Sodium Balance
advertisement

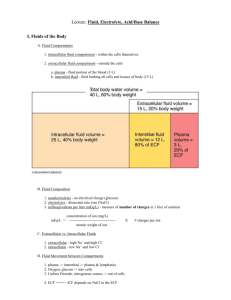
Sodium Balance Lecture Objectives: 1) Describe the effect of a change in NaCl ingestion on ECF and blood volume, plasma [Na+], GFR, aldosterone secretion rate, atrial natriuretic peptide and urodilatin secretion and urinary Na+ excretion i. The amount of sodium excretion is directly related to the amount of sodium ingestion b. Effect of INCREASE IN SODIUM INTAKE on sodium excretion and ECF volume i. When Na+ intake increases 1. GFR may increase; secretion of ANP and urodilatin increase 2. RPF increases and FF decreases a. Remember that FF = GFR/RPF 3. ECF volume increases a. Creates a Positive sodium balance to increase volume and body weight 4. Secretion of renin, Angiotensin, and aldosterone decrease 5. Serum Na+ concentration changes very little c. Effect of a DECREASE IN SODIUM INTAKE on sodium excretion and ECF volume i. When Na+ intake decreases 1. GFR may decrease; secretion of ANP and urodilatin decrease 2. RPF decreases and FF increases 3. ECF volume decreases 4. Secretion of renin, Angiotensin, and aldosterone increase 5. Serum sodium concentration changes very little d. Na+ balance influences ECF volume, blood volume, and blood pressure i. Increase in Na+ intake increased ECF Na+ and increase ECF osmolality increased ADH secretion and increased THIRST increase in H2O and ECF volume increased blood volume and blood pressure 2) Name the components of the juxtaglomerular apparatus a. JG Apparatus i. Afferent arteriole + Glomerular capillary +macula densa + thick ascending limb of loop + efferent arteriole + renal sympathetic nerves ii. Renin is synthesized mostly in the afferent arteriole smooth muscle cells 3) For these hormones, name the class of hormone they belong to (steroid or peptide) and state where they are synthesized: a. Renin – peptide hormone synthesized in the smooth muscle cells of the afferent arteriole b. Angiotensin II - Angiotensinogen is an α-2-globulin that is produced constitutively and released into the circulation mainly by the liver i. Angiotensin I is formed by the action of renin on angiotensinogen ii. Angiotensin I is converted to angiotensin II through removal of two terminal residues by the enzyme Angiotensin-converting enzyme (ACE, or kinase), which is found predominantly in the capillaries of the lung c. Aldosterone - The corticosteroids are synthesized from cholesterol within the adrenal cortex i. Aldosterone acts at the Principal Cells of the collecting duct to: 1. Increase permeability of Na+ - fast 2. Increase synthesis of Na+, K+, ATPase -slow 4) 5) 6) 7) 8) 9) 10) 11) 12) d. Atrial natriuretic peptide - ANP is produced, stored and released by cardiac myocytes of the atria of the heart. i. It is released in response to atrial stretch and a variety of other signals induced by hypervolemia, exercise or caloric restriction e. Urodilatin - hormone that causes diuresis through increasing renal blood flow. i. It is secreted in response to increased mean arterial pressure and increased blood volume from the cells of the distal tubule and collecting duct Name the organ where renin substrate (angiotensinogen) is synthesized a. Angiotensinogen is synthesized in the LIVER Explain the function of converting enzyme a. ACE – b. The rate limiting step in the production of angiotensin II is the rate of renin secretion List 4 effects of Angiotensin II on sodium and water balance a. Brain – thirst, increase in drinking increase in blood volume b. Adrenal Cortex – increase in aldosterone secretion increase in Na+ reabsorption c. Arteriolar vasoconstriction – increase in filtration fraction increase in Na+ reabsorption d. Proximal Tubule - increase in Na+ reabsorption i. Angiotensin II stimulates Na+, H+ antiport in the proximal tubule and loop of Henle, increasing Na+ & HCO3- reabsorption Diagram the pathways showing the effect on renin secretion of changes in blood volume, arterial blood pressure, or urine [Na+] a. Decrease in blood volume decrease in central venous pressure veno-atrial mechanoreceptors decrease in firing of vagus nerve CNS increase in renal sympathetic nerve activity beta-receptors on JG cells increase in renin secretion increase in angiotensin II synthesis b. Same effect would occur with a decrease in arterial pressure Describe the role of the macula densa in regulating renin secretion a. Decrease in Na+ intake decrease in BV vascular mechanoreceptors CNS increase renal nerve activity increase in proximal Na+ reabsorption decrease urine flow to the loop of henle decrease [Na+] in urine at macula densa increase in renin secretion List 3 effects of the sympathetic nerves on renal function a. Renin secretion b. Proximal sodium reabsorption c. Keeping GFR constant, decreasing renal plasma flow increase in filtration fraction Explain the mechanism regulating release of ANP into the blood a. An increase in blood volume creates an increase in central venous pressure and increased atrial filling i. The atria secretes ANP in response to decrease renin secretion List 3 effect of ANP on renal function a. Decreased renin decreased angiotensin and aldosterone decrease Na+ pump activity decrease Na+ reabsorption increase Na+ excretion b. ANP acts to vasodilate the kidney to increase GFR and RPF and decrease FF c. ANP acts to decrease sodium pump activity at the proximal tubule and collecting ducts Give the location where urodilatin is synthesized, and its effect on renal function a. Urodilatin is synthesized in the DISTAL TUBULE & CORTICAL COLLECTING DUCT in response to increases in blood pressure and ECF volume b. Urodilatin is secreted INTO the urine acts on the medullary duct to decrease NaCl and H2O reabsorption and increases their excretion 13) Explain how the shift in the renal function curve causes hypertension a. The renal function curve represents the combined effects of intrinsic pressure diuresis plus all the normal hormonal and neural influences on the kidney that affect sodium excretion b. The pressure diuresis mechanism acts as a negative feedback connecting kidney function with blood pressure i. Diuresis – increase in urine flow ii. Natriuresis – increase in Na+ excretion c. The kidney acts like a pressure release valve i. Angiotensin stimulates sodium reabsorption; its effect opposes pressure diuresis 1. The effect of angiotensin on renal function curve shifts to the right and mimics essential hypertension ---- an increase in pressure is needed to effectively filter the blood