Renal I and II
advertisement

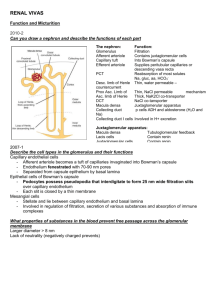
Human Physiology 11/20- 11/21/08 Jeff Weiner Renal I and II Objectives- Dr. Brand 1. Define osmolality, and give the normal value of human serum osmolality. a. Osmolality is the number of osmoles/kg of solvent. The normal plasma osmolality is 280-296 mOsm/liter 2. Describe the initial changes that occur in ICF and ECF osmolality and volume in response to deficits or excesses of water or NaCl. a. Deficit of water: Water is lost from both ICF and ECF, osmolality will increase equally, and the volumes of both compartments will decrease b. Excess water: Water will distribute through all body fluid compartments and distributes passively according to the osmotic gradient c. Loss of NaCl: NaCl is is lost from ECF, and ECF osmolality decreases. Water will move along osmotic gradient from ECF to ICF. Movement of water into ICF decreases ICF osmolality d. Ingested NaCl: Initially retained in ECF. Water moves along osmotic gradient from ICF to ECF, and the osmolality of total body water increases 3. Describe the effect of afferent arteriolar constriction on GFR and renal blood flow. a. Sympathetic vasoconstriction decreases renal blood flow, glomerular capillary hydrostatic pressure & glomerular filtration rate (GFR) 4. Describe the changes that occur on GFR and renal blood flow with increased sympathetic nerve activity. a. Sympathetic vasoconstriction decreases renal blood flow, glomerular capillary hydrostatic pressure & glomerular filtration rate (GFR) 5. List the percentage of the filtered load of Na+ and water reabsorbed in the proximal tubule, descending and ascending limb of loop of Henle, and the distal tubule and collecting duct. a. % reabsorption of NaCl and water along the nephron NaCl H2O Proximal tubule 67% 67% Descending limb Zero 15% Thick ascending limb 25% Zero Distal tubule and collecting duct 7% ~17% Totals 99% 99% 6. Describe the cellular mechanism for reabsorption of Na+ in the proximal tubule. a. Sodium is taken in through the brush border to the proximal tubule via cotransport or countertransport. The Na/K ATPase will pump the sodium into the interstitial fluid between the nephron and the capillary. Oncotic and hydrostatic pressure will move sodium into the capillaries. 7. Define these terms: primary active transport, secondary active transport, cotransport, and counter transport. a. Primary active transport: mechanism that uses ATP to directly transport a particle across a membrane Human Physiology 11/20- 11/21/08 Jeff Weiner b. Secondary active transport: ATP is used to transport an ion and create a gradient. This gradient will act to transport another type of ion via a symport (example is sodium/glucose symport) c. Cotransport: Form of secondary active transport in which net movement of actively transported substance and “downhill” movement of molecule supplying the energy are in the same direction d. Countertransport: Form of secondary active transport in which net movement of actively transported substance and “downhill” movement of molecule supplying the energy are in the opposite direction 8. Explain the mechanism that is responsible for reabsorption of glucose, lactic acid and amino acids in the proximal tubule. a. These substances use a secondary active transport (symport system) to be reabsorbed into the proximal tubule. 9. Describe the cellular mechanism of Na+ and Cl- reabsorption in the thick portion of the ascending limb of the loop. a. NaCl reabsorption occurs via a Na, K, 2Cl symport energized by passive diffusion of Na from lumen to cell b. K exhibits secondary active symport with Na. c. Loop diuretics are competitive inhibitors of the symport mechanism d. Thick ascending limb is NOT permeable to water under any conditions 10. Describe the effects of aldosterone on renal Na+ reabsorption. a. Na transport is stimulated by aldosterone i. Short term: (45 minutes) increase in luminal permeability to Na and K ii. Long term: (hours) increase in synthesis of Na/K ATPase 11. Name the major effect of ADH (anti-diuretic hormone, vasopressin) on the cortical and medullary collecting ducts. a. Principal cells of the cortical and medullary collecting duct have K+ secretion and water permeability regulated by ADH. ADH will insert H2O channels in luminal membrane, increasing water permeability is. 12. Describe the effects of a change in NaCl ingestion on ECF and blood volume, plasma [Na+], GFR, aldosterone secretion rate, atrial natriuretic peptide and urodilatin secretion and urinary Na+ excretion. a. GFR may increase, secretion of ANP and urodilatin increase b. Renal blood flow may increase c. ECF volume increases d. Secretion of renn, angiotensin, and aldosterone decrease e. Serum Na concentration changes very little 13. Describe the juxtaglomerular apparatus & state where renin is synthesized and stored. a. The juxtaglomerular apparatus functions as a sodium sensory apparatus. Renin is synthesized and stored in the vascular smooth muscle cells, and secreted directly into the blood from these cells. 14. Describe the function of converting enzyme. a. Angiotensin Converting Enzyme (ACE) converts angiotensin I to angiotensin II 15. Describe the effects of angiotensin II on arterioles, aldosterone secretion and + Na transport in the kidney. Human Physiology 11/20- 11/21/08 Jeff Weiner a. Angiotensin II will cause arteriolar vasoconstriction (mostly efferent arterioles), will cause an increase in aldosterone secretion, and an overall increase in sodium reabsorption from the urine 16. Diagram the pathway whereby renin secretion changes in response to changes in blood volume or blood pressure. a. A drop in blood pressure or blood volume will be detected by baroreceptors (atria/vena cava) and relayed to the brain stem, which activates renal sympathetic nerves. These nerves act through the juxtaglomerular cells to increase renin secretion 17. Describe the role of the macula densa in regulating renin secretion. a. Decreased sodium transport at the macula densa will act on the juxtaglomerular cells to increase renin secretion 18. Tell how the renal nerves influence renal tubular Na+ reabsorption. a. Increase in renal nerve activity will act directly and indirectly to increase reabsorption i. Direct: Will increase proximal Na/K ATPase which increases reabsorption ii. Indirect: Will cause vasoconstriction which lowers GFR and acts to decrease NaCl and H2O excretion. Also, an increase win renal nerve activity will increase renin secretion, increasing angiotensin II and causing an increase in sodium reabsorption 19. Give the location where atrial natriuretic peptide (ANP) is synthesized, and tell what stimulates its secretion into the blood. a. ANP is synthesized, stored, and released by the cardiac myocytes of the atria of the heart. An increase in atrial filling (from a rise in central venous pressure due to rise in blood volume) will lead to an increase in secretion of ANP 20. List the effects of ANP on GFR, Na+ excretion, and aldosterone secretion. a. ANP will increase renal vasodilation, which will increase GFR b. ANP will lower renin secretion, thereby lowering angiotensin II production and lowering aldosterone secretion c. These factors, combined with the fact that ANP directly acts on the proximal and distal tubule to lower Na reabsorption, will combine to increase Na+ excretion 21. Tell where urodilatin is synthesized, and give its effects on renal function. a. Urodilation is synthesized in the distal tubule. It acts on the medullary collecting duct to lower NaCl & H2O reabsorption and increase excretion. 22. Name the site where ADH is synthesized, stored and released into the blood. a. ADH (Vasopressin) is synthesized in the surpaoptic nucleus b. It is stored in the posterior pituitary gland. c. It is released into capillaries perfusing the gland. 23. Describe the effects of changes in plasma osmolality, blood volume or blood pressure on ADH secretion. a. Increase in plasma osmolality will cause an increase in CSF sodium, which will cause an increase in ADH secretion. b. Drops in blood volume and arterial blood pressure will also cause a release of ADH 24. Describe the effects of changes in plasma [ADH] on renal water excretion and urine osmolality. Human Physiology 11/20- 11/21/08 Jeff Weiner a. A rise in plasma ADH will cause the urine to be more concentrated (two slides on page 26). Water excretion is lowered, and ADH increases permeability of the medullary collecting ducts to H2O 25. Describe the effects of changes in K+ intake on plasma [K+] and body K+ content. a. An increase in K intake will cause an increase in plasma K and an increase in body K. This will stimulate aldosterone, which will increase Na/K pump and K channel production, and increased secretion of K to the urine 26. Describe the cellular mechanism for secretion for secretion of K+ by the Principal cells of the distal tubule. a. The Na/K pump will bring plasma potassium into the Principal cell. The K+ channel will then allow potassium to passively diffuse into the urine. This process is stimulated by increased plasma potassium concentration and aldosterone, and is driven by intra/extracellular charges 27. Describe the effect of aldosterone on renal K+ secretion and excretion. a. Aldosterone increases renal potassium secretion and excretion 28. List the main extracellular and intracellular buffers. a. Intracellular: H2CO3 (acid) and HCO3- (base) b. Intracellular: Proteins and organic phosphates i. Proteins contain carboxyl groups that act as proton donors or acceptors, and phosphates may act as proton donors or acceptors 29. Name the primary acid base imbalances and describe the changes in serum bicarbonate concentration and PCO2 that occur in each type of imbalance. Disorder Primary Defect Buffering Compensation Metabolic acidosis Inc. H+ production ECF HCO3Hyperventilation ICF protein, phosphate Respiratory acidosis Inc. PCO2 ICF proteins, organic phosphates Increased HCO3generation Metabolic alkalosis Inc. HCO3production Increased lactic acid synthesis (minor) Hypoventilation Respiratory alkalosis Lower PCO2 Increased lactic acid synthesis (minor) Increased HCO3excretion 30. Describe the renal response to each of the four primary acid-base distributions. a. Metabolic acidosis: Excess H+ production causes a drop in serum pH, and an increase in HCO3- synthesis by the kidney to stabilize ECF [HCO3-] b. Respiratory acidosis: Rise in arterial PCO2 causes a drop in serum pH, and the same renal response as in metabolic acidosis c. *Metabolic alkalosis: No renal response listed in notes, just the hypoventilation compensation is mentioned d. Respiratory alkalosis: Renal compensation is to decrease HCO3- reabsorption and increase HCO3- excretion, which will lower serum HCO3-