Anemias Presentation

Red Blood Cells & Anemias
RBC: ~5 x 10 6 / m l; Generate ~ 8,000,000,000/hour
Andrew D. Leavitt, MD
Departments of Laboratory Medicine & Medicine
March 26, 2012
Outline – topics we will cover
Erythropoiesis – names, faces, & numbers (review)
RBC biology Hemoglobin
O
2 dissociation curves
Hemoglobin – fetal, adult
RBC membrane
Hemoglobin switching
Anemias: Production vs. destruction vs. loss
Membrane or contents – Hgb, enzymes
Immune mediated
Physical destruction
Anemia of inflammation
Ribosomopathies
Erythropoiesis
Pro-
Erythroblast
Basophilic
Erythroblast
Polychromatic
Erythroblast
Orthochromatic
Erythroblast Reticulocyte RBC
CHROMATIN STRUCTURE
5 stages in the marrow
NUCLEAR SIZE & COLOR
Red Blood Cell (RBC)
Delivers O
2
Takes CO
2 from your lungs to all your tissues from your tissues to your lungs
Also – binds NO (a vasodilator)
Their size: 8 m [capillaries have ~3 m M diameter]
Their life-span: 120 days
Mature RBCs have no nucleus
Too few RBCs = anemia
What tells your body to make RBCs?
EPO:
Is not stored, but expressed in response to the kidney sensing oxygen in the blood
It -
1. Increases # of E-committed progenitors
2. Increase GATA1 and FOG expression
3. Enhances anti-apoptotic gene expression
4. Increases transferrin receptor expression
Hemoglobin
Hemoglobin (Hgb) in the RBC carries O
2
CO
2 from tissues to lungs.
, which is poorly soluble in water, to tissues &
~640,000,000 Hemoglobin molecules/RBC b
6
Glu to Val
Heme
Iron in a Porphyrin ring
Tetramer of two heterodimers ( a
& b
)
Must coordinate: 1.heme and globin synthesis
2. a (Chromosome 11; 141 aa)
& b (Chromnosome 16; 146) chains
Colors of a bruise are globin breakdown products
Linus Pauling
1949 – molecular diagnosis
2012 – no therapy
Hemoglobin oxygen dissociation curve
O
Arterial
2 tension
HbF
; CO
2
Mean Venous
O
2 tension
50
Erythropoiesis: Hemoglobin Switching
(ALWAYS: 2 alpha & 2 “beta-like” [3 ‘ b options]) a a g b
Alpha: Chromosome 16
Beta-like: Chromosome 11 e
0
Embryo z
Fetus Birth
HgF a
HgA a
2
2 g b
2
2
(75)
(25)
6 mo.
d
Adult
HgA a
HgA
2
HgF a a
2
2
2 b d g
2
2
2
(96-98)
(2-3)
(< 1)
Hoffman et al. Hematology 2000
Schematic of red cell membrane depicting proteins crucial for normal membrane mechanical strength
*
*
*mutations lead to hereditary spherocytosis
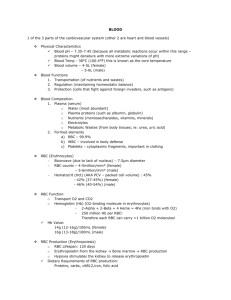
Normal Values for Hematology Tests - UCSF
Thinking about anemia…a clinical perspective
Framework:
RBC size (MCV) & is the marrow responding (reticulocyte count)
Etiology:
Cell intrinsic:
1. Hgb – too little; abnormal type; unequal a and b synthesis
2. Enzyme
3. Membrane
Cell extrinsic:
Immune mediated
Physical destruction
Blood loss
Marrow does not produce
Primary – leukemia, myelodysplasia
Secondary – vitamin deficiency
Reticulocyte Stain – detects the ribonucleoprotein in the young RBC
Reticulocytes
#1.1 Too little Hgb: Iron Deficiency Anemia
Small cells – microcytic (MCV < 80 fL)
Young women – OK
Older people – Worry about gastrointestinal blood loss normal peripheral blood (40x) Iron deficiency anemia, peripheral blood (40x)
Lead poisoning can look like Fe deficiency – Lead blocks heme synthesis
Iron Deficiency Anemia peripheral blood, 100X Iron stian of bone marrow – none found
Elliptocytes
Hypochromic
RBCs
~ 500 million people worldwide
The Iron Circuit – mostly a game of recycling
Daily absorption:
Duodenum ~ 1 mg
Transferrin
Plasma (4 mg)
Daily loss: urine, feces, skin, hair ~ 1 mg
Ineffective erythropoiesis
Bone Marrow
Erythroblasts
( ~ 150 mg)
Macrophage
(0.5 – 1.5 gm)
Circulating RBCs (1.7 – 2.4 gm)
Menstrual loss/hemorrhage
Iron Circuit in Disease
Infection/inflammation/malignancy
IL-6/LPS hepcidin (25aa protein) absorption macrophage Fe storage
Impairs Erythropoiesis:
Decrease EPO
Directly suppresses marrow
Interferon – g
TNF – a
IL-1, IL-10
Weiss & Goodnough NEJM 2005
Iron stain of bone marrow aspirates
Iron deficienyc anemia - iron stain
Anemia of inflammation – iron stain
Storage iron
(blue)
#1.2 Abnormal Hgb: Sickle cell disease
Multi-system disease
Cardiovascular/strokes
Kidneys
Skin
Lungs
Immune system
Treatment:
Supportive care
Transfusions
Demethylating agents
Stem cell transplants
#1.3 Abnormal a / b Globin ratio: Thalassemia
Small cells – microcytic (MCV < 80 fL)
Imbalance between a and b chains
Name based on which chain is deficient [ a or b thal]
Make lots of RBCs, just unstable and lyse, so increased retics
Alpha Thal: silent carrier -a / aa trait
Hgb H
-- / aa
-a / --
Hydrops fetalis -- /-or -a / -a
Beta Thal:
Minor
Intermedia
Major
50
Erythropoiesis: Hemoglobin Switching
(ALWAYS: 2 alpha & 2 “beta-like” [3 ‘ b options]) a a g b
Alpha: Chromosome 16
Beta-like: Chromosome 11 e
0
Embryo z
Fetus Birth
HgF a
HgA a
2
2 g b
2
2
(75)
(25)
6 mo.
d
Adult
HgA a
HgA
2
HgF a a
2
2
2 b d g
2
2
2
(96-98)
(2-3)
(< 1)
Hoffman et al. Hematology 2000
Normal peripheral smear Alpha thal trait
Hemoglobin H, -- / -A
Target cells
Retics
Beta-thalassemia major
Target cells
Nucleated RBC
Severe thalassemia
Beta-thalassemia major
Beta-thalassemia major (transfused)
Target cells
Normal RBCs
(transfused)
Nucleated RBC
Nucleated
RBC
#2 Enzyme: G-6-PD deficiency
(Heinz body hemolytic anemia)
Reduced glutathione (GSH) is critical for RBCs to counter oxidative stress.
Arrows show Heinz bodies
Bite cells
Sulfa drugs, fava beans, antimalarials..…
#3: Membrane: red cell membrane depicting proteins crucial for normal membrane mechanical strength
*
*
*mutations lead to hereditary spherocytosis
Hereditary spherocytosis (HS)
Reticulocytes spherocytes
Thinking about anemia…a clinical perspective
Framework:
RBC size (MCV) & is the marrow responding (reticulocyte count)
Etiology:
Cell intrinsic:
1. Hgb – too little; abnormal type; unequal a and b synthesis
2. Enzyme
3. Membrane
Cell extrinsic:
Immune mediated
Physical destruction
Blood loss
Marrow does not produce
Primary – leukemia, myelodysplasia
Secondary – vitamin deficiency
Autoimmune hemolytic anemia spherocytes
Reticulocytes
Testing for anti-RBC antibodies: attached or in circulation
Hemolytic disease of the newborn
RBC destruction - extrinsic schistocytes
(RBC fragments)
Hemolytic uremic syndrome (HUS) schistocytes
(RBC fragments)
Retics
Megaloblastic anemia (MCV > 100)
B12 deficiency
Folate deficiency
Affects DNA synthesis
Megaloblastic anemia (MCV > 100)
Anemia yet hypercellular marrow – ineffective erythropoiesis
Ribosomopathies and hematopoietic disorders
Our findings indicate that the erythroid lineage has a low threshold for the induction of p53, providing a basis for the failure of erythro- poiesis in the 5q- syndrome, DBA, and perhaps other bone marrow failure syn- dromes.
Narla & Ebert 2010
Thanks for your attention!
Take home message……
Blood is good…everyone should have some!
Share it…become a blood donor if you can
UCSF Blood donor center:
Millberry Union next to Subway sandwich shop
The best donor center nurses in town