File - Anna E. Marshall MSN Portfolio
advertisement
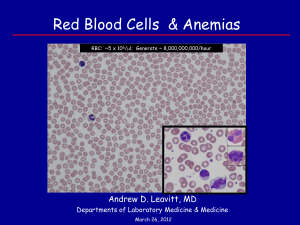
Anna Marshall NU 506- Case study 3 Anemia Henry is 77 years old and lives with his daughter and son-in-law. He has chronic renal failure, but likes to get out whenever he can to work in his daughter’s back yard garden. Over the last few months he began to go outside less often. He said he was feeling unusually tired and he was running out of breath doing the simplest of tasks. He also said his head ached and he often felt dizzy. His daughter took him to his doctor, who performed a complete physical examination and diagnosed Henry with anemia. 1. From what you know of Henry’s history, what type of anemia do you suspect he has? Explain your answer, and include a brief description of how Henry’s red blood cells would appear on a peripheral blood smear. Based on his history, I suspect that Henry has iron deficiency anemia related to chronic disease. Anemia almost always results from chronic renal failure (CRF), and is primarily due to a deficiency of erythropoietin, the hormone that controls red blood cell (RBC) production. The kidneys are the primary site for production of erythropoietin, the hormone that controls RBC production, with 89-95% of erythropoietin being formed in the kidneys. In renal failure, erythropoietin production is insufficient to stimulate adequate RBC production by the bone marrow. Other factors include unidentified uremic toxins and retained nitrogen that interfere with the actions of erythropoietin and with RBC production and survival. Other factors in addition to bone marrow suppression due to retained uremic factors, may be the chronic blood loss and hemolysis associated with hemodialysis and bleeding tendencies. On a peripheral blood smear, Henry’s blood would most likely contain fewer numbers of RBCs than normal, the RBCs would probably be microcytic (small) and hypochromic (light-colored), and exhibit poikilocytosis (irregular shape), and anisocytosis (irregular size) (Porth & Matfin, p.292, 864). 2. Describe the physiological basis that would explain why Henry’s anemia would cause him to have the symptoms he is experiencing. Hemoglobin (Hgb) is an efficient carrier of oxygen (O2); about 98-99% of O2 in the blood chemically combines with Hgb in red blood cells (RBCs) for transport. The Hgb molecule is composed of four polypeptide chains with an iron-containing heme group. Specifically O2 binds to the iron atom, and each Hgb molecule can bind four molecules of oxygen (O2) when it is fully saturated. Iron is needed for heme synthesis, and a lack of iron leads to a decrease in hemoglobin (Hgb) synthesis and smaller than normal amounts of hemoglobin in RBCs. With decreased levels of Hgb, there is impaired oxygen delivery, and manifestations of hypoxia are seen. In Henry’s case, it is the impaired oxygen delivery that is causing his symptoms: feeling unusually tired, short of breath from doing simple tasks, having a head ache, and often feeling dizzy. 3. Predict the cellular adaptations erythrocytes undergo when chronic hypoxia is present. How would this be evident on an oxygen-hemoglobin dissociation curve? Any condition that causes changes in the metabolic needs of the tissues, such as hypoxia, causes changes in Hgb’s affinity for O2. Erythrocytes, (RBCs) rely on glucose and the anaerobic glycolytic pathway for their metabolic needs. In hypoxia, increased tissue metabolism causes reduced affinity of Hgb for O2, allowing O2 to be released to the tissues to participate in tissue metabolism. RBCs also contain a metabolic intermediate called 2,3-diphosphoglycerate (2,3-DPG) that affects the affinity of Hgb for O2. The 2,3-DPG binds to the hemoglobin (Hgb) molecule and decreases the affinity of Hgb for oxygen (O2), facilitating the release of O2 at tissue levels. An increase in the concentration of 2,3-DPG enhances unloading of O2 from Hgb at the tissue level; conditions that increase 2,3-DPG include hypoxia, and chronic lung disease. The S-shaped oxygenhemoglobin dissociation curve has a flat top portion representing binding of O2 to Hgb in the lungs and a steep portion representing its release into the tissue capillaries. The S shape of the curve reflects the effect that O2 saturation has on the conformation of the Hgb molecule and its affinity for O2. The reduced affinity of the Hgb for O2 at any given partial pressure of oxygen (PO2) in the blood is reflected by a shift to the right in the dissociation curve. Caused by conditions that reflect increased tissue metabolism, such as chronic hypoxia, a shift to the right indicates that the tissue PO2 is greater for any given level of Hgb saturation and represents reduced affinity of the Hgb for O2 at any given partial pressure of oxygen (PO2) in the blood (Porth & Matfin, p. 661).