learning guide for physical examination of adult respiratory patient
advertisement

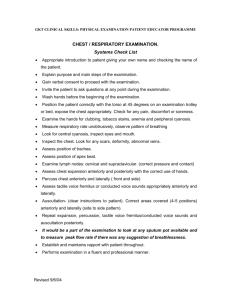
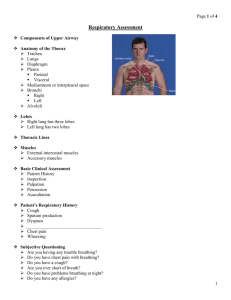
RESPIRATORY PHYSICAL EXAMINATION IN ADULTS Arto Yuwono, dr.,SpPD-KP,FCCP,FINASIM Yana Akhmad, dr., SpPD-KP,FINASIM Prayudi Santoso, dr., SpPD-KP,FCCP,FINASIM,M.Kes I. II. GENERAL OBJECTIVE After completing skill practice, the student will be able to perform respiratory physical examination. SPECIFIC OBJECTIVE At the end of skill practice, the student will be able to perform the procedure of respiratory physical examination systematically including: Systematic physical examination of respiratory system by performing inspection, palpation, percussion and auscultation III. SYLLABUS DESCRIPTION 3.1 Sub Module Objective After finishing skill practice of clinical examination, the student will be able to perform physical examination of respiratory disorders 3.2 Expected competencies Student will be able to demonstrate the procedure of respiratory disorders 3.3 Method a. Presentation b. Demonstration c. Coaching d. Self practice : role-play 3.4 Laboratory facilities a. Skills laboratory: table, chairs, and examination couch b. Trainers c. Patient: real patient and model d. Student learning guide 3.5 Venue Skills laboratory A5.1 3.6 Evaluation a. Point nodal evaluation b. OSCE 3.7 Sub Model Objective After finishing skill practice of clinical examination, the student will be able to perform respiratory system physical examination. 3.8 Expected Competencies Student will be able to demonstrate the procedure of physical examination of: - Locating Cervical lymph node - Tracheal position - Locating chest abnormalities vertically and circumferentially - Shape and movement of the chest - Tactile fremitus - Chest Percussion Normal breath sounds Presence and absent of adventitious sounds Presence and absent of transmitted voice sounds (bronchophony, egophony and whispered pectoriloquy) LEARNING GUIDE FOR PHYSICAL EXAMINATION OF ADULT RESPIRATORY PATIENT No I 1 2 3 4 II A B C D Step / Task PREPARATION Greet client respectfully and with kindness. Tell the patient what is going to be done Help the patient on to the examination table Wash hands thoroughly with soap and water and dry with a clean dry cloth or air drier The examiner should stand at the patient’s right side EXAMINATION TECHNIQUE General Physical Examination (described elsewhere) Locating Cervical Lymph Nodes 1. Make the patient comfortable and relax 2. Flexed the neck slightly forward and if needed slightly toward the examination 3. Palpate using the pads of your index and middle fingers 4. Move the skin over the underling tissue in each area 5. Describe location, quantity, size (diameter), consistency, movability, presence specific formation (package). Findings : 1. Preauricular – in front of the ear 2. Posterior auricular – superficial to mastoid process 3. Occipital – at the base of the skull posteriorly 4. Tonsilar – at the angle of mandible 5. Submandibular – midway between the angle and the tip of the mandible. These nodes are usually smaller and smoother than lobulated submandibular gland against which they lie 6. Submental – in the midline a few cm behind the tip of mandible 7. Superficial cervical – superficial to sternomastoid 8. Posterior cervical – along the anterior edge of trapezius 9. Deep cervical chain – deep to the sternomastoid and often inaccessible to examination. Hook your thumb and fingers around either side of the sternomastoid muscle to find them 10. Supraclavicular – deep in the angle formed by the clavicle and the sternomastoid TRACHEA 1. Inspect trachea for any deviation from its midline position. 2. Place the finger along one side of the trachea and note the space between trachea and the sternomastoid. 3. Compare it with the other side. Normally the space should be symmetrical. Locating Chest abnormalities To locate vertically Anterior chest 1. Identify the suprasternal notch 2. Move your down about 5 cm 3. Find the horizontal bony ridge that join the manubrium to the body of sternum. 4. Move your finger laterally and find the adjacent 2nd rib and costal cartilage Performance Scale 1 2 3 5. From here you can walk down the interspaces. 6. The first intercostals space below the 2nd rib is the second intercostals space. Posterior chest 1. Flexed the patients neck forward 2. Find the most prominent process 3. The most prominent is the C7 4. When two process appear equally prominent they are C7 and T1 5. Then you can felt and counted the process below them 6. You can also estimating location from location of inferior angle of scapula is usually leis at the level of the 7th rib of interspace. To locate findings around the circumference of the chest 1. midsternal and vertebral are lines drops vertically mid sternal and midvertebral 2. Identify both end of the clavicle and the midclavicular line drops vertically from the mid point of clavicle. 3. Anterior and posterior axillary lines drop vertically from the anterior and posterior axillary folds 4. The midaxillary line drops from the apex of the axilla TECHNIQUES OF CHEST EXAMINATION : Examine the anterior chest Inspection 1. place the patient in supine position 2. your position is in the midline position in front of the patient 3. inspect the shape of the chest and the way in which it moves 4. findings : deformities or asymmetry, abnormal retraction of interspace during inspiration, impairment of respiratory movement on one or both side or a unilateral lag (delay) in the movement. Palpation Test respiratory expansion 1. place your thumb about at the level of and parallel to the 10th ribs, your hands grasping the lateral rib cage. 2. Slide your hand medially a bit in order to raise loose skin folds between your thumb and the spine. 3. ask the patient to inhale deeply 4. Watch the divergence of your thumbs during inspiration and feel for the range and symmetry of respiratory as the thorax expands and feel for the extent and symmetry of respiratory movement. Tactile fremitus a. use either the ball (the bony part of the palm at the base of the fingers) or the ulnar surface of your hand and place it in both side of the chest symmetrically b. ask the patients to repeat the words “ninety nine” or “one – one – one” c. repeat this examinations in other areas of the chest symmetrically Percussion 1. hyperextend the middle finger of your left hand (the pleximeter finger) 2. press its distal interphalangeal joint firmly on the surface to be percussed. 3. AVOID contact by any other part of the hand 4. Position your right forearm quite close to the surface with the hand cocked upward. The right middle finger should be partially flexed, relaxed, and poised to strike 5. Strike the pleximeter finger with the right middle finger (the plexor), with a quick, sharp but relaxed wrist motion 6. Aim the strike at your distal interphalangeal joint. 7. Learn to identify five percussion notes which can be distinguished by differences in their basic qualities of sound : intensity, pitch and duration. Auscultation 1. instruct the patients to breath deeply through an open mouth 2. listen to breath sound with the diaphragm of your stethoscope 3. move your stethoscope from one side to the other and comparing symmetrical areas of the lung 4. pattern of breath sound identified by their intensity, pitch, and relative duration of their inspiratory and expiratory phases 5. the normal breath sounds are : vesicular, bronchovesicular and bronchial 6. listen for any added or adventitious sound that are superimposed on the usual breath sound. Adventitious sounds are crackles (rales), wheezes and rhonchi 7. if you hear crackles, listen for the following characteristics a. loudness, pitch and duration (summarized as fine or coarse crackles) b. number (few to many) c. timing in respiratory cycle d. location on the chest wall e. persistence of their pattern from breath to breath f. any change after a cough or a change in the patients position 8. if you hear wheeze or rhonchi , note their timing and location and do they change with deep breathing or coughing 9. if you hear abnormally located bronchovesicular or bronchial breath sound, continue on to asses transmitted voice sound. 10. With stethoscope, listen in symmetrical areas over the chest, as you : g. ask the patient to say “ninety nine”. Normally the sound transmitted through the chest wall are muffled and indistinct. Louder and clearer voice sounds are called bronchophony h. ask the patient to sal “ee” you will normally hear a muffled long E sound. When “ee” is heard as “ay”. An E to A change (egophony) is present. i. Ask the patient to whisper “ninety nine” or “one – two – three “. The whispered voice is normally heard faintly and indistinctly. Louder, clearer whispered sounds are called whispered pectoriloquy TOTAL Note: 0 = not doing at all 1 = do the step partially 2 = do the step completely