Bone Tissue & Joints
advertisement

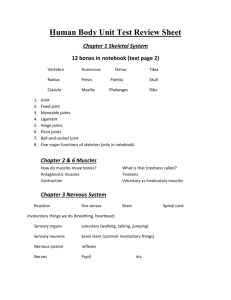
BIOL 2304 Bones and Joints The Skeletal System Functions of the Skeletal System Support against gravity Movement - leverage for muscle action Protection of soft internal organs Blood cell production Storage - calcium, phosphorous, fat The Skeletal System The skeletal system includes: Bones Cartilages Joints Ligaments Other connective tissues (CT) Tissues in Bone Bones contain several types of tissues: Primarily bone (CT) Contain nervous tissue (NT) and blood (CT) Contain cartilage (CT) in articular cartilages that articulate with other bones, forming joints Contain connective tissue proper (CT) in the form of periosteum, the outermost covering of bones Contain epithelial tissue (ET) lining blood vessels that permeate bone tissue Bone (Osseous Tissue) Bone Types: Compact Bone Dense outer layer Spongy Bone (cancellous bone) Trabeculae – honeycomb, needle-like, or flat pieces filled with bone marrow Specialized cells - 2% of bone weight Strong flexible matrix: Calcium phosphate crystals - 2/3 of bone weight Collagen fibers 3 Types of Cartilage Hyaline cartilage – Most abundant cartilage Glassy appearance Provides support through flexibility Articular cartilages and costal cartilage, larynx, trachea, and nose Elastic cartilage – Contains many elastic fibers Able to tolerate repeated bending Ear and epiglottis Fibrocartilage – Resists immense compression and tension An intermediate between hyaline and elastic cartilage Intervertebral discs and pubic symphysis General Shapes Of Bones Long bones e.g., humerus, femur Short bones e.g., carpals, tarsals, patella Flat bones e.g., parietal bone, scapula, sternum Irregular bones e.g., vertebrae, hip bones Structure of Typical Long Bone Diaphysis – tubular shaft forming the axis of long bones Composed of compact bone Central medullary cavity Contains bone marrow Epiphysis – expanded end of long bones Composed mostly of spongy bone Joint surface is covered with articular (hyaline) cartilage Epiphyseal plate (line) separates the diaphysis from the epiphyses Metaphysis – Where epiphysis and diaphysis meet Contains the epiphyseal plate (epiphyseal line) Bone Membranes Periosteum “Peri-” = around; enclosing Outermost, protective membrane Double-layered Innervated (supplied with nerve fibers) Vascularized (supplied with blood and lymphatic vessels) which enter the bone via nutrient foramina Provides anchoring points for tendons and ligaments Inner osteogenic layer is composed of osteoblasts and osteoclasts Endosteum “Endo-” = inside; internal Delicate CT membrane covering internal surfaces of bone Covers trabeculae of spongy bone Also lines canals in compact bone Also contains both osteoblasts and osteoclasts Gross Anatomy of Bones External Features of Bones: Projections and depressions for muscle, ligament, & tendon attachment Surfaces that form joints Openings as conduits for blood vessels and nerves Superficial surfaces of bones reflect stresses on them Depression & Openings Meatus – canal like passageway Foramen – round or oval opening Sinus – air-filled cavity Fissure – narrow, slit-like opening Fossa – shallow basin Facet – smooth, nearly flat articular surface Sulcus, Groove, or Furrow – shallow groove Processes (projections): Condyle – rounded, articular process Epicondyle – elevated area above condyle Head – rounded epiphysis Crest – prominent narrow ridge Line – small narrow ridge Spine – sharp, narrow, pointed end Ramus – arm like bar of bone Trochanter – large, blunt process (femur only) Tubercle – small, rounded process Tuberosity – large, rounded, rough process Histology of Compact Bone Osteon – the structural unit of compact bone Lamellae – column-like matrix tubes composed of collagen and crystals of bone salts Central canal (Haversian canal) – canal containing blood vessels and nerves Lacunae - cavities in bone containing osteocytes Canaliculi - hairlike canals that connect lacunae to each other and the central canal Perforating canal (Volkmann’s canal) – channels lying at right angles to the central canal, connecting blood and nerve supply of the periosteum to the central canal Cells in Bone Osteoprogenitor cells – precursors to osteoblasts Osteocytes - mature bone cells between lamellae Osteoclasts - bone-destroying cells, break down bone matrix for remodeling and release of calcium Source of acid, enzymes for osteolysis (the breakdown of bone) Lysosomal enzymes & HCl Calcium homeostasis (bones contain 99% of body calcium) Osteoblasts - bone-forming cells Responsible for osteogenesis (new bone) Source of collagen, calcium salts The Structure of Spongy Bone No osteons Lamellae as trabeculae Arches, rods, plates of bone Branching network of bony tissue Strong in many directions Red marrow (blood forming) spaces Short, Irregular, and Flat Bones Plates of periosteum-covered compact bone on the outside Endosteum-covered spongy bone, diploë, on the inside Diploë – the spongy bone within short, irregular, and flat bones; found between the inner and outer compact layers Have no diaphysis or epiphyses Contain red bone marrow between the trabeculae Bone Development Osteogenesis or Ossification – the process of bone tissue formation that leads to: The formation of the skeleton in embryos Bone growth until early adulthood Bone thickness, remodeling, and repair Osteolysis – active resorption of bone matrix by osteoclasts during the natural formation of health bones Bone Growth and Development Before week 8: Skeleton of embryo made of fibrous CT membranes and hyaline cartilage After week 8: Embryo undergoes ossification (converting other tissues to bone) Processes of Development: Intramembranous ossification – Bone develops from a fibrous connective tissue membrane Endochondral ossification – Bone forms by replacing hyaline cartilage; uses hyaline cartilage “bones” as patterns Intramembranous Ossification Intramembranous Ossification Forms flat bones of skull, mandible, clavicle Stem cells differentiate to osteoblasts Produces spongy bone, then compact bone An ossification center appears in the fibrous connective tissue membrane Osteoblasts secrete bone matrix within the fibrous membrane Osteoblasts mature into osteocytes Osteoblasts are trapped in the matrix they secrete The bone matrix develops into trabeculae The trabeculae formed from various ossification centers fuse with one another to create spongy bone Eventually, the spaces between trabeculae fill with red bone marrow Endochondral Ossification Endochondral Ossification Most bones formed this way Hyaline cartilage model replaced by bone Replacement begins in middle (diaphysis) Replacement follows in ends (epiphyses) Endochondral Ossification Appositional Bone Growth Growing bones widen as they lengthen Appositional growth – growth of a bone by addition of bone tissue to its surface Bone is resorbed at endosteal surface and added at periosteal surface Osteoblasts – add bone tissue to the external surface of the diaphysis Osteoclasts – remove bone from the internal surface of the diaphysis Longitudinal Bone Growth Longitudinal Growth (interstitial) – cartilage continually grows and is replaced by bone Bones lengthen entirely by growth of the epiphyseal plates Cartilage is replaced with bone as quickly as it grows Epiphyseal plate maintains constant thickness Epiphyseal Plate Cartilage is organized for quick, efficient growth 1) Chondroblasts (cartilage cells) divide quickly forming tall stacks of daughter cells Chondroblasts at the top of stacks are highly mitotic during growth periods Pushes the epiphysis away from the diaphysis Lengthens entire long bone 2) Older chondrocytes at bottom of stacks signal surrounding matrix to calcify, then die and disintegrate 3) Leaves long trabeculae (spicules) of calcified cartilage on diaphysis side Trabeculae are partly eroded by osteoclasts Osteoblasts then cover trabeculae with bone tissue 4) Trabeculae finally eaten away from their tips by osteoclasts Bone - Remodeling/Homeostasis Role of Remodeling in Support Remodeling – Continuous breakdown and reforming of bone tissue Shapes reflect applied loads Mineral turnover enables adapting to new stresses Remodeling Units – adjacent osteoblasts and osteoclasts deposit and reabsorb bone at periosteal and endosteal surfaces Bone Remodeling Bone is active tissue – small changes in bone architecture occur continuously 5 to 7% of bone mass is recycled weekly Spongy bone is replaced every 3-4 years Compact bone is replaced every 10 years What you don’t use, you lose The stresses applied to bones during exercise are essential to maintaining bone strength and bone mass Bone Remodeling Bone Deposition - the formation of new bone by osteoblasts Occurs when bone is injured or extra strength is needed Requires a healthy diet - protein, vitamins C, D, and A, and minerals (calcium, phosphorus, magnesium, manganese, etc.) Bone Resorption - the process by which osteoclasts break down bone and release the minerals Osteoclasts are multinucleate, phagocytic cells Osteoclasts secrete: Lysosomal enzymes that digest organic matrix HCl that converts calcium salts into soluble forms Dissolved matrix is removed by interstitial fluid and blood Bone - Remodeling/Homeostasis Homeostasis and Mineral Storage Bones store calcium Contain 99% of body calcium Store up to two kg calcium Hormones control storage/release PTH, calcitriol release bone calcium (through osteolysis) Calcitonin stores bone calcium (through osteogenesis) Blood levels kept relatively constant Joints Rigid elements of the skeleton meet at joints or articulations Greek root “arthro” means joint Functions of joints Hold bones together Allow for mobility Articulations can be Bone to bone Bone to cartilage Teeth in bony sockets Classification of Joints Joints can be classified by function or structure Functional: Synarthroses – immovable joints Amphiarthroses – slightly moveable joints Diarthroses – freely moveable joints Structural: Fibrous joints – generally immovable Cartilaginous joints – immovable or slightly moveable Synovial joints – freely moveable Functional Classification Functional classification – based on amount of movement Synarthroses – immovable joints Suture – very short CT fibers, e.g. between cranial bones Gomphosis – teeth in sockets Synchondrosis – hyaline cartilage unites bones, e.g. epiphyseal plate, costal cartilage of 1st rib and manubrium Amphiarthroses – slightly moveable joints Syndesmosis – bones connected by ligaments, e.g. between tibia and fibula Symphysis - bones are covered by hyaline cartilage fused with fibrocartilage, e.g. between vertebrae, pubic bones of the hip Diarthroses – freely moveable; knee, elbow, etc Classifications of Joints Structural classification based on Material that binds bones together Presence or absence of a joint cavity Structural classifications include Fibrous Cartilaginous Synovial Fibrous Joints Bones are connected by fibrous connective tissue Primarily dense regular CT Do not have a joint cavity Most are immovable or slightly movable Types: Sutures Syndesmoses Gomphoses Fibrous Joints – Sutures Bones are tightly bound by a minimal amount of fibrous tissue Only occur between the bones of the skull Allow bone growth so the skull can expand with brain during childhood Fibrous tissue ossifies in middle age Synostoses – closed sutures Fibrous Joints – Syndesmoses Bones are connected exclusively by ligaments Amount of movement depends on length of fibers Tibiofibular joint – immovable synarthrosis Interosseous membrane between radius and ulna Freely movable diarthrosis Fibrous Joints – Gomphoses Tooth in a socket Periodontal ligament – the connecting ligament Cartilaginous Joints Bones are united by cartilage Lack a joint cavity Two types: Synchondroses - hyaline cartilage unites bones Epiphyseal plates Rib and sternum Symphyses – permanent, slightly moveable fibrocartilaginous fusion between two bones The pubic symphysis Intervertebral disc between two vertebrae Synovial Joints Most movable type of joint All are diarthroses Each contains a fluid-filled joint cavity General Structure of Synovial Joints Articular cartilage Ends of opposing bones are covered with hyaline cartilage Absorbs compression Joint cavity (synovial cavity) Unique to synovial joints Cavity is a potential space that holds a small amount of synovial fluid Articular capsule – joint cavity is enclosed in a twolayered capsule Fibrous capsule – dense irregular connective tissue, which strengthens joint Synovial membrane – loose connective tissue Lines joint capsule and covers internal joint surfaces Functions to make synovial fluid Synovial fluid A viscous fluid similar to raw egg white A filtrate of blood Arises from capillaries in synovial membrane Contains glycoprotein molecules secreted by fibroblasts Reinforcing ligaments Often are thickened parts of the fibrous capsule Sometimes are extracapsular ligaments, located outside the capsule Sometimes are intracapsular ligaments, located within the capsule Structures Associated with the Synovial Joint Tendon sheath – elongated bursa that wraps around a tendon Bursae – flattened fibrous sacs Lined with synovial membranes Filled with synovial fluid Not actually part of the joint Menisci Fat pads Structural Classification of Synovial Joints Gliding (Plane joint) Example: vertebra–vertebra Hinge Example: knee Pivot Example: Atlas-axis vertebral articulation Ellipsoidal (Condyloid joint) Example: distal radius Saddle Example: thumb Ball-and-Socket Example: hip Types of Synovial Joints Based on Shape Summary of Joint Classes