcription and/or translation. 4. Virus replicates: Viruses contain either DNA or RNA (never both). Viruses containing DNA, mRNA can form using the host’s RNA polymerase. Viruses with only RNA must use their own RNA polymerases. 6. Assembly: Combining the replicated nucleic acid with newly synthesized capsomeres. 7. Release: Exit from the host cell. Week 5 Magic Bullets The epithelium may be left compromised. For example in a rhinovirus the DNA is replicated within the cytoplasm and exists via cell lysing instead of budding. This results in epithelial damage, and thus prone to secondary infection. This was seen in Mrs A’s case in Magic Bullets. 3. Identify the location in the respiratory system typically infected by these agents, and the clinical pattern invoked. Upper Respiratory Infections: Common Cold, Sinusitis, Pharyngitis, Epiglottitis and Laryngotracheitis. Most upper respiratory infections are of viral aetiology. Common Cold Aetiology: Common colds are the most prevalent entity of all respiratory infections. Rhinoviruses are the most common pathogens. Coronaviruses, Parainfluenza viruses, respiratory syncytial virus, adenoviruses and influenza viruses have all been linked to the common cold. Pathogenesis: direct invasion of epithelial cells of the respiratory mucosa, but destruction and sloughing of these cells or loss of ciliary activity depends on the specific organism involved. There is an increase in both leukocyte infiltration and nasal secretions. Clinical Manifestations: After an incubation period of 48-72 hours, classic symptoms of nasal discharge, obstruction, sneezing, sore throat and cough. Myalgia and headache may also be present. Fever is rare. Diagnosis: based on symptoms (lack of fever combined with symptoms of localization to the nasopharynx). Prevention/Treatment: symptomatic- decongestants, antipyretics, fluids and bed rest. Avoid infecting others, along with good hand washing, are best measures to prevent spread. Sinusitis Aetiology: Acute sinusitis is most often a secondary response to a primary URT infection of either a bacterial, viral or fungal nature. (Chronic sinusitis - lasts minimum 8 weeks, bacterial origin). Pathogenesis: Impair ciliary action of epithelial lining of sinuses, increased mucous secretions- obstruction and impedes drainage. With bacterial multiplication in the sinus cavities, the mucus is converted to mucopurulent exudates. The pus further irritates the mucosal lining causing more oedema, epithelial destruction and obstruction. Week 5 Magic Bullets Clinical Manifestations: The paranasal sinuses (commonly maxillary, ethmoid) are implicated. Pain, sensation of pressure and tenderness over affected sinus exists. Malaise and low-grade fever may occur. Diagnosis: difficult to distinguish bacterial and viral sinusitis. If resolve within 10 days most likely viral, if persist generally bacterial and antibiotics prescribed. Pharyngitis Aetiology: inflammation of the pharynx. Can be bacterial, viral (adenovirus, herpes simplex virus, EpsteinBarr virus and cytomegalovirus infections) and less commonly fungus. Pathogenesis: viral pathogens invade the mucosal cells of the nasopharynx and oral cavity, resulting in oedema and hyperemia of the mucous membranes and tonsils. Clinical Manifestations: presents with a red, sore, scratchy throat. Inflammatory exudate may cover tonsils. Vesicles or ulcers may be seen on the pharyngeal linings. Depending on pathogen, fever and systemic manifestations such as malaise, myalgia, or headache may present. Diagnosis: Serologic tests may be used to confirm due to viral, mycoplasmal or chlamydial pathogens. Prevention/treatment: symptomatic treatment for viral pharyngitis. The exception is herpes simplex virus, which can be treated with acyclovir if clinically warranted or if diagnosed in immunocompromised patients. Lower Respiratory Infections: Bronchitis, Bronchiolitis and Pneumonia. Although viruses can cause lower respiratory tract infections, most LRI are of bacterial aetiology. Bronchitis and Bronchiolitis Aetiology: respiratory syncytial virus primary cause in infants. Other viruses, including influenza viruses and adenoviruses (as well as occasionally M pneumoniae) are also implicated. Pathogenesis: Infants initially have inflammation and sometimes necrosis of the respiratory epithelium, with eventual sloughing. Bronchial and bronchiolar walls are thickened. Exudate made up of necrotic material and respiratory secretions and the narrowing of the bronchial lumen lead to airway obstruction. Clinical Manifestations: bronchiolitis presents with a cough and fever is common. A deepening cough, increased respiratory rate, and restlessness follow. Retractions of the chest wall, nasal flaring, and grunting are prominent findings. Wheezing or actual lack of breath sounds may be noted, respiratory failure and death may result. Diagnosis: Aspirations of nasopharyngeal secretions or swabs are sufficient to obtain specimens for viral culture in infants with bronchiolitis. Rapid serological diagnostic tests for antibody or viral antigens may be performed on nasopharyngeal secretions. Prevention/Treatment: Respiratory syncytial virus infections in infants may be treated with ribavirin. Pneumonia inflammation of the lung parenchyma, consolidation of lung tissue may be identified by physical examination and chest x-ray. Aetiology: viral pneumonias are rare in healthy adults (exception of pneumonia caused by influenza viruses). A serious complication following influenza virus infection is secondary bacterial pneumonia, particularly s. pneumonia. Respiratory syncytial virus can cause severe pneumonia among infants as well as among institutionalized adults. Adenoviruses may also cause pneumonia. Measles pneumonia may occur in adults. Pathogenesis and Clinical Manifestations: Infectious agents gain access to the lower respiratory tract by the inhalation of aerosolized material, by aspiration of upper airway flora, or haematogenous seeding. Pneumonia occurs when lung defence mechanisms are diminished or overwhelmed. The major symptoms or pneumonia are cough, chest pain, fever, shortness of breath and sputum production. Patients are tachycardia. Headache, confusion, abdominal pain, nausea, vomiting and diarrhoea may be present, depending on the age of the patient and the organisms involved. Microbiologic Diagnosis: Viral infection may be diagnosed by demonstration of antigen in secretions or cultures or by an antibody response, or serologic tests. Prevention/Treatment: Until organism identified, therapy based upon clinical history. Therapy is then directed at the specific organism responsible.