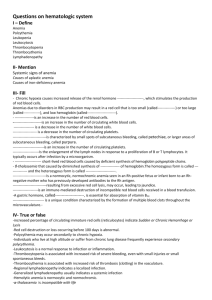
Pediatric Hematological Disorders
advertisement
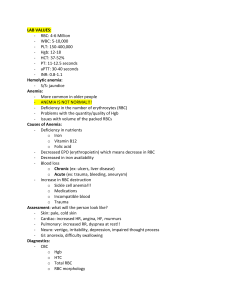
Pediatric Hematological Disorders Whaley and Wong Chapters 35, 36 Components of the Blood Blood: – Plasma • water, albumin, electrolytes, clotting factors – Cellular Components • RBCs, WBCs, Platelets • All formed in the red bone marrow (after birth) – In utero- spleen, thymus, liver • lymphatic system regulates maturation Erythrocytes RBCs – carry hemoglobin which is attached to oxygen- provides O2 to the tissues – life span 120 days – manufacture regulated by erythropoetin – Normal Hematocrit- 35-45% – Normal Hemoglobin- 12-16 grams Problems of Erythrocyte Production Anemia – reduction of RBC volume or Hgb concentration below normal Classifications: 1. Etiology/Pathophysiology – causes of RBC/Hgb depletion 2. Morphology – changes in RBC size, shape, and color Causes of Anemia Nutritional deficiency – iron, folate, B12 Increased destruction of RBCs – sickle cell anemia Impaired or decreased rate of production – aplastic anemia Excessive blood loss - hemophilia Iron Deficiency Anemia Causes - inadequate supply of iron - impaired absorption - blood loss - excessive demands for iron req’d for growth - inability for form Hgb Iron Deficiency Anemia Signs and Symptoms: due to tissue hypoxia > lack of energy, easy fatigability, pallor Diagnosis: CBC with diff, red cell indices (MCV, MCH, MCHC), iron studies, physical exam Medical Treatment: supplement with ferrous sulfate (dosages vary with age), dietary counseling Iron Deficiency Anemia Nursing Assessment and Interventions: - educate parents about nutrition - explain laboratory testing - teach parents proper administration of iron preparations, caution about high toxicity of iron Sickle Cell Anemia Causes: genetic transmission, 2 parents with the trait have 25% chance of having child with SCD, found primarily in Blacks, occ Hispanics Hgb A is partly or completely replaced by Hgb S With dehydration,acidosis, hypoxia, and temp elevations, Hgb S “sickles” Sickle Cell Anemia Pathophysiology: - vaso-occlusion from sickled RBCs - increased RBC destruction - splenic congestion and enlargement - hepatomegaly, liver failure - renal ischemia, hematuria - osteoporosis, lordosis, kyphosis - cardiomegaly, heart failure, stroke Sickle Cell Anemia Signs/Symptoms: Exercise intolerance Anorexia Jaundiced sclera Gallstones Chronic leg ulcers Growth retardation Sickle Cell Anemia Diagnosis - Sickledex - Hgb electrophoresis - Stained blood smear Vaso-occlusive crisis - mild to severe bone pain - acute abdominal pain - priapism - arthralgia Sickle Cell Anemia Medical management Supportive/symptomatic tx of crises - bed rest - hydration - electrolyte replacement - analgesics for pain - blood replacement - antibiotics - oxygen therapy Sickle Cell Anemia Nursing care: Minimize tissue deoxygenation Promote hydration Minimize crises Pain management Administering blood transfusions Encourage screening and genetic counseling Parent education Thalassemia Autosomal recessive disorder – Greeks, Italians, Syrians Signs/symptoms – microcytic anemia > splenomegaly,jaundice,epistaxis, gout Diagnosis – Hgb electrophoresis Medical Treatment – transfusions, chelation Hemophilia Factor 8 or factor 9 deficiency – prolonged bleeding any where in the body! Cause: X-linked recessive disorder, defects in platelets and clotting factors Diagnosis: history of bleeding episodes, evidence of x-linked inheritence, labs Medical Management: Factor VIII concentrate, DDAVP (vasopressin) Hemophilia Nursing care: Prevent bleeding Recognize and control bleeding (RICE) - Rest - Ice - Compression - Elevation Prevent crippling effects of bleeding Client education Idiopathic Thrombocytopenic Purpura Causes: acquired hemorrhagic disorder of unknown origin, probably an autoimmune response to disease-related antigens Diagnosis: platelet count < 20,000, abnl bleeding time and clot retraction Signs and Symptoms: petechiae, bruising, bleeding from mucous membranes, prolonged bleeding from abrasions Medical management: supportive, steroids, Anti-D antibody, splenectomy Idiopathic Thrombocytic Puerpera Nursing Considerations: Client/Parent teaching No contact sports No aspirin Prevent infection Blood Transfusion Complications: Hemolytic reactions - chills, shaking, fever - dyspnea - flank pain - progressive signs of shock Febrile reactions Allergic reactions - urticaria, flushing - wheezing Circulatory overload Blood Transfusions Nursing Care Take VS BEFORE administering blood Check ID of recipient with donor’s blood type Administer 50 mL or 1/5 volume SLOWLY – STAY WITH THE CHILD Administer with NS on piggyback set-up Use appropriate filter Use within 30 mins – infuse within 4 hrs If reaction suspected: Stop the transfusion, maintain patent IV line with NS, take VS, notify practitioner