Everolimus in combination with Exemestane in hormone
advertisement

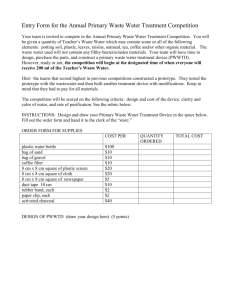
[P5-19-02] Everolimus in combination with exemestane in hormone receptor-positive locally advanced or metastatic breast cancer (BC) patients progressing on prior non-steroidal AI (NSAIs): Ballet study (CRAD001YIC04) Jerusalem G, Mariani G, Ciruelos EM, Martin M, Tjan-Heijnen VCG, Neven P, Gavila Gregori J, Michelotti A, Montemurro F, Lang I, Mardiak J, Naume B, Camozzi M, Lorizzo K, Brenski D, Conte P. CHU Sart Tilman Liege and Liege University, Liege, Belgium; Fondazione IRCCS Instituto Nazionale dei Tumori, Milan, Italy; University Hospital 12 de Octubre, Madrid, Spain; Hospital General Universitario Gregorio Marañón, Madrid, Spain; Maastricht University Medical Centre, Maastricht, Netherlands; KU Leuven and University Hospital Leuven, Leuven, Belgium; Fundacion Instituto Valenciano de Oncologia, Valencia, Spain; Azienda Ospedaliera Universitaria Pisana, Santa Chiara Hospital, Pisa, Pisa, Italy; Fondazione del Piemonte per l'Oncologia, Institute of Candiolo Cancer Center (IRCCs), Candiolo (Torino), Italy; National Institute of Oncology, Budapest, Hungary; National Cancer Institute, Bratislava, Slovakia (Slovak Republic); Oslo University Hospital and Norwa and K.G. Jebsen Center for Breast Cancer Research, Institute for Clinical Medicine, University of Oslo, Oslo, Norway; Novartis Farma S.p.A., Origgio/VA, Italy; Istituto Oncologico Veneto IRCCS and Università di Padova, Padova, Italy Background: Despite progress, a large number of breast cancer patients experience metastatic relapse and death. Hyperactivation of the mTOR pathway has been observed in patients (pts) with BC progressing on endocrine therapy. The BOLERO-2* trial demonstrated significant doubling of PFS obtained via dual blockade with everolimus (EVE) and exemestane (EXE), versus EXE alone in pts refractory to NSAIs. Methods: BALLET is a European multi-center open-label, single-arm, expanded-access study to evaluate the safety of EVE (10 mg/day) and EXE (25 mg/day) in postmenopausal women with hormone receptorpositive HER2 negative locally advanced or metastatic BC progressing on prior NSAIs. Study treatment continued until disease progression, unacceptable toxicity, death, drug locally reimbursed, discontinuation from the study for any other reason or last patient last visit (June 30th, 2014), whichever occurred first. Here we report an ad hoc-analysis that includes all pts recruited from May 12th 2012 till Dec 31st 2013 with cut-off date March 17th 2014 (final database will be available on October 31st 2014). Results: 2.133 pts were recruited in 269 sites across 14 European countries. Baseline characteristics were median age: 64 yrs; PS (ECOG) 0/1/2: 64%/30%/3%; median time from first diagnosis: 8 yrs; Stage IV pts: 99%. At the data cut off, a total of 1795 pts (84%) had discontinued the treatment. Reasons for discontinuation were: disease progression (38%), drug reimbursement (35%), adverse events (15 %), consent withdrawn (4%), death (1.5%) and others (6.5%). EVE and EXE were administered as first line treatment in 10% of pts, as second line in 23%, as third line in 22% and as fourth line or beyond in 45% of pts. 74% of pts received more than 1 line of chemotherapy in the metastatic setting. 80% of pts experienced at least one adverse event (AE) referred by the investigators as related to EVE [45% stomatitis, 7% non-infectious pneumonitis (NIP)]. The most frequent grade 3-4 drug related AEs were stomatitis (8.9%), asthenia (3.2%), GGT increase (2.4%), hyperglycemia (2.4%), and NIP (1.8%).The median time to onset of stomatitis and NIP was 3-4 weeks and 2-3 months respectively. Conclusions: These results confirm that the combination of EVE + EXE is a tolerable treatment in a real world setting even in pts more heavily pretreated by chemotherapy compared to BOLERO 2. The better understanding of side effects leading to treatment discontinuation in this large European study where investigators frequently administered the drug for the first time, will allow defining priority actions for better management of side effects including patient education and early interventions. Longer follow up with mature data (expected in October 2014) will give additional information on the safety profile, stratified by line of treatment. * Everolimus in Postmenopausal Hormone- Receptor–Positive Advanced Breast Cancer. J. Baselga et al, NEJM 2012. Friday, December 12, 2014 5:00 PM