Therapeutic Discussion – Anemia
advertisement
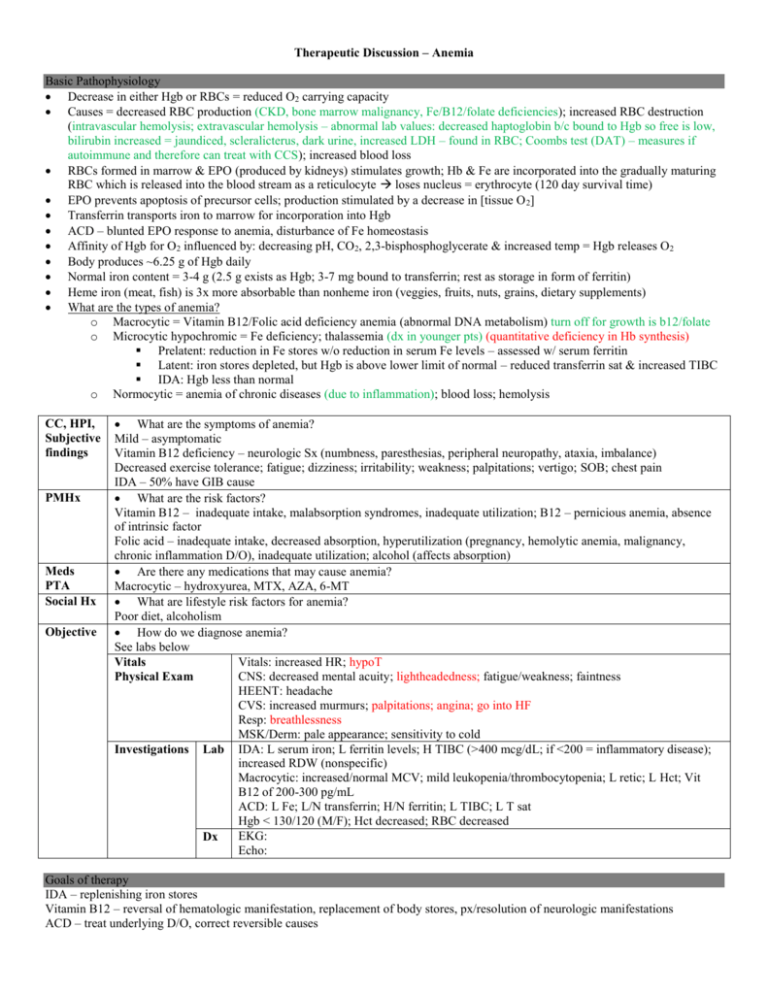
Therapeutic Discussion – Anemia Basic Pathophysiology Decrease in either Hgb or RBCs = reduced O2 carrying capacity Causes = decreased RBC production (CKD, bone marrow malignancy, Fe/B12/folate deficiencies); increased RBC destruction (intravascular hemolysis; extravascular hemolysis – abnormal lab values: decreased haptoglobin b/c bound to Hgb so free is low, bilirubin increased = jaundiced, scleralicterus, dark urine, increased LDH – found in RBC; Coombs test (DAT) – measures if autoimmune and therefore can treat with CCS); increased blood loss RBCs formed in marrow & EPO (produced by kidneys) stimulates growth; Hb & Fe are incorporated into the gradually maturing RBC which is released into the blood stream as a reticulocyte loses nucleus = erythrocyte (120 day survival time) EPO prevents apoptosis of precursor cells; production stimulated by a decrease in [tissue O 2] Transferrin transports iron to marrow for incorporation into Hgb ACD – blunted EPO response to anemia, disturbance of Fe homeostasis Affinity of Hgb for O2 influenced by: decreasing pH, CO2, 2,3-bisphosphoglycerate & increased temp = Hgb releases O2 Body produces ~6.25 g of Hgb daily Normal iron content = 3-4 g (2.5 g exists as Hgb; 3-7 mg bound to transferrin; rest as storage in form of ferritin) Heme iron (meat, fish) is 3x more absorbable than nonheme iron (veggies, fruits, nuts, grains, dietary supplements) What are the types of anemia? o Macrocytic = Vitamin B12/Folic acid deficiency anemia (abnormal DNA metabolism) turn off for growth is b12/folate o Microcytic hypochromic = Fe deficiency; thalassemia (dx in younger pts) (quantitative deficiency in Hb synthesis) Prelatent: reduction in Fe stores w/o reduction in serum Fe levels – assessed w/ serum ferritin Latent: iron stores depleted, but Hgb is above lower limit of normal – reduced transferrin sat & increased TIBC IDA: Hgb less than normal o Normocytic = anemia of chronic diseases (due to inflammation); blood loss; hemolysis CC, HPI, Subjective findings PMHx Meds PTA Social Hx Objective What are the symptoms of anemia? Mild – asymptomatic Vitamin B12 deficiency – neurologic Sx (numbness, paresthesias, peripheral neuropathy, ataxia, imbalance) Decreased exercise tolerance; fatigue; dizziness; irritability; weakness; palpitations; vertigo; SOB; chest pain IDA – 50% have GIB cause What are the risk factors? Vitamin B12 – inadequate intake, malabsorption syndromes, inadequate utilization; B12 – pernicious anemia, absence of intrinsic factor Folic acid – inadequate intake, decreased absorption, hyperutilization (pregnancy, hemolytic anemia, malignancy, chronic inflammation D/O), inadequate utilization; alcohol (affects absorption) Are there any medications that may cause anemia? Macrocytic – hydroxyurea, MTX, AZA, 6-MT What are lifestyle risk factors for anemia? Poor diet, alcoholism How do we diagnose anemia? See labs below Vitals: increased HR; hypoT Vitals CNS: decreased mental acuity; lightheadedness; fatigue/weakness; faintness Physical Exam HEENT: headache CVS: increased murmurs; palpitations; angina; go into HF Resp: breathlessness MSK/Derm: pale appearance; sensitivity to cold Investigations Lab IDA: L serum iron; L ferritin levels; H TIBC (>400 mcg/dL; if <200 = inflammatory disease); increased RDW (nonspecific) Macrocytic: increased/normal MCV; mild leukopenia/thrombocytopenia; L retic; L Hct; Vit B12 of 200-300 pg/mL ACD: L Fe; L/N transferrin; H/N ferritin; L TIBC; L T sat Hgb < 130/120 (M/F); Hct decreased; RBC decreased EKG: Dx Echo: Goals of therapy IDA – replenishing iron stores Vitamin B12 – reversal of hematologic manifestation, replacement of body stores, px/resolution of neurologic manifestations ACD – treat underlying D/O, correct reversible causes Treatment alternatives and duration IDA: Goal = 150-200 mg elemental Fe/day x 3-6 months after anemia restored o Gluconate = 35mg; green o Sulfate = 60mg; red All come as 300 mg tabs o Fumarate = 100mg; purple Parenteral iron (doesn’t lead to quicker hematologic response than PO iron) reserve for CKD pts on HD o Iron dextran anaphylaxis leading to death – need test dose; least safe; IV > IM (50mg iron/mL – max 2mL/site) o Processed by macrophages for iron to be biologically available o Slowly absorbed over months (60% after 3 days; 90% w/in 3 weeks) o Diluted in 250-1000 mL NS/D5W & infused over 4-6 hours o Sodium ferric gluconate (62.5mg/5mL) less anaphylaxis – no test dose needed o Hemodialysis patients require 1g over 8 sessions o Administered as 10 mL (125 mg Fe) in 100 mL NS over 1 hour o Iron sucrose (20mg/mL) o Hemodialysis: 100mg IV 1-3x/week (total 1000mg in 10 doses) o Dilute in NS (100mL) & infuse over 15 min Blood transfusions if Hgb <70 g/L or <90 g/L if CV history should increase Hgb by 10 Vitamin B12 1-2mg PO/IM daily; 1000mcg cyanocobalamin x 1 week, then weekly x 1 month, then monthly therafter – can switch to 1 mg PO daily (parenteral if neurologic Sx) Folic acid 1mg daily; malabsorption = 1-5 mg daily; x 4 months if underlying cause identified and corrected; 400mcg pregnant ACD: RBC transfusions; EPO (darbepoetin alfa longer t1/2 than epoetin alfa) – most evidence in CKD (target Hgb of 110); NOT in cancer pts (increases risk of thrombosis, cancer tx failure, death); DM pts with CKD not on HD – increases risk of stroke via increasing viscosity of blood; also used in Jehovah Witness; Fe only if unresponsive to EPO; NO Fe if ferritin >100 Monitoring Parameters: Efficacy and toxicity Efficacy: Fe PO: increase retics in 3-5 days (if not seen, something may be wrong in bone marrow); increase Hgb 2-4 g/dL Q3weeks (if not, may not be receiving enough Fe); ferritin will take 6 months to restore Vitamin B12: retics 2-5 days & peak at 7 days; Hgb rises after 1st week; leukocyte/platelets normalize after ~7 days Folic acid: retics 2-3 days & peaks w/in 5-8 days; Hct rises w/in 2 weeks and normal w/in 2 months EPO: retics 2-3 days; iron status; Hgb ~4 weeks, then every 2-4 weeks thereafter (max 8 weeks if no response) Safety: Fe PO: stomach upset; constipation (dose-dependent) Iron Dextran: arthralgias, myalgias, flushing, malaise, fever; staining of skin, inj site pain; allergic rxns Na Ferric Gluconate: cramps, N/V, flushing, hypotension, intense upper gastric pain, rash, pruritus Fe Sucrose: leg cramps, hypotension Vitamin B12: hyperuricemia, hypoK, fluid retention EPO: Fe deficiency; increased BP, nausea, H/A, fever, bone pain, fatigue; seizures, thrombotic events, allergic rxns, death/MI Hct = actual volume of RBCs in unit volume of blood (~3x Hgb); low = reduction in either number/size of RBCs or increase in plasma volume MCV = average volume of RBCs MCH = % volume of Hgb in RBC MCHC = weight of Hb per vol. of cells; independent of cell size therefore low = hypochromia RDW = higher means more variable size of RBCs Serum Fe = conc. of Fe bound to transferrin Iron Folate B12 Hct RBC HgB MCV MCHC RDW / Ferritin TIBC Serum Fe (diurnal -/ fluctuations) % Transferrin Saturation (0.2-0.5) Ferritin is also an acute phase reactant, therefore increased in inflammation and infections - If all labs fit IDA, except ferritin, use: CD -/ - o Ferritin/3 < 20 = IDA; > 20 = inflammation/infection Ferritin is also the most representative of iron deficiency extent (i.e. if ferritin low, Sr Fe has been used up and now stores are being depleted) T-Sat > 50%, worry about iron toxicity Hgb levels of 80 g/L associated with a doubling of the odds of death If giving blood to patient and Hgb not increasing may be due to blood loss or they may be hemolysizing it Fe absorbed in ileum (latter end of duodenum as well)